Biography
Interests
Cameron Kia1, Yasser Faraj2, Emily Isch1 & Vinayak Sathe1*
1Department of Orthopaedic Surgery, University of Connecticut Health Center, Farmington, CT, USA
2Lake Erie College of Osteopathic Medicine, Erie, PA, USA
*Correspondence to: Dr. Vinayak Sathe, Department of Orthopaedic Surgery, University of Connecticut Health Center, Farmington, CT, USA.
Copyright © 2018 Dr. Vinayak Sathe, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Newer minimally invasive and percutaneous techniques of the Achilles tendon are ever evolving with few reviews examining the long-term data along with comparisons to open procedures. The purpose of this study is to review the literature on various percutaneous techniques of Achilles repair, along with their clinical outcomes.
Introduction
Although it is the strongest and thickest tendon in the body, Achilles tendon ruptures are the most frequently
ruptured tendons in the lower extremity, with an incidence ranging from 5.5-9.9 ruptures per 100,000 people
[1,2]. A higher frequency of ruptures tend to occur in athletes and middle-aged people while participating in
recreational activity, and is a significant cause of morbidity. While traumatic injuries and sporting activities
are a major cause of tendons ruptures, other risk factors include drugs like fluoroquinolones antibiotics
and corticosteroids as well as footwear, and walking surfaces, all of which contribute to the biomechanical
degeneration and ruptures on Achilles tendon [3,4].
Ideal treatment algorithm to repair a ruptured Achilles tendon remains to be determined. Treatment options include a conservative cast immobilization, percutaneous and minimally invasive repair, and open surgery [5]. Each treatment comes with its advantages and disadvantages. A recent retrospective study compared the clinical and functional outcomes of the three treatments options.5 They reviewed twentyeight patients with a minimum follow-up of 24 months (average 25.7, SD:6.3) [5]. Patients were divided into 3 groups: conservative non-operatively managed group (n = 8), minimally invasive percutaneous repair group (n = 7), and traditional open surgery (n = 11). The study reported a significantly higher patient satisfaction and Thermann scores in patients who were surgically treated than those who were managed conservatively [5]. Interestingly, this small study showed no significance difference between open and minimally invasive operated patients [5]. Other studies have shown that surgical repairs carries with it an increased risk of infections, iatrogenic sural nerve damage and other complications [6,7].
Nonetheless, surgical managements have been favored over the nonsurgical treatments due to higher risk or re-ruptures associated with the non-operative treatment [8,9]. However, advancement of the non-operative techniques and adoption of early rehabilitation and functional casting has gained more popularity in more recent years and showed a re-rupture incidence that is comparable to operative treatment [6,10].
Percutaneous Repair
Percutaneous repairs were first described in 1977 by Ma and Griffith and it offers a good compromise
between the conservative non-operative treatments and the traditional open surgery treatment options [11].
Nevertheless, it has come with its own complications including sural nerve injury [12]. In order to better
localize the sural nerve and identify its anatomical course in relation Achilles tendons, MacMahon did a
retrospective review of MRI studies of the Achilles tendons that were done in healthy people and people
with injured Achilles tendon [13]. His research found that the Achilles tendon was more externally rotated
when ruptured than in non-ruptured cohort at the level of the ankle and that its distance to the sural nerve
differed between the 2 cohorts in the A-P and M-L planes [13]. He suggested that during percutaneous
repair, to externally rotating the proximal end of the rupture by 11° and the distal end 16° to minimize sural
nerve injury and increase tendon capture [13].
Percutaneous Techniques
Since 1977, many modification and variations of the original technique has been described. This review
article addresses the recent literature on different minimally invasive and percutaneous techniques. It also
presents the current literature comparing outcomes of different treatment approaches using outcomes scores
like American Orthopedic Foot and Ankle Society (AOFAS) [14] and Achilles tendon Total Rupture Score
(ATRS) [15].
The Ma & Griffith technique consisted of 4 stab incisions proximal to the rupture and 2 stab incisions distal to it [11]. Rozis reported results using this percutaneous technique on 41 patients, of which, 3 patients developed paresthesias due to sural nerve entrapment but none had any wound complications [16]. The mean return-to-work time was 7.9 weeks, while the AOFAS and ATRS scores were 96 and 95, respectively [16].
Maffulli et al. added their own modification to the technique by passing a needle with larger curvature radius through the stab incisions in a Bunnell fashion [17]. They found the wider curvature was shown to minimize iatrogenic sural nerve injuries [17].
Webb and Bannister developed another modified percutaneous technique in order to avoid iatrogenic sural nerve injuries [18]. Instead of using paratendinous stabs, three posterior midline stab incisions were made and 2 nylon box stitches were used to bring the distal and proximal ends of ruptured tendons together [18]. They performed this techniques on a series of 27 patients, none of which had sural injuries or late reruptures [18]. The average return-to-work time was 4 weeks and return to sports activities was 4 months [18]. More recently, Makulavicius et al. performed a cadaver study in which he compared the standard Bunnell suture to a modified-medialized percutaneous technique [19]. They reported no entrapment of the sural nerve or vein with the modified-medialized percutaneous Bunnell suture technique group, whereas 7 of 10 sural nerves and 9 small saphenous veins were entrapped when using standard percutaneous Bunnell type technique [19].
He et al. also modified the percutaneous technique by using a Kirshner wire leverage before suturing [20]. They showed that this modification can better ensure tight contact between the ruptured ends and minimize and lengthening of the tendon which could lead to weakness of gastrocnemius muscle [20].
The Achillon jig (Integra Life Science Corp., Plainboro, NJ) is a newer device used for percutaneous and minimally invasive tendon repair. Using this instrument, the sutures were guided through a transverse incision, and when the jig is removed the sutures remain within the paratenon to be tied to opposing the proximal and distal ends of the tendon [21]. Assal et al. reported the outcome of 82 patients on whom this technique was used [21]. He evaluated the patients at an average of 26 months after the procedure and reported no wound complications or sural nerve injuries [21]. However, they reported 3 re-ruptures, one from a fall and 2 from noncompliance with post-repair rehabilitations [21]. Davis et al., examined a series of 143 patients who underwent repair with the Achillon device [22]. At a mean follow-up of 25 months, they found no re-rupture and the ATRS score was 84 (range 15-100) [22]. However, there was 2 sural nerve entrapments, 7.7% overall complication rate [22].
Since then, the Achillon device has also evolved and undergone modifications. Chen et al. designed a similar instrument with the addition of a channel to further help guide the sutures [23]. He reported the outcome of 41 patients with ruptures that were repaired using channel-assisted minimally invasive repair (CAMIR) and compared the outcome with 41 patient who underwent traditional open surgery repair [23]. They found no wound complications, sural nerve injuries or re-ruptures with a mean AOFAS of 90 at 12 months follow-up in their CAMIR group and 88 for the open surgery group [23].
Recently, Liu did a retrospective study on a series of 35 cases of acute Achilles tendon rupture that were repaired percutaneously using oval forceps to guide the suture and absorbable anchor nails instead of the Achillon device.24 Patients were followed-up with for a mean of 18.6 months (range 12-19 months); there were no reported wound complications or infections, re-ruptures, or sural nerve injury [24]. At the final follow-up ATRS and AOFAS scores were 95 and 99 respectively [24].
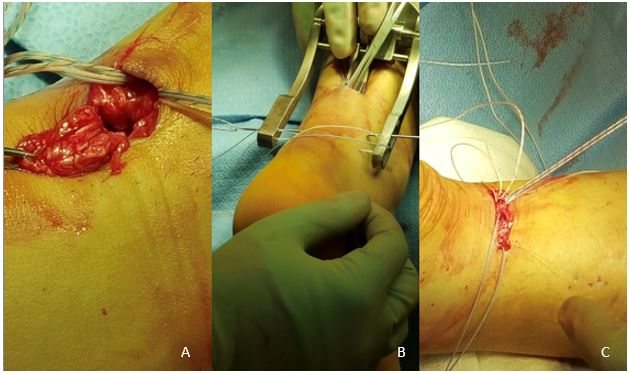
Similar to the Achillon device, the Percutaneous Achilles Repair System (PARS) (Arthrex, Naples, FL) is a knotless technique that is also widely used for minimally invasive repairs [25]. The PARS jig is inserted horizontally using a 3cm incision made about 1 cm above the distal end of the ruptured tendon (Figure 1). A malleable retractor is used to separate the proximal tendon from surrounding paratenon and the jig is advanced proximally between the tendon and paratenon. This separation minimizes the risk of sural nerve injury. Five holes on either side of the jig arms guide the sutures which are then fixed to the calcaneus distally.
Kanchanatawan described a new technique that combined the traditional open surgery technique with the percutaneous technique in hope to avoid the complications of each one when done alone [26]. This hybrid technique uses percutaneous repair at the distal stump using FiberWire no. 5 (Arthrex Inc., Naples, Fl) suture material with a 1.5-mm straight needle [26]. Proximally, open direct repair is done through a 5cm long vertical incision that is made 5 cm above the tear to avoid a vertical incision in a high-tension skin area and to avoid sural nerve injury. The torn tendon is reattached with at least 5 knots at each end and the wound is closed. While this technique still carries some risk with soft-tissue complications and blood supply disruption, it is simplified and reproducible that does not require specially designed instruments [26].
Percutaneous vs Open Repair
Multiple studies have been performed comparing outcomes of percutaneous and open surgery techniques
[27,28]. Recently, a meta-analysis of five randomized control trial and seven retrospective cohort studies
was done involving 815 patients [27]. Their study showed that of the 424 ruptures that were repaired
percutaneously, only 31 (3.1%) experienced re-ruptures.27 In contrast, only 12 (2.7%) of 442 patients that
underwent open repair experienced re-ruptures, however, the difference was not statistically significant (P
= 0.38) [27]. However, there was a significant difference in the occurrence rate of sural injury (P = 0.006)
between percutaneous repair group (5.5%) and open surgery (1.2%) [27]. Comparing deep infections rates,
the open technique had a significantly higher rate of infection (3.6%) while the percutaneous repair only
showed 0.6% occurrence rate of deep infections [27]. Fixed effect analysis of AOFAS scores between the
two groups showed a statistically significant difference (P = 0.005) between the open repair group (AOFAS
score = 98.4) and the percutaneous group (AOFAS score = 95.6). They also showed a significantly longer
operative time the open repair group compared to the percutaneous group (P = 0.001). When comparing
the various percutaneous technique used, there were no difference between difference in sural nerve injury,
deep infection rate, or deep vein thrombosis rate [27].
Jallageas et al. performed a cross-sectional study of 31 athletes with acute tendon rupture [28]. In their study, 16 ruptures were treated percutaneously and 15 rupture were repaired with open surgery [28]. After a 15 month follow-up, their study showed that patients who were treated percutaneously returned to sport 130 days after surgery while patients treated with open surgery returned after 178 days (P = 0.005). Moreover, the percutaneously treated injured athletes experienced only 13mm leg muscle atrophy which was significantly (P = 0.01) lower than the open surgery group which experienced on average 24 mm leg muscle atrophy. They reported an AOFAS score of 95.9 for the percutaneous group and 91.6 for the open surgery group, however, the difference was not statistically significant [28]. They showed no re-rupture in either group at the 15 months follow-up [28].
In another recent retrospective study, Zayni et al. examined 29 patients 16 patients who underwent percutaneous repair while 13 had open repair [29]. Both groups had the same postoperative rehabilitation and with mean follow-up of 46 months [29]. Although neither group had any major complications, the percutaneous group had 2 minor complications (1 early superficial wound infection and 1 hypoesthesia related to sural nerve injury), while the open group had a total of 4 complications (2 early superficial wound infection, 1 wound healing delay, and 1 presented with scar adherence at the final follow-up) [29]. ATRS scores were not significantly different between the two groups and both groups presented with similar AOFAS scores and return to work at follow-up [29].
Endoscopic and Ultrasound Assistance
Rungprai et al. recently delved into the benefits of endoscopic assistive percutaneous repair, a retrospective
view on 23 patients that received the repair by this method from 2008-2015 [30].
The study design utilized validated tools like the Foot and Ankle Ability Measure (FAAM), Activities of Daily Living (ADL) and Sports subscales; Visual Analog Scale (VAS); Short form-36 (SF-36), physical component summaries (PCS) and mental component summaries (MCS) to prove improvement in functional outcomes among a cohort of 23 patients, average age 36.7 years old [30]. This case series showed improvement in all primary outcomes measured. FAAM scores increased in both the ADL and sports subscales (26.1 to 83.0, and 0 to 61.7, respectively) [30]. The patients also reported significantly decreased VAS scores of 7.9/10 to 0.1/10; SF-36 scores increased in both physical and mental categories (PCS: 32.5 to 44.7; MCS: 47.9 to 51.4) [30].
In addition to these primary outcomes, the study also discussed average tourniquet time (41.3 minutes), return to work (8.8 weeks), and average time to return to daily activities (8.0 weeks) [30]. Patients returned to sports on average 5.7 months following the endoscopically assisted repair. The cohort studied had one complication associated with the surgical repair portal site (wound infection in T1DM patient), but otherwise did not report any additional complication occurrence; none of the patients followed in the follow-up period of 24 months experienced DVT, sural nerve injury, or painful scar, which were followed as surgical complications/ secondary outcomes [30].
According to a comparative case series evaluating Ultrasound (US) guided percutaneous Achilles tendon repair performed by a single surgeon from 2005-2008, Chen et al. were able to show statistically significant improvement in rates of secondary complications when comparing a group of 23 patients receiving ultrasound-guided percutaneous Achilles repair to a control group containing 25 patients, with a mean patient age of 43 years old [31].
Although the postoperative AOFAS ankle-hindfoot scores did not show a statistically significant difference between the control and the US-guided percutaneous repair (98.7 and 96.5, respectively), there was a statistically significant difference in the rates of documented complications [31]. The US-guided surgery group reported decreased rates of local infection, ankle stiffness, scar pain, and injury to the sural nerve compared to the control. This study concludes that the ultrasound guided technique is seemingly superior given the decreased complication rate and increased availability to visualize the tissue in real-time throughout the surgery [31].
Postoperative Rehab
Although the outcome of tendon repair depends substantially on the success of the surgery, post-surgical
rehabilitation plays an essential rule in the overall functional outcome of the treatment. While heavy weight
bearing postoperatively can be associated with re-ruptures and tears, functional rehabilitation that included
non-weight bearing activity has been shown to improve the functional outcome and minimize atrophy and
strength deficit after the repair [32]. A series of 30 patients who underwent percutaneous repair followed
accelerated rehabilitation were studied. Rehabilitation protocol included initial non-weight bearing walking
with crutches. After the first 2 weeks postoperatively, the plaster cast was replaced with a walker boot with
3 heel wedges, and full weight bearing was allowed [33]. The wedges were removed one by one at 2 week
intervals, achieving neutral foot position by 8 weeks [33].
Active toe and foot dorsiflexion inversion and eversion were allowed at 2 weeks but active planter flexion was discouraged until the 8th week. Tolerance and activities including proprioception training were gradually increased between the 8th and the 16th weeks after the procedure. The mean follow-up was 12.5 months and all patients were able to return to work by 3 months with an average time-to-return to pre-rupture activity of 10.4 months [33].
Another study reported the outcome of 39 patients who underwent percutaneous repair [32]. Twenty patients received aggressive rehabilitation from first day after the repair and 19 patients were in the conventional group that rested for 28 days postoperatively before the start of rehabilitation. Aggressive rehabilitation included physical therapy based on immediate controlled mobilization and weight-bearing principles. ATRS score, verbal pain score, Achilles tendon strength were all measured at 4 weeks, 8 weeks, and 12 weeks mark after the repair [32]. At all three time intervals, all three parameters showed statistically significant favorable outcome in the aggressive group when compared to the conventional group. In addition, 12 weeks postoperatively, the aggressive group showed significantly higher one-leg heel rise repetitions (41.2 SD = 19.0) comparing to the conventional group (12.8 SD = 18.0). Of note, there was one re-rupture in each group [32].
Summary
Our review found that percutaneous and minimally invasive techniques for Achilles tendon repair provide
good outcomes for acute ruptures. Studies comparing to open techniques have shown to have similar re-tear
rates with quicker operative time and reduced infection rate. However, sural nerve damage is still a concern
and visualization during surgery is always recommended. Long-term data greater than five years is still
needed for percutaneous techniques, however for now still provides an adequate fixation method.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!