Biography
Interests
Evija Stumbra Stumberga1*, Gaida Krumina2, Silva Senkane3, Olga Voika4, Liana Ziediņa5 & Edgars Vasiļevskis6
1Specialist in Rheumatology, Department of Rheumatology, Riga Stradins University, Latvia
2Professor of Radiology, Department of Radiology, Riga Stradins University, Latvia
3PhD specialist in Quantitative Social Research, Statistics Unit, Riga Stradins University, Latvia
4Specialist in Radiology, Lecturer in Language Centre, Riga Stradins University, Latvia
5Specialist in Neurosonology, Health Center 4, Latvia
6PhD Specialist in Anesthesiology, Riga Stradins University, Institute of Anatomy and Antropology, Latvia
*Correspondence to: Dr. Evija Stumbra Stumberga, Department of Rheumatology, Riga Stradins University, Latvia.
Copyright © 2018 Dr. Evija Stumbra Stumberga, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Rheumatoid arthritis is a chronic systemic autoimmune disease. It causes chronic inflammation of joints manifesting with swelling, pain, synovitis and joint destruction. High work disability rates, as well as functional decline due to knee and hip joint destruction can lead eventually to both total knee and hip replacement surgeries.
Little is known about the predictors of the prevalence of joint arthroplasty over the course of the disease. Therefore, verification of the predictive factors of aggressive disease course could manage the need for joint arthroplasty in future. The purpose of our study was to analyse and evaluate the factors contributing to the need of joint replacement surgery with regard to the highly aggressive course of the disease in a cohort of rheumatoid arthritis (RA) patients. A case-control prospective study was conducted with one hundred fifteen RA patients. According to our case-control study, both high disease activity evaluated as Das 28>5.1 and high titers of Anti-CCP (above 500 U/ ml) were not strong predicting factors of joint replacement therapy. Neither the age when RA was diagnosed, nor the age when complaints started, seropositivity for Anti-CCP, RF, synovitis in the small joints, comorbidities (primary arterial hypertension, stroke, diabetes mellitus), smoking history, and BMI had any association with the joint replacement surgery. However, we determined that only those patients with erosive changes in the small joints of the hands and feet (detected radiographically) required a total joint arthroplasty.
Abbreviations (if used)
RA - Rheumatoid Arthritis
BMI - Body Mass Index
Anti-CCP - Anti-Citrullinated Protein Antibodies)
RF - Rheumatoid Factor
DAS 28 - Disease Activity Score 28 joints
CDAI - Clinical Disease Activity Index
HAQ - Health Assessment Questionnaire for Rheumatoid Arthritis
TJA - Total Joint Arthroplasty
TJR - Total Joint Replacement
Introduction
Rheumatoid arthritis is a chronic autoimmune disease characterised by persistent inflammatory synovitis,
involving small hand and feet joints in symmetric distribution [1]. The prevalence of RA is approximately
0,8% of the population, affecting women three times more often than men. The onset is most frequent
during the fourth and fifth decades of life [2,3].
Early diagnostics and disease pattern recognition in conjunction with the new generation of more powerful biologic DMARD treatment facilities improve the long - term outcome, functional status of RA patients and protect RA affected joints from irreversible destruction. Moreover, it is well-known that approximately 25% of patients with RA undergo multiple joint replacement surgeries [4]. Regarding this, we have to acknowledge that little is known about the predictors of the prevalence of joint arthroplasty over the course of the disease. The purpose of our study was to analyse and evaluate the factors contributing to the need of joint replacement surgery with regard to the highly aggressive course of the disease in a cohort of rheumatoid arthritis (RA) patients.
The above - mentioned factors comprised the following: analysis of DAS 28 (>5,1) and CDAI scores, seropositivity, extremely high titers of anti CCP (above 500 U/ml), erosive disease status, smoking history, another clinical factors, as well as co-morbidities that alter the severity of RA outcome, such as joint failure.
Materials and Methods
This was a case-control prospective study of the patients with RA that lasted between 2012 and 2017.
The consecutive patients who fulfilled the 2010 criteria for RA, with the disease duration exceeding 6 weeks and without a prior disease - modifying antirheumatic drug use were included in our study.
The patients who underwent total joint arthroplasty after the diagnosis of RA were included as the cases for this study. The controls were selected randomly from the cohort of patients with RA, who had similar disease duration (exposure time to inflammation) for cases and controls.
Comprehensive information on co-morbidities (including diabetes mellitus, stroke, primary arterial hypertension, smoking history) and the course of the disease was regularly collected and stored in the electronic database. Clinical and radiographic examinations, as well as laboratory tests were obtained during each follow up visit at the Health Centre 4 and Riga 1st Hospital out-patient rheumatology facility. During each clinic visit the following variables were recorded: body mass index, (BMI), smoking history, radiographic erosions, synovitis on musculoskeletal ultrasound of the small hand and feet joints. We had access to the medical files of each patient; therefore, the registration of co- morbidities and medical events was complete.
The case and control groups were matched in age, gender, and duration of the disease to better investigate other predisposing factors.
In the cohort, disease activity was prospectively assessed by the DAS28 and CDAI scores [5].
The CDAI or Clinical Disease Activity Index evaluates 28 tender and swollen joints (shoulders, elbows, wrists, metacarpophalangeal joints, proximal interphalangeal joints and the knees). CDAI is useful to make a correct assessment of the rheumatoid arthritis activity [5].
The DAS28 is a measure of disease activity in rheumatoid arthritis [6]. DAS stands for ‘disease activity score’ and the number 28 refers to the 28 joints that are examined in this assessment DAS 28, it is calculated from the 28-tender joint count, 28-swollen joint count, C-reactive protein and the patient’s global assessment of disease related general health on a visual analogue scale. Calculated Das 28 >5,1 was selected as a very active disease process.
Disability was assessed by using the disability index of the Health Assessment Questionnaire (HAQ). HAQ includes questions of fine movements of the upper and lower extremities. It is a sensitive tool for measurement of health status [7,8].
Severity of the disease was determined by presence of erosions, radiographically proven, in the small hand and feet joints, as well as synovitis of the synovial joints of hands and feet, detected by musculoskeletal sonography.
Circulating biomarkers - rheumatoid factor (RF), anti-cyclic citrullinated peptide (Anti- CCP) antibodies
were a analyzed from frozen serum or plasma by ELISA tests. High titres of Anti- CCP antibodies above
500 U/ml were regarded as pronounced production of antibodies.
Joint surgery data were collected during the first clinic visit of patient. A total joint arthroplasty was
considered to be any surgery that resulted in the placement of a total joint prosthesis that was the primary
surgery. None of the cases had secondary/subsequent joint replacement to replace total joint prosthesis, also
known as revision. Procedures of non-prosthetic surgery including fusions, tendon transfers, bursectomies,
synovectomies, laminectomies of the cervical, thoracic or lumbar spine were not included in our study.
Moreover, other clinical variables were also obtained. The above mentioned variables included female gender,
metabolic dysfunction, hypertension, diabetes mellitus, smoking.
The BMI is generally used as a means of correlation between groups related by general mass and can serve as a vague means of estimating adiposity. Body mass index (BMI) was calculated from height and weight at a baseline [9]. Diabetes mellitus was regarded as present if the diagnosis was made before the event or censoring.
Hypertension was defined as a history of hypertension, use of antihypertensive medication before the event or censoring, systolic office blood pressure ≥140mm Hg and/or diastolic office blood pressure ≥90mm Hg. Brachial blood pressure was measured according to the European Society of Hypertension guidelines by an OMRON M7 apparatus (Kyoto, Japan) [10]. The average of the last two measurements was reported.
Information on smoking history and occurrence of cerebrovascular disease (stroke ischaemic and haemorrhagic) was assessed during patient appointments, as well as obtained from the medical records of patients.
Data collection procedures. This study was approved by the Riga Stradins University Committee for Research Ethics. All subjects gave a written informed consent prior study examinations.
The statistical analyses were undertaken using IBM SPSS statistics V.22.0 (IBM, Armonk, New York,
USA). Normally distributed continuous data were expressed as mean and SD and non-normally distributed
continuous data as median and IQR. Categorical variables were presented as numbers and percentages.
Both the cases of TJA and controls were compared by disease activity variables, as well as other factors by
using the Mann-Whitney U test (for continuous variables), the Pearson’s X² test, or Fisher’s exact test (for
dichotomous variables). In this report Kaplan -Meier survival statistics were used for data analysis.
Results
The consecutive 115 patients were enrolled in this study and followed up for 5 years, of whom the patients
with joint replacement surgery (84.6%) were females with a mean age of 59.23 (±13.0) years. The case and
control group did not statistically differ in age (p=0.842) or gender (p=0.715). The BMI is an attempt to
quantify the amount of tissue mass (muscle, fat, and bone) in an individual, and then categorise that person
as underweight, of normal weight, overweight, or obese based on that value [9]. The BMI was 27.71(±3.84),
as was calculated for the patients of the case group (p=0.247).
The mean age of the patients when RA was diagnosed was 56.15 (±15.28) years, the mean of the disease duration - 6.52 (±6.31) years. The case and control group did not statistically differ in the disease duration (p=0.387). In our study, the mean age when RA complaints appeared was 52.46 (±13.68), (p=0.902).
Of all the case group patients, 69.2% suffered from arterial hypertension (p=0.764), 15.4% experienced stroke (p=0.611), and 7.7% had such co-morbidity as diabetes mellitus (p=0.457). Smoking was detected in 30.8% of cases (p=0.394), a long-term smoking history was observed for 30.75 (±13.74) years (p=0.210).
Table 1 summarizes the description for each of these case and control groups.
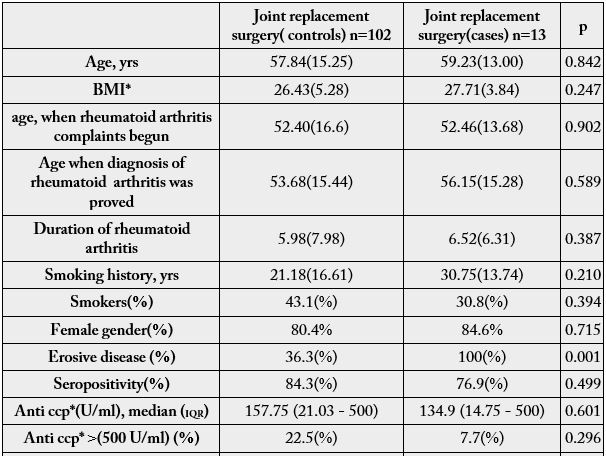
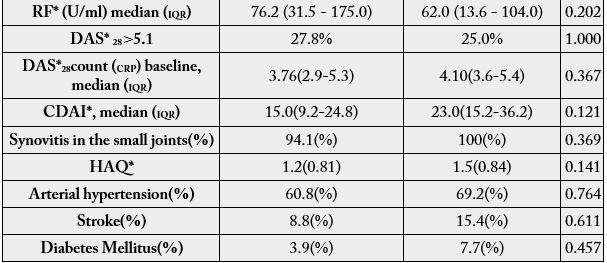
BMI-body mass index
Anti - ccp - anti-citrullinated protein antibodies
RF - rheumatoid factor
DAS 28 - Disease Activity Score 28 joints
CDAI - Clinical Disease Activity Index
HAQ - Health Assessment Questionnaire for Rheumatoid Arthritis
Distribution of Joint Surgery in RA
Over 6.52(±6.31) years of the disease duration, the 13 case patients underwent total joint arthroplasty (TJA).
Of all joint replacement surgeries of the hip joints, the unilateral hip joint replacements comprised 38.5%,
bilateral hip joint replacements - 30.8%; of all the knee joint replacement surgeries (total knee arthroplasty),
unilateral were 15.4% and bilateral knee joint replacements - 23.1%, while unilateral surgeries of the small
hand joint comprised only 7,7%.
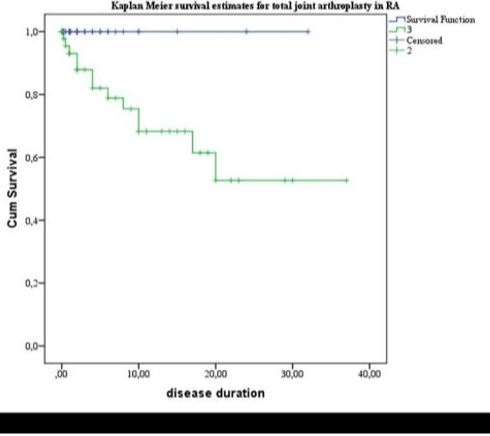
Figure 1 Kaplan- Meier survival curves demonstrating the risk of total joint arthroplasty for rheumatoid arthritis (RA) patients.
Kaplan - Meier survival curve demonstrates 5 year TJA surgery risk of 0,18 CI (0.06-0.30) of total joint arthroplasty for rheumatoid arthritis patients. (Figure 1)
Disease activity evaluated by the Das 28 (CRP) score for the case group was 4.10 (3.6-5.4) and 23 (15.2- 36.2) assessed by the CDAI. Disease activity in the case group did not differ from the control group, the Das 28 score (p=0.367), and the CDAI score (p=0.121), consequently. In an attempt to estimate the aggressive nature of the disease, high grade inflammation was assessed as Das 28>5.1. It was observed only in 25% of cases, Fisher exact test (p=1.000), in the control group it was observed in 27.8% of cases. One should take into account that a persistent disease activity is accompanied by joint abnormalities and functional impairments; however, in our study we did not find any correlation with the TJR. We searched further for other factors that could potentiate development of joint abnormalities and cause the necessity of joint replacement surgery.
Therefore, we evaluated other features that correlate with a greater likelihood of development of joint destruction [1]. These include radiographic evidence of bone erosions, high titers of serum rheumatoid factor (RF) or Anti -CCP antibodies, presence of functional disability and co-morbid conditions [1].
Joint erosive disease was found in 100% of the case group patients on their radiographs of the small hand and feet joints, that was statistically different from the control group, the Pearson Chi-Square (p<0.001).
Seropositivity for RF and Anti - CCP was found in 76.9% of the patients with joint replacement therapy; however, it did not differ between the case, and the control group: for RF (p=0.198), and Anti-CCP (p=0.848), respectively. High titers of Anti - CCP (above 500 U/ml) were registered in 7.7% of cases, Fisher exact test (p=0.296).
HAQ did not differ between the case 1.5(±0.84), and the control groups 1.2(±0.81); (p=0.141).
Synovitis on musculoskeletal ultrasound was found in both groups equally (p=0.369) and affected 100% of the case group patients.
Of all the case group patients, 69.2% suffered from primary arterial hypertension (p=0.764), 15.4% experienced stroke (p=0.611), and 7.7% had such co-morbidity as diabetes mellitus (p=0.457). Smoking was detected in 30.8% of cases (p=0.394), a long-term smoking history was observed for 30.75(±13.74) years.
Discussions
It has been speculated that highly aggressive disease course of RA would lead to more pronounced disability
due to joint destruction and eventually lead to TJR surgery. Our task was to evaluate the important markers
of a highly active disease - Das 28 >5,1 and seropositivity (Anti - CCP, RF and Anti- CCP above 500 U/
ml), as well as other features of clinically severe RA course to determine their prognostic value in joint failure
and subsequent need for TJA (total joint arthroplasty).
The course of RA has been valued by DAS 28 score and CDAI index, allowing to categorise all the patients into those with high, moderate, and low disease activity. Presence of highly active disease status implies a greater likelihood of developing progressive joint abnormalities and joint failure [1]. In our study evaluation of the disease activity in the case group did not differ from the control group, the Das 28 score (p=0.367), the CDAI score (p=0.121), respectively, moreover, high grade inflammation assessed as Das 28>5.1 was observed in only 25% of cases, Fisher exact test (p=1.000). Thus, there could be other underlying pathogenetic mechanisms involved that provoke active bone resorption and joint destruction. Persons who present with high titers of rheumatoid factor, Anti - CCP antibodies [11] also have a worse prognosis as do individuals with subcutaneous nodules at the time of initial evaluation. Presence of Anti-CCP is especially common in persons with aggressive disease, with a tendency for developing bone erosions [12]. With regard to this, patients with RF and Anti CCP antibodies, as well as high titers of Anti- CCP antibodies were analyzed. In previous studies RF has been remarkably raised in those patients who required TJR [4]. Therefore, with great expectations we investigated all those variables. Although mostly all the case patients with TJR surgery were seropositive: 76.9% of the patients with joint replacement therapy were seropositive for RF and Anti- CCP, there was no statistically significant difference between the case, and the control group - for RF (p=0.198), and for Anti - CCP (p=0.848), respectively. High titers of anti CCP (above 500 U/ml) were registered in only 7.7% of cases. Perhaps with larger amount of cohort patients and other titer levels of Anti - CCP, the results would give more additional information.
Development of Anti - CCP is most frequent in RA individuals who smoke. In some studies (past or current) smoking has been indicated as a predictive factor for TJR surgery [4]. It has been suggested that smoking alters bone, thereby, impedes joint destruction in weight - bearing joints either directly or through its antiestrogen effect. Despite a long - term smoking history in the case group patients - median of 30.75(±13.74) years, smoking status (past or current) was detected in 30.8% of cases that explains statistically insignificant result (p=0.394).
Radiographic erosions are objective markers of a disease progression that in our study correlate with TJR surgeries, but they are poorly related to the key functional features of the illness, such as pain and functional disability. In our study the case group had a slightly greater (HAQ-DI) HAQ Disability Index 1.5(±0.84) that did not differ statistically from the control group patient.
Taking into account the National Health System, financial status and other variable parameters that alter and affect the rate of the proceeding surgeries, we compared the information concerning the rates of TJR surgery in our study with other Northern Europe Countries [13]. We found out that our observations on TJR rates are generally similar.
The proportion of the patients undergoing TJA in our study was 18% during 5 years of disease duration, according to Kaplan - Meier survival analysis. That is comparable with other studies [3,4,14].
It is anticipated that both ageing and obesity increase demand for TJR surgeries. In our study the patient age of 59.23 (±13) years was matched between the case and control groups and was comparable with other studies [4].
The mean of BMI was 27.71 (±3.84), as calculated for the patients of the case group, is positively attributable more to overweight category. In the routine practice it is observed that overweight and obese individuals are at increased risk for comorbidities [15,16]; thus, leading to more complications and difficulties to receive a complete remission in rheumatoid arthritis.
RA usually starts as synovitis of the small hand and feet joints, destroying them first, but surprisingly enough, just one of all 13 case patients was operated on for the left hand joint prosthesis.
What is interesting, in our case control study only 15.4% of the case patients were observed to experience stroke (cerebrovascular accident), although RA patients are prone to chronic inflammatory reaction that eventually lead to procoaguable/prothrombotic status [17].
Conclusions
In our case-control study both high disease activity evaluated as Das 28>5.1 and high titers of Anti - CCP
(above 500 U/ml) were not good predictors of the joint replacement therapy.
However, joint replacement therapy was found to be associated with erosive disease of the small joints of hands and feet detected radiographically. Neither the age when RA was diagnosed, nor when the complaints appeared, presence of seropositivity for Anti-CCP, RF, synovitis of the small joints, co-morbidities (primary arterial hypertension, diabetes mellitus), as well as smoking history and BMI had any association with the joint replacement surgery.
It was a prospective cohort study that included the RA patients with the various severity of the disease selected from 2 different primary care clinics; thus, all the above-mentioned supports the relevance of the results acquired.
Future observations are needed to reveal alternative risk factors influencing RA patients in whom a severe disease course is accompanied by radiographic progression, work disability and rapid joint destruction that lead eventually to total joint replacement surgery.
Conflicts of Interests
None
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!