Biography
Interests
Ahmed Sonbol, M.*, Lutf Abumunaser, A. & Amre Hamdi, S.
Orthopedic Surgery, King Abdulaziz Univesity, Jeddah, Saudi Arabia
*Correspondence to: Dr. Ahmed Sonbol, M., Orthopedic Surgery, King Abdulaziz Univesity, Jeddah, Saudi Arabia.
Copyright © 2019 Dr. Ahmed Sonbol, M. , et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Major orthopedic surgeries such as total knee arthroplasty (TKA) which have a particular high risk
to develop venous thromboembolism (VTE). Factors such as older age, female sex, higher body
mass index, bilateral surgery, operation time more than 2 hours, VTE history and other factors were
found as a VTE risk after TKA in the literature. This risk is improved significantly with use of
thromboprophylaxis.
To determine the incidence of VTE post TKA and associated factors with its occurrence among
our population.
Retrospective chart review of 348 cases of primary TKA performed between January 2008 to December 2012. Various known risk factors of VTE were retrospectively studied for each case.
Descriptive and relationship studies were conducted beside comparison of means were used to
determine significance of each factors.
A total of 348 cases had TKA in King Abdulaziz university hospital were reviewed. unilateral TKA
300 (86.2%) and simultaneous bilateral TKA 48 (13.8%). Female cases were 371(73.9%). Mean
length of stay was 11.02 days (SD ± 6.2). VTE was present in 8 cases (2.3%), either symptomatic
DVT or PE. Diabetes was found in 125 cases (35.9%) and 6 cases of them had VTE (p-value =
0.020). Start of post-op mobilization day mean was higher in cases who later found to have VTE
(p-value = 0.045). Other factors such as advanced age, Previous History of VTE, female sex, history
of cerebrovascular event, heart failure, obesity, longer operation time and use of pre-operative VTE
pharmacological prophylaxis showed no statistical significance. Length of stay was significantly
higher in cases of VTE.
Incidence of VTE post primary TKA in our population is comparable to literature. History of
diabetes and delayed mobilization are significant risk factors for these events. Presence of VTE was
a significant cause for longer hospitalization after primary TKA surgery.
Abbreviations
AAOS: American Academy of Orthopedic Surgeons
BMI: body mass index
DVT: Deep venous thrombosis
OA: osteoarthritis
PE: pulmonary embolism
TKA: total knee arthroplasty
VTE: venous thromboembolism
Introduction
Knee Osteoarthritis is a common condition in Saudi Arabia [1-3]. Total knee arthroplasty (TKA) is the
standard of care of management of end stage osteoarthritis(OA) when standard nonsurgical methods have
failed [4]. TKA is considered a major orthopedic surgery procedure which have a particular high risk to
develop venous thromboembolism (VTE) in the perioperative period, and routine thromboprophylaxis has
been included as standard care for them for many years [5,6]. Without pharmacological prophylaxis, VTE
was detected by venography in 40 to 60% of major orthopedic surgery patients [7]. This incidence was
much improved with the use of VTE prophylaxis to 1.09% for patients undergoing total or partial knee
arthroplasty [8]. Older age, female sex, higher BMI, bilateral surgery, operation time more than 2 hours,
VTE history and other factors were found as a VTE risk factors of TKA [9-12]. Among our population, there is very few recent studies of VTE incidence following TKA [13]. The aim of
this study was to determine the incidence of VTE post primary TKA in our institution and its associated
factors.
Methodology
After ethical committee approval obtained, 276 patients who underwent 348TKA from January 2008
to December 2012 in King Abdulaziz University Hospital, Jeddah, Saudi Arabia were recruited in this
retrospective study. Cases of revision TKA and conversion of unicompartmental knee arthroplasty to TKA
were excluded. 5 Files were missing. The electronic medical records and digital radiographes were reviewed
to obtain the demographic, clinical, and radiological data. These data included the presence of known
VTE risk factors, mobilization post-op, anesthesia type and duration, duration of surgery, pharmacological
prophylaxis, intensive care unit (ICU) admission post op, readmission for VTE, presence of DVT or PE
and death for each case. VTE presence was in case of diagnosed symptomatic deep vein thrombosis (DVT)
or confirmed pulmonary embolism (PE). Positive DVT was only considered if radiologically confirmed by
Doppler ultrasound. Chest computed tomography (CT) angiography was the method for PE diagnosis.
Mobilization post-op was defined in this study by the time patient start walking few steps after the operation..
This study was analyzed using IBM SPSS version 22. A simple descriptive statistics was used to define the characteristics of the study variables through a form of counts and percentages for the categorical and nominal variables while continuous variables are presented by mean and standard deviations. To establish a relationship between categorical variables, this study used chi-square test. While comparing two groups means variable an independent t-test was used. These tests were done with the assumption of normal distribution. Otherwise, Welch’s t-test for two group means was used. Lastly, a conventional p-value <0.05 was the criteria to reject the null hypothesis.
Results
Of the total 348 cases, unilateral TKA was done in 300 cases (86.2%) and simultaneous bilateral TKA for
48 cases (13.8%). 15 patients had staged bilateral TKA on same admission. The mean age was 64.41 years
(± 9.3). Female cases were 257 (73.9%) and male were 91 cases (26.1%). Diagnosis of osteoarthritis was in
341 cases (98.0%) and the remaining 7 cases had rheumatoid arthritis (2.0%). Body mass index (BMI) in
318 cases mean 35.15 (± 6.6) and 30 cases BMI was not documented in the chart. ICU admission post-op
was reported in 11 cases (3.2%). Length of stay mean is 11.02 days (± 6.2) for all cases. Death was reported
in one case post op due to myocardial infarction.
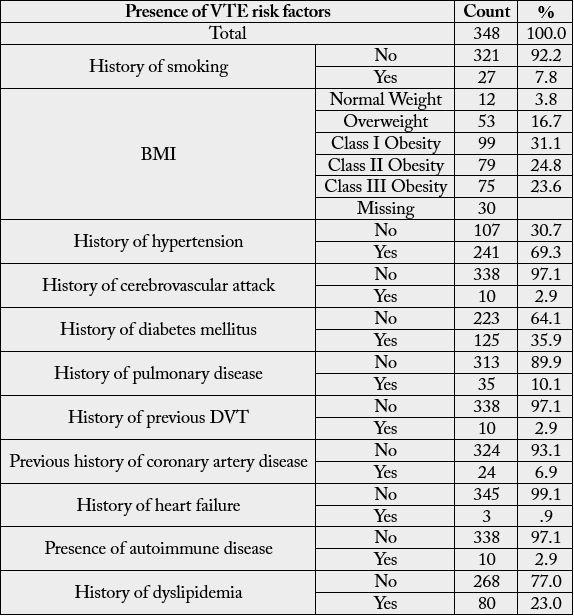
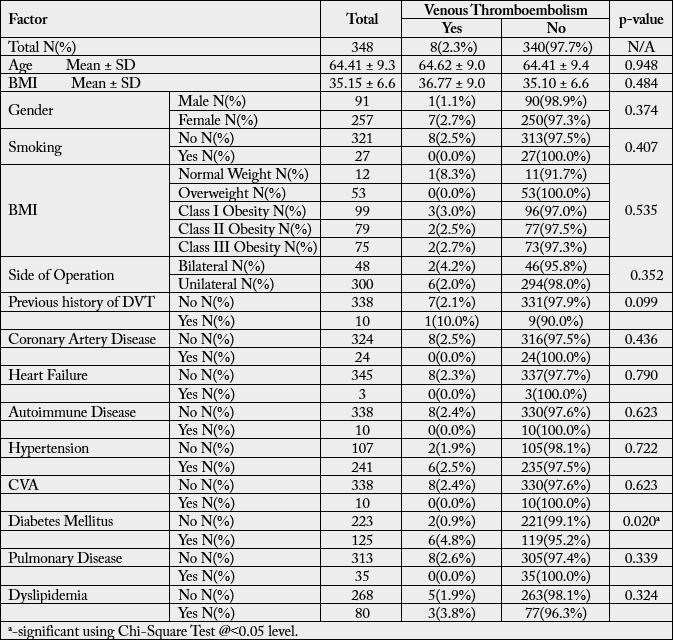
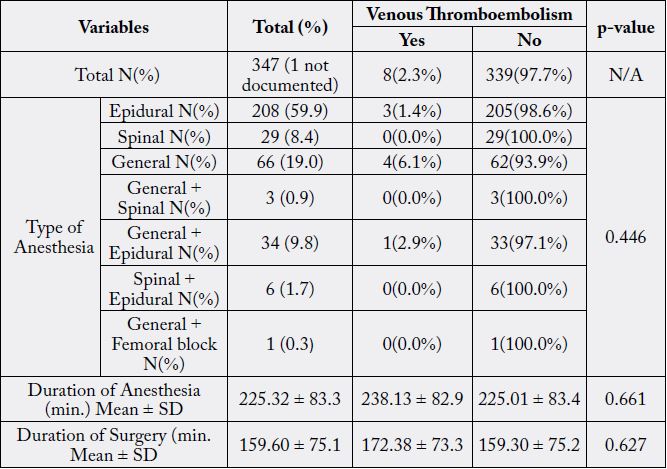
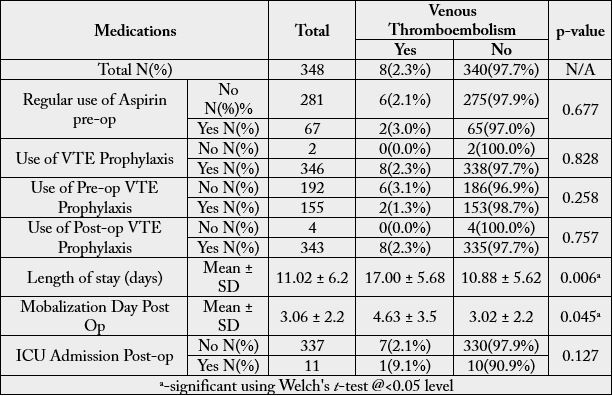
VTE incident in 8 cases (2.3%) post TKA, 5 patients had DVT post op (1.4%) and 4 patients had diagnosis of PE (1.1%), as 1 patients had confirmed DVT and PE. Diagnosis of either DVT or PE was on 4, 7, 9, 12, 12, 30, 82 and 229 days post-op. In-hospital VTE occurred in 5 cases (1.4%) and the other 3 cases (0.9%) needed readmission. Presence of known VTE risk factors summarized in (table1). Age, Gender and BMI found to had no significant relation (p-value < 0.05) with VTE development post TKA. Two of the patients who had simultaneous bilateral TKA developed VTE (4.2%) and six of the unilateral group developed VTE (2.0%) although it was not statistically significant. Length of stay was affected significantly by presence of VTE (p-value = 0.006), cases who had VTE had mean length of stay 17.00 days (± 5.68) in comparison to negative cases 10.88 days (± 5.62). Diabetes mellitus (DM) was found in 125 cases (35.9%). Six patients (4.8%) with VTE had DM (p-value = 0.020). Factors relation and significance with VTE on (Table2). Most was given epidural anesthesia 208 cases (59.9%) with anesthesia mean duration of 225.32 minutes (± 83.3), more details and association of anesthesia with VTE is in (table 3). Surgery time mean was 159.60 minutes (±75.1) and was increased in VTE cases to 172.38 (±73.3) which is not significant (p-value = 0.627). Start of post-op mobilization day mean was longer in cases who later found to have VTE from 3.02 (± 2.2) to 4.63 (± 3.5) of statistical significance (p-value = 0.045) (table 4). Use of Aspirin regularly pre-op in 67 cases (19.3%) had no relation with VTE occurrence. Two cases (0.6%) had not received any pharmacological prophylaxis before or after the operation and other 2 did not receive post op only. Preoperative pharmacological prophylaxis was given in 155 cases (44.7%), of them, two cases had VTE. While 192 cases (55.3%) did not receive pre-op prophylaxis and 6 cases of them had VTE. this difference had no statistical significance (p-value 0.258).
Discussion
Our incidence of all VTE was 2.3% including DVT which was 1.4% and PE 1.1% ,which is almost
approaching the results found in Almegren and Bakhsh`s study with 2.4% on 205 patients from same
population between May 1989 and August 2005 [13,14] In-hospital incidence of VTE was 1.4% in our
study, which is comparative to what reporetd by Januel et al (1.9% for symptomatic post-op VTE before
hospital discharge) in a meta-analysis of 47 randomized clinical trials and observational studies included
44`844 cases receiving prophylaxis for total or partial knee arthroplasty with pooled rates of symptomatic
DVT of 0.63% and 0.27% for PE [8].
According to American Academy of Orthopaedic Surgeons (AAOS) VTE prevention guideline, current evidence is not clear about whether factors other than a history of previous venous thromboembolism increase the risk of VTE in patients undergoing elective TKA [6].This factor had no significance with VTE increase in our study. In contrast, presence of DM had shown to be a risk factor in our study. DM is associated with increased risk for VTE generally [15,16], although in most studies it was not proved to be a risk factor for VTE in TKA patients [9,12,17], or even is associated with lower risk [18]. AAOS recommended early mobilization as soon as possible following TKA even In the absence of reliable evidence [6]. That would address the stasis limb of Virchow’s triad; movement of the operated limb promotes regional blood flow. In this study delayed mobilization post op was significantly associated with VTE which is consistent with other studies [11,19-21]. Simultaneous Bilateral TKA had no significant increase risk for VTE over unilateral TKA in our study but it was increased risk in some literature [10,22]. Neither type of anesthesia nor duration of anesthesia showed significance with VTE occurrence in this study or many other studies [23-25], however, AAOS recommends neuroaxial anesthesia to help limit blood loss [6,21]. Some studies suggest that advanced age, female sex, history of cerebrovascular event, heart failure, obesity, and longer operation time are associated with more VTE post TKA [9,11,12,17,21,26-28] these findings could not be agreed in our study.
Use of pharmacological prophylaxis for VTE was given for 99.4% of cases in this study which is recommended by AAOS guideline to decrease the incidence of these events [6]. AAOS guideline is unable to recommend for or against specific prophylactics because current evidence is unclear about which prophylactic strategy is optimal or suboptimal. In this study, regular use of Aspirin or the use of pre-operative pharmacological prophylaxis had no statistical significant prevention of VTE. Length of stay was significantly affected by VTE in this study.
The retrospective nature exists some limitation of this study such as missing files and incorrect recoding or missing data. Some VTE cases could be missing due to follow up or admission in other hospital. Asymptomatic VTE could not be traced in this study type. We recommend clinical trials and detailed studies of prophylaxis of VTE and other complications post TKA especially in our population due to very lack of studies in this field.
Conclusion
Our findings showed that the incidence of VTE post primary TKA in our population is comparable to rates
found in literature. History of DM and delayed post op mobilization were found to be associated with VTE
significantly. Presence of VTE was a significant cause for longer hospitalization after primary TKA.
Conflicts of Interest
No conflict of interest.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!