Biography
Interests
Prem James Charles1*, Selvaraj Periyasamy2 , Ashwin Narashimhaprasad3 & Sumedh Krishna Waghmare4
1Aster Specialist Centre For orthopedics and Physiotherapy, Dubai, UAE
2RALS Clinic, Al Qusais, Dubai, UAE
3Aster Clinic, Al Muteena, Dubai, UAE
4Aster Imaging Centre, Al Muteena, Dubai, UAE
*Correspondence to: Dr. Prem James Charles, Aster Specialist Centre For orthopedics and Physiotherapy, Dubai, UAE.
Copyright © 2022 Dr. Prem James Charles, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Restriction of extension of the knee joint is one of the most common complications after anterior cruciate ligament (ACL) reconstruction surgery. Impingement caused by a fibrous tissue mass related to the graft (named as cyclops lesion) has been found to be an important cause of blocking complete extension.
We present our experience of managing two cases of cyclops lesions who reported with pain and loss of knee extension after arthroscopic ACL reconstruction.
The clinical and radiological findings were suggestive of a cyclops lesion which were later confirmed during arthroscopic procedure. After a trial of physiotherapy, these patients were treated arthroscopically with shaving, radiofrequency ablation and removal of obstructing nodules which were present near the tibial insertion of ACL graft. Post-operatively, pain subsided and full range of motion was restored.
Introduction
The ACL reconstruction (ACLR) is the most commonly performed arthroscopic knee surgery. Restriction
in range of motion (ROM) of knee is one of the most frequent and challenging post-operative complications
knee surgery. Impingement of the graft and development of cyclops lesions are the two major causes found
to be mechanically blocking the motion [1].
Cyclops lesion (also known as localized anterior arthrofibrosis) is a localized fibrotic nodule developing anterior to the ACL graft at its tibial insertion [2]. This is a mass made of fibrocartilaginous tissue with leash of overlying blood vessels giving an appearance of eye of the cyclops. (1) The size of the nodule may vary from 3 X 5mm to 8 X 12mm [3].
Though primarily recognized as a complication of ACLRs, cyclops lesions can develop in ACL tears without history of reconstruction [4]. and in bicruciate sparing total knee arthroplasty (TKA) [5]. Among the ACLRs, this complication has been reported with different type of grafts including BPTB, hamstrings and fascia lata and single as well as double-bundle reconstruction [6].
Majority of lesions are asymptomatic and are found accidentally during routine post-operative MRI imaging. Clinically, the typical presenting symptoms are 1. Loss of full extension of knee, and 2. Palpable (sometimes audible) clunk at the terminal range of extension. Prior history of ACL injury or ACL surgery can be elicited. When a cyclops lesion presents with pain and extension deficit, the condition is named as cyclops syndrome [7].
MRI shows anteriorly convex soft tissue mass with low to intermediate signal intensity on T1, T2 and proton density images [8]. Normally, arthroscopic inspection confirms the diagnosis where it is visible as head-like appearance with a focal area of discoloration resembling an eye.
While majority of cyclops lesions are managed conservatively, the management of cyclops syndrome necessitates arthroscopic resection followed by physical rehabilitation therapy in order to regain normal knee movement [9].
Cases Details
Our first patient is a 27 year-old male who had undergone ACL reconstruction 6 months back. He presented
with pain and stiffness of the left knee for the last 4 weeks duration. Clinical examination demonstrated
active and passive ROM of 30 -110 degrees. There was no significant ligament laxity. He was started with
a 2-weeks course of physiotherapy focusing on knee extension. As this could not bring about the intended
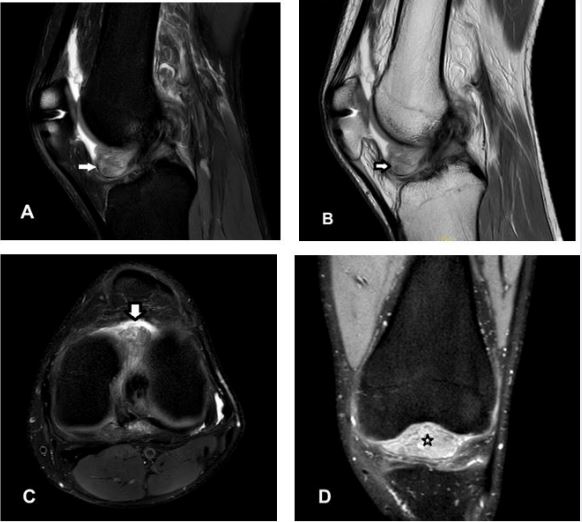
result, MRI scan was taken evaluate the cause for stiffness. A soft tissue mass lesion (Fig.1) measuring approximately 36 x 24 x 26mm in AP x TRAN x LONG dimensions was seen in the anterior aspect of
intercondylar notch anterior to the reconstructed ACL. The lesion displayed heterogeneous signal intensity
appearing heterogeneously hyperintense on PD FAT SAT and predominantly hypointense on PD and
isointense on T1 sequences.
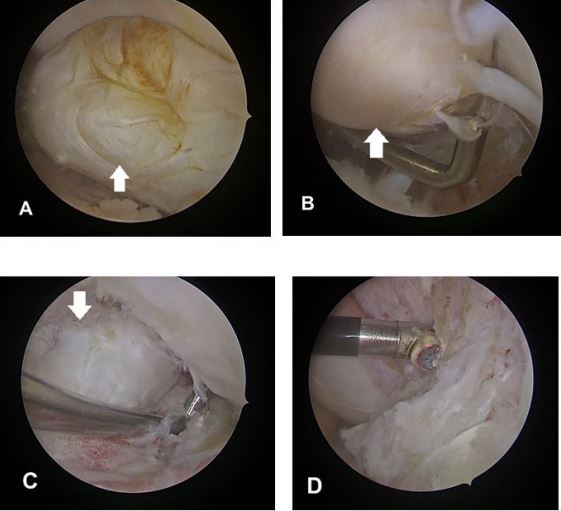
After discussion with the patient, arthroscopic excision was performed. During arthroscopy (Fig. 2), a large smooth fibrous nodule was found and mechanically obstructing the movement of knee. Other structures such as the menisci, cartilage and the reconstructed graft all appeared normal. No loose bodies were found. The nodule was excised. On follow-up after 4 weeks, he showed full extension of the knee joint.
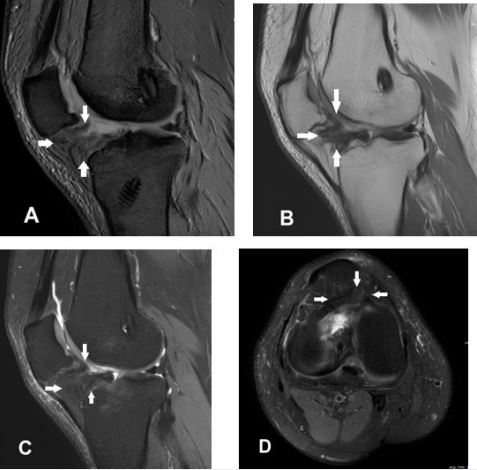
Our second patient is a 41 year old male presented with similar complaints for 2 weeks duration, 3 months after ACLR surgery. Extension of knee was not possible at 30 degrees of flexion (Fig.5 A). Two weeks of guided physical therapy yielded no significant improvement. Later, MRI (Fig.3) revealed a soft tissue fibrous mass measuring approximately 20 x 20 x 15 mm in AP x TRAN x LONG dimensions seen in the region of infra-patellar fat, anterior to the reconstructed ACL graft. The lesion displayed hypointense signal in T1, PD and STIR sequences.
Like the previous case, the nodule was approached arthroscopically and excised. (Fig.4)
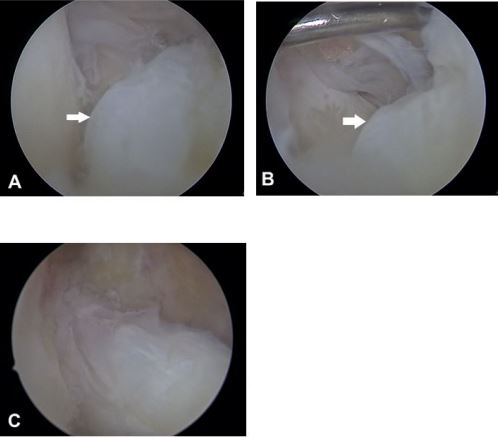
During post-operative period, rehabilitation programme was followed. After 2 weeks, full range of extension was achieved. (Fig.5 B)

Discussion
The cyclops lesions usually found 10-25% after ACL reconstruction percent of ACLR procedures [10].
Most of the cyclops lesions are asymptomatic and found in incidental postoperative MRI scans. Symptomatic lesions are rare, about 2-10% [11]. Incidence is more common in females than males [12].
The exact etiology of the cyclops lesion is unknown; but most likely of multifactorial origin. The nodule typically forms within first six months of ACLR. The debris of cartilage and bone released during tunnel drilling, rupture of graft fibers, stump of native ACL, impingement of graft on the notch all have been suggested to be involved in the pathogenesis [13].
Among many intra-operative factors, a narrow intercondylar notch was associated with a higher risk of cyclops syndrome [14]. As per the recently published article by Ficek, K., et al., the geometry of the intercondylar notch plays an important role in the occurrence. They concluded that cyclops lesions had been significantly occurring with lower notch shape index and notch width index than with others [15].
The nodule gets pinched between the tibia and femur which then blocks at the later stages of extension. Presence of cyclops lesion inside the knee alters gait mechanics which is different from ACLR patients without a cyclops lesion [16].
MRI scan is the modality of choice for identifying cyclops nodules after ACL reconstruction; additionally it helps rule out other possible causes of knee stiffness. Lesions appear in MRI as nodule with a convex anterior border. On T1-weighted images, they appear with low to intermediate signal intensity. MRI offers the best diagnostic test for cyclops lesions with a sensitivity of 85%, a specificity of 84.6% [17].
On arthroscopy, the lesion has a head-like appearance with a focal area of reddish-blue discoloration due to venous channels that resemble an eye. Hence, the name “cyclops lesion.”
Aggressive physical therapy does not improve extension loss associated with cyclops lesions [18]. Persistent loss of knee extension for more than 6 weeks even after aggressive rehabilitation should raise suspicion of a cyclops lesion [19]. It is also important to rule out other causes of loss of extension namely intra-articular adhesions, fibrosis of the fat pad and capsular contracture [20].
Conclusion
High index of suspicion and thorough evaluation through history, clinical examination and MRI for cyclops
lesion in cases of ACLR who report with extension deficit is essential. Arthroscopic resection followed by
postoperative physical therapy yields excellent results in the relief of symptoms.
Conflict of Interest: The authors declare that there is no conflict of interest regarding the preparation of this manuscript.
Funding Sources: None.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!