Biography
Interests
Mohammed Al Sobeai1*, Hesham Abdelbary2 & Joel Werier2
1Department of Orthopedic Oncology and Lower Limb Reconstruction, Dr Soliman Fakeeh Hospital, Jeddah, Saudi Arabia
2The Ottawa Hospital, University of Ottawa, Ottawa, Canada
*Correspondence to: Dr. Mohammed Al Sobeai, Department of Orthopedic Oncology and Lower Limb Reconstruction, Dr Soliman Fakeeh Hospital, Jeddah, Saudi Arabia.
Copyright © 2018 Dr. Mohammed Al Sobeai, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
We are presenting a case report of a young lady with history of posterior thigh mass. On radiological examination, we found bony lesion with massive soft tissue extension. These findings had similarities to aggressive bone sarcoma on MRI. Pathological examination revealed intraosseous Schwannoma. After literature review, we concluded that diagnosis is mainly missed because of the rarity of the disease and intraosseous schwannoma should be included in differential diagnosis of benign looking bone lesions.
Introduction
Schwannoma is a soft tissue tumor that rarely involve bone and derived from schwann cells of nerve sheath. There are 4 main types that behave differently and has slightly different hitopathology. The most common type is conventional schwannoma. More cellular types are cellular and plexiform which are more like malignant peripheral nerve sheath tumors (MPNST) in histopathology. The fourth type is melanotic schwannoma which can be misdiagnosed as melanoma. Schwannomas do not invade the nerve fibers which help differentiate them from neurofibroma [1,2].
In 1967, Mayo clinic presented 7 intraosseous schwannomas out of 3987 (0.2%) primary bone tumors. In their series, they only included lesion originated from the bone. All schwannomas that originated in soft tissue with bone identation were excluded. Four out of the seven cases originated from the alveolar nerve in the mandible and all the remaining cases has been related to a nutrient foramen of bone [3]. In their literature review, 16 out 35 cases involved the mandible. The next bone in their series was sacrum followed by humerus and femur.
Case Report
We are presenting a case report of a 19 years old healthy lady. She is in high school and highly interested in horseback riding sport. She was referred by her family medicine with 6 months’ history of posterior thigh mass noticed by personal massage therapist. No pain or discomfort is associated and has been almost the same size since it was noticed. On physical examination, there is a palpable mass on the psterolateral mid to distal right thigh. It is not tender and fixed to bone with firm consistency.
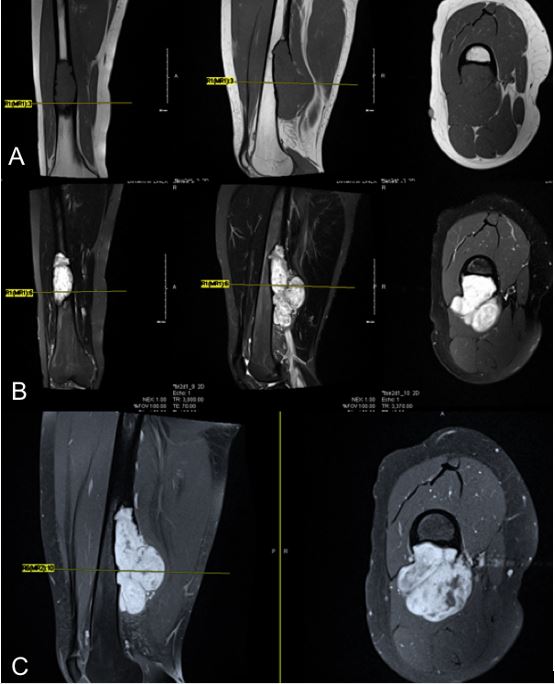
Plain xrays were not done at presentation and an outside MRI (Fig. 1) showed aggressive features with massive soft tissue mass originating from the bone and extending posteriorly. It measures 12 x 5 x 5cm and it is abutting the femoral vascular bundle. It has heterogenous enhancement in post gadolinium images and there is no evidence of skip lesions. At this point, the lesion looks aggressive and sarcoma was in the differential diagnosis.
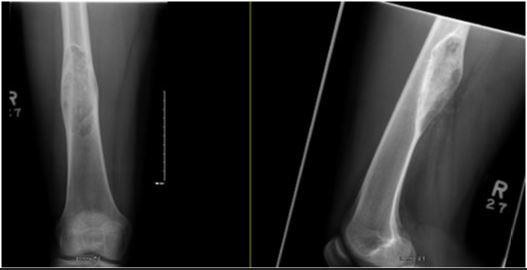
On plain radiograph (Fig. 2), the lesion was more benign looking, diaphyseal, geographic and lytic with sclerotic rim. The intramedullary canal looks narrowed and no deformity of the bone is seen. There are no signs of periosteal reaction, however, there is a significant soft tissue component extending posteriorly.

After the above information, differential diagnosis was non specific including chondromyxoid fibroma or more malignant surface osteosarcoma. Other pathologies could not be ruled out. CT chest showed small nodules that need a repeat follow up and could not confirm metastasis. Bone scan showed increased uptake in the bone and soft tissue lesion that could be malignant (Fig. 3).

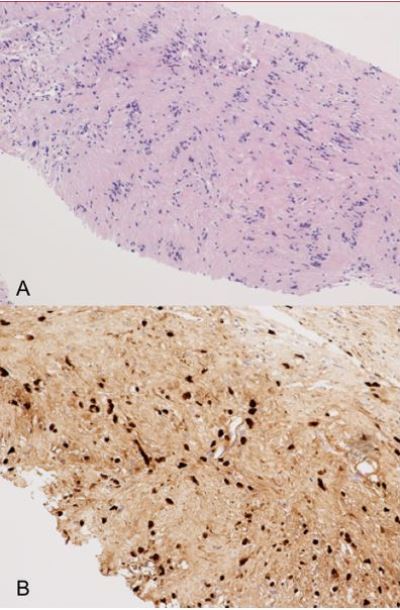
Ultrasound guided biopsy revealed mildly hypercellular spindle cell lesion. There is prominent nuclear palisading (Verocay bodies-Antoni A) and less cellular Antoni B areas. No mitosis was identified. Immunohistochemistry studies were positive for S-100 protein and CD34. The pathology was typical for schwannoma (Fig. 4).
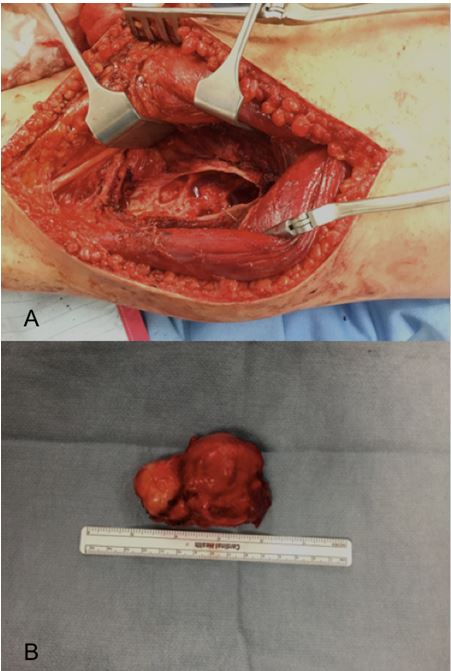
Patient had curettage and bone grafting through posterior approach. Extensive curettage was followed by high speed burr and irrigation. The soft tissue component was resected en bloc whereas the bone component was curettaged. There was a big posterior defect, however, most of the anterior part of the anterior cortex was intact and did not require fixation. The pathology was confirmed after tumor resection and the soft tissue component measured 8.3 x 4.9 x 4.2cm and the remaining aggregate volume was 5.7 x 6.5 x 1.7cm (Fig. 5 and 6).
Literature Review
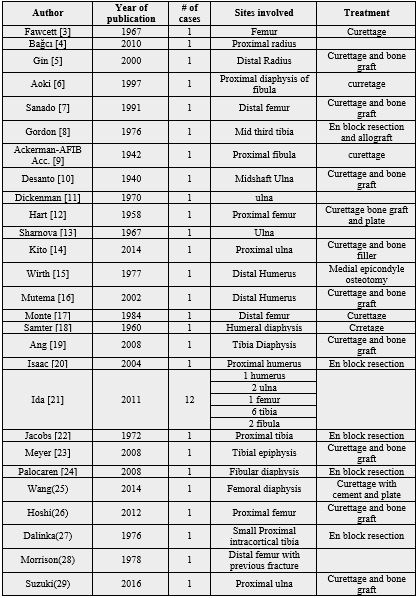
We used PubMed search and google scholar electronic databases to identify all published intraosseous schwannoma involving the long bones including: Humerus, Ulna, Radius, Femur, Tibia and Fibula. The more common intraosseous schwannoma (IS) involving the mandible or other small and flat bones were excluded. Exclusion also included: all malignant peripheral nerve sheath tumor, benign pathology like neurofibroma or lesions that are parts of syndromes like Carney Complex or neurofibromatosis disease.
Results
We could identify 39 cases published in the literature with confirmed intraosseous schwannoma involving long bones including our case (Table 1). The most commonly involved bone is tibia with 28.2% (11 cases). Other bones involved are (femur 9, ulna 7, humerus 5, fibula 5 and radius 2). Most of the cases involved the metaphyseal and diaphyseal part except one involved the tibial epiphysis. Four cases were intracortical lesions including our case. One of the tibial cases developed recurrence after curettage and bone graft.
Discussion
Intraosseous schwannoma is a rare entity. it should be included in the differential of geographic lytic bone lesions. It can involve any part of the long bone. Range of the size can differ according to the point of time it is found. It can be painful or cause pressure symptoms depending on the size of the lesion. It can start from the bone and extend outside as soft tissue component.
Our case is the largest intracortical schwannoma lesion identified in literature with huge soft tissue component. A similar case was published in radiology literature with very similar features and finding, however, the lesion is smaller than our case. Schwannoma was not included in the differential diagnosis until the biopsy was done and showed the typical picture of Conventional Schwannoma [25]. In our case, the soft tissue component was way bigger than the intraosseous part and was confusing for malignancy especially after the MRI findings.
Intraosseous schwannoma is not common reason for lytic bone lesions but reported cases were identified and very rarely cause pathological fracture. malignant transformation in Schwannoma in general is very rare and only reported cases in literature were found. We could not identify any published case with malignant transformation of schwannoma from long bones [28]. One patient with cervical intraosseous schwannoma had malignant transformation to MPNST (malignant peripheral nerve sheath tumor) [30].
Conclusion
Intraosseous schwannoma should be included in the differential diagnosis of geographic bone lesions. They are mainly found incidentally and treatment should be guided by understanding patients’ expectation and needs. We recommend biopsy when the diagnosis is doubtful and possibility of malignancy is raised according to radiological finding.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!