Biography
Interests
Dr. Henrique Mansur Gonçalves1,2*, Dr. Isnar Moreira de Castro Junior2, Dr. Max Rogério Freitas Ramos3, Dr. Cesar Barbosa Gonçalves4, Dr. Yonder Archanjo Ching San Junior5 & Dr. Flavio Carvalho Cruz5
1M.D., MSc., School of Medicine of Federal University of the State of Rio de Janeiro, Rio de Janeiro - RJ, Brazil, Brasília Air Force Hospital, Brasília - DF, Brazil
2M.D., Foot and Ankle Department, National Institute of Traumatology and Orthopedic, Rio de Janeiro - RJ, Brazil
3PhD., Department of General and Specialized Surgery, Federal University of the State of Rio de Janeiro, Rio de Janeiro - RJ, Brazil
4M.D. Foot and Ankle Department, Navy Hospital Marcílio Dias, Rio de Janeiro - RJ, Brazil
5M.D., MSc., School of Medicine of Federal University of the State of Rio de Janeiro, Rio de Janeiro - RJ, Brazil
*Correspondence to: Dr. Henrique Mansur Gonçalves, M.D., MSc., School of Medicine of Federal University of the State of Rio de Janeiro, Rio de Janeiro - RJ, Brazil, Brasília Air Force Hospital, Brasília - DF, Brazil.
Copyright © 2018 Dr. Henrique Mansur Gonçalves, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Ankle sprains are very common injuries, especially in athletes. Most of the time, conservative treatment provides complete recovery of symptoms. However, approximately 3,0% may lead to anterolateral impingement, a common cause of chronic joint pain and functional ankle instability.
Twenty-six patients, of which 76,9% were women, underwent arthroscopy debridement of the anterolateral impingement. The mean age was 38,5 ± 10,7 years. Mean time between injury and surgery was 33,1 months, with a mean follow-up of 31.2 months (between June 2008 and February 2015).
The mean of postoperative AOFAS score was 84.5 points and the median of pain scale was equal to 2. A quantity of 92,3% of the patients stated they were satisfied with the surgery performed and 84,6% of the patients had improvement of the functional instability. There was no statistically significant difference between the postoperative AOFAS score and classification of pain of patients with time between injury and surgery less than 24 months and greater than or equal to 24 months (p-value = 0.169, Mann-Whitney Test, and p-value Fisher’s exact test = 1,000, respectively). There was no statistically significant difference between the postoperative AOFAS score and classification of pain of patients with postoperative time less than 24 months and patients with postoperative time greater than or equal to 24 months (p-value = 0.085 Mann-Whitney Test, and p-value = 0,063, Fisher’s Exact Test, respectively).
Chronic pain and functional ankle instability can be treated simply by arthroscopic debridement of the anterolateral impingement. Good outcomes of the surgery, low pain scores and high AOFAS scores are independent of patient’s gender, injury side, time between injury and surgery and postoperative time.
Introduction
The lateral ligament complex of the ankle - anterior talofibular ligament (ATF), calcaneofibular ligament (CFL) and posterior talofibular ligament (PTFL) - is the structure most frequently damaged in sports, representing 13% to 56% of the lesions. The sprains that compromise the lateral ligaments correspond to 85%, with the trauma mechanism being supination and inversion of the foot, which is in plantar flexion with external rotation of the tibia [1-3].
Most of these lesions are treated conservatively with symptom improvement in up to 80% of cases [3]. However, from 10 to 40% of the cases develop chronic pain and instability [2,3]. Instability associated with lateral ankle sprain (LAS) can be classified into three types: mechanical, functional, and both mechanical and functional [4]. Mechanical instability is a deviation from the normal physiological range of motion. In contrast, functional instability (FI) is instability of ankle joint when the normal mechanical constraints are intact [5].
After an acute ankle sprain, 32-47% of patients report functional ankle instability [6-8]. It is characterized by symptoms of giving way, instability, or resprains (or a combination of these) [9]. Indeed, proprioceptive ability, postural control, strength of ankle muscles, and feedback (reflex-mediated) and feedforward (anticipatory) neural control have all been shown to be impaired in FI [10-12]. Although the mechanisms for this condition are not clearly understood, several pathologic factors have been associated with FI [13].
Approximately 3% of patients suffering from ankle sprains do not have mechanical changes, [14] however develop FI and anterolateral impingement due to the interposition of hypertrophic tissues or ruptured ligaments in the lateral gutter and anterolateral region of the ankle [15]. Some studies cite three types of soft tissue impingement: (I) meniscal injury, (II) synovial hypertrophy (more frequent) and (III) distal fasciculus of the anteroinferior tibiofibular ligament [13,15-17].
The careful physical examination, with semiological maneuvers as anterior drawer and medial subtalar glide tests, can differentiate mechanical from functional instability [3,4]. Complimentary exams like radiographics under stress can also help with this differentiation [4]. Magnetic resonance imaging is the most specific examination. Arthro-resonance and arthrotomography can increase the diagnostic accuracy, the last being considered the gold standard for the anterolateral impingement diagnosis [18].
Failure of conservative treatment, with persistence of the symptoms, such as giving way, persistent pain and muscle weakness, after 3 to 6 months of physiotherapeutic treatment, indicates surgical treatment [3]. The techniques can be open or arthroscopic, with anatomic and non-anatomic ligamentoplasty or the arthroscopic resection of the impingement, without ligamentoplasty [19].
The purpose of the present study is to assess the clinical results of the arthroscopic resection of ankle anterolateral impingement. We wish to investigate whether pain and functional instability can be treated simply by resection of the anterolateral impingement, whether there are differences in outcome over time between injury and surgery and in relation to the time of the postoperative period.
Methods
We evaluated all patients submitted to arthroscopic resection of the anterolateral ankle impingement with pain and functional instability, between February 2008 and October 2014, in this prospective study. The study was performed after approval by the research ethical committee. The diagnosis of functional instability was made throughout the history of at least two lateral ankle sprains in the same ankle and reported symptoms of giving way or instability. Each episode must have resulted in pain, swelling, limited weight bearing, a failure to return to pre injury function and repeated episodes of ankle spraining. Were included all patients that undergo at least three months of physical therapy and a minimum follow-up of sixteen weeks postoperatively. We performed the anterior drawer, talar tilt and medial subtalar glide tests to assess mechanical instability. Patients with positive scores in either test were excluded from the study because of mechanic instability. Participants with neurologic disorders or associated lesions, such as osteochondral lesions in the talus were excluded. Also were excluded the patients who underwent different surgical techniques, like ligamentoplasty, besides who did not keep the aforementioned follow-up and those with incomplete records.
Twenty-six patients were selected and answered a questionnaire, showing demographic and lesion characteristics. They also responded if they were satisfied with the surgery and quantified the pain in the ankle, by the analog pain scale (varying from 0, no pain, to 10, worse pain ever felt by the patient). The functional result was quantified by the application of the AOFAS score for hindfoot and ankle [20-22]. Moreover, after the operation, we consider persistence of functional instability if the patients reported any new episode of ankle sprain or symptom of giving way or instability.
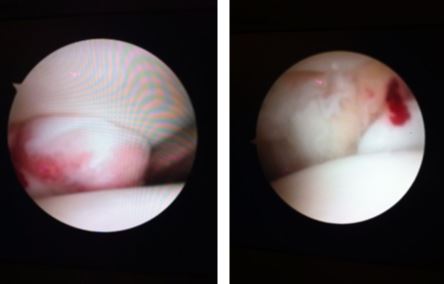
Surgery was performed under regional and peripheral nerve block and a thigh tourniquet. The operated limb was placed in a holder located under the knee with a 90-degree flexion and a distractor at the ankle. A 2.7 mm arthroscope was introduced through the standard anteromedial portal. After routine joint inventory, an anterolateral portal was made and used for debridement of all hypertrophic synovial and scar tissue in the anterolateral gutter with a 2.9 mm shaver blade.
All patients were discharged one day after surgery, wearing a plaster cast, and were kept non-weight bearing. After two weeks, stitches were removed and protected and progressive weight bearing was allowed over the following four weeks with ankle support orthosis and elastic stocking. In the sixth week, total load was allowed and physiotherapy started with exercises of proprioception, kinesiotherapy, analgesia and fibular strengthening.
For statistical analysis of the variables, we used the non-parametric Mann-Whitney test and the chisquare and Fischer’s exact tests for qualitative variables, at level of significance 0.05. Statistical analysis was performed with the IBM SPSS program (Statistical Package for the Social Science), version 22.0.
Results
Out of the 26 patients evaluated, six were male (23,1%) and 20 were female (76,9%). Regarding the affected side and the foot format, there were 12 cases in the right ankle (46,2%) and 14 cases in the left ankle (53,8%), 22 cases (84.6%) had good alignment (plantigrade) and four cases (15,4%) had flat feet. Six patients (23,1%) were athletes, of which five were amateurs and one was a professional. Five patients (19,2%) were smokers and four (15.3%) reported frequent alcohol drinking.
Figure 2 shows the frequencies of the trauma mechanisms. The most typical cause of injury was the fall. This mechanism generated the lesion in 53.8% of the cases.
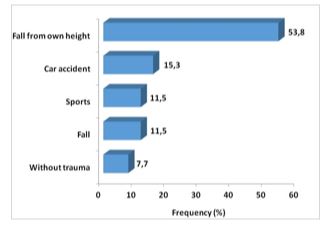
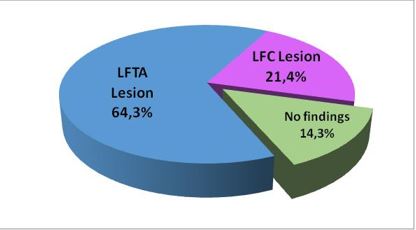
Figure 3 shows the frequencies of magnetic resonance findings, performed by 11 patients. The LFTA lesion is the most prevalent diagnosis (64.3%), however all of the patients had clinically stable ankles.
The patients’ ages ranged from 22 to 63 years, which resulted in an average of 38.5 years, a median of 40.5 years and a standard deviation of 10.7 years.
The time between injury and surgery ranged from 14 to 72 months in the sample. This distribution resulted in an average of 33.1 months, a median of 30 months and a standard deviation of 15.5 months. Postoperative time ranged from four to 74 months in the sample, which resulted in an average of 31.2 months, a median of 31.5 months and a standard deviation of 20 months.
In postoperative analysis, the pain scale scores ranged from 0 to 4, with median 2 and typical or modal score 2. The postoperative AOFAS scores ranged from 70 to 100 points, which resulted in an average of 84,5 points, median of 80 points and standard deviation of 6.9 points. All 26 patients complained of chronic pain and reported symptom of giving way or instability before surgery. After surgery, 22 patients (84,6%) reported improvement of the symptoms and had no new sprain. Two (7,69%) patients had new sprain and other two (7,69%) referred residual giving way symptom, despite improvement of the pain and no new sprain reported.
As complication, we had five (19%) patients with postoperative pain, who showed improvement after physiotherapy. There were no important complications such as infection or neurological injury. Finally, when questioning about patient satisfaction, 92.3% were satisfied with surgery. The two patients (7.7%) that were not satisfied were the same that had new episodes of ankle sprain after the surgery.
There were seven patients (26.9%) who had time between injury and surgery less than 24 months and 19 patients (73.1%) greater than or equal to 24 months. There is no significant difference in the postoperative AOFAS between theses subgroups (P-value = 0.169, Mann Whitney Test). Moreover, the association between pain and these subgroups is not statistically significant (p-value of Fisher’s exact test equals 1,000). Table 1 summarizes the results found for each of these groups and overall.
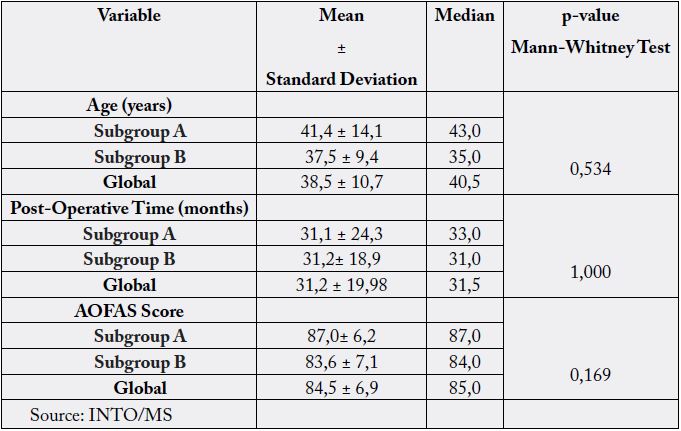
In the sample, nine patients (34.6%) had a postoperative follow-up less than 24 months and 19 patients (73.1%) with a follow-up greater than or equal to 24 months. The p-values obtained, all higher than 5%, allowed us to conclude that there is no significant difference between the postoperative AOFAS score of patients with postoperative follow-up less than 24 months and greater than or equal to 24 months (p-value = 0.085, Mann Whitney Test). In addition, the association between pain and these subgroups is not statistically significant (p-value of Fisher’s exact test equals 0.063). Table summarizes the results found for each of these groups and overall.
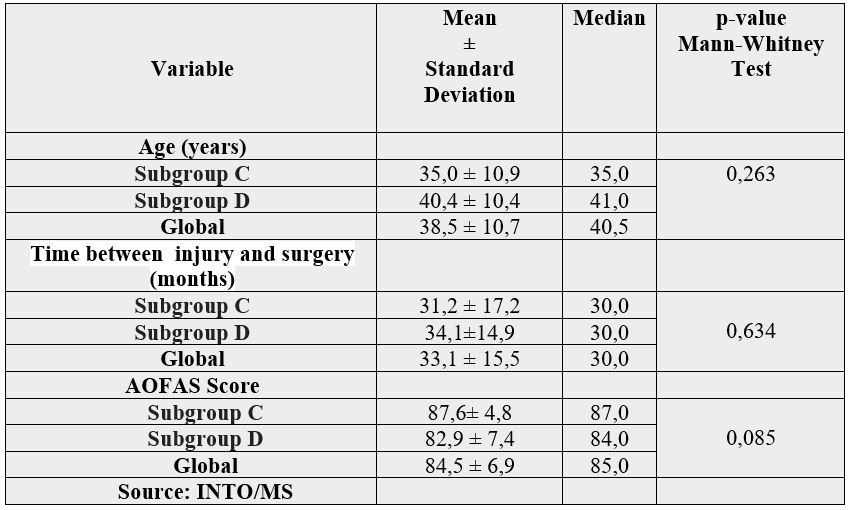
Table 3 presents the database, with a description of the main variables of the 26 patients.
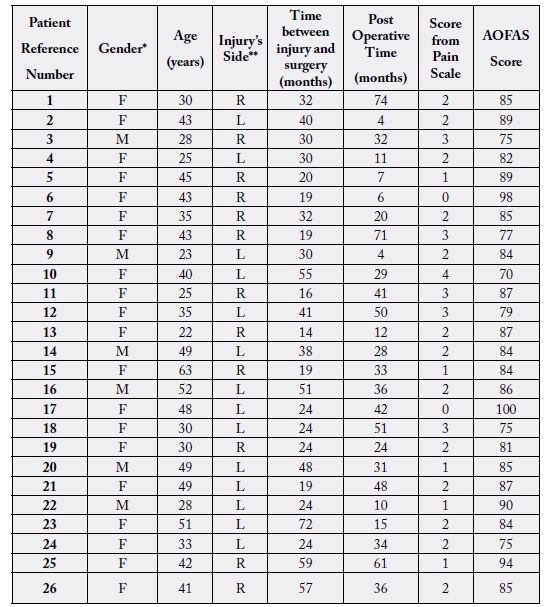
* F= Female, M=Male
** L= Left, R= Right
Discussions
Approximately 3% of all lesions with ankle inversion cause soft tissue impingement resulting from obliteration of the anterolateral recess by synovial hyperplasia, secondary to bleeding and / or abnormal scarring of the anterior talofibular ligament [13]. This impingement is a common causes of chronic lateral or anterolateral pain in the joint and can led to functional instability of the ankle [13,15].
Several surgeons suggest that arthroscopy must be performed in surgeries to correct instability, regardless of the technique chosen, because it is a safe and effective technique [23-24]. The rate of good and excellent results in the treatment of anterolateral ankle impingement through arthroscopic resection varies in the literature between 74-96.7% [15,16,25-30]. However, most articles had a short-term follow-up period, of up to 24 months [16,25,27,29,31].
In the present study, we obtained a final mean of the AOFAS score of 84.5 with an average follow-up of 31.2 months, considered mid-term. In order to answer the question about a possible difference in outcome over time in the postoperative period, the statistical analysis between the AOFAS score of patients with postoperative time less than 24 months and greater than or equal to 24 months showed that there was no significant difference (p-value = 0.085). Leading us to conclude that the good results with the arthroscopic debridement of the anterolateral impingement remain, at least, with mid-term follow-up.
There were few articles in the literature with postoperative follow-up of mid-term [15,26] and long-term [23,32]. Ferkel [26] had a mean follow-up of 33.5 months, Kim [15] 30 months, while Buda [32] and Urgüden [23] had a follow-up of 90.1 and 83.7 months, respectively. In the study of Urgüden [23] with 41 patients, their final AOFAS score was 89.6. Kim [15] reported 94% of good and excellent results. Ferkel [26] suggests with his results that arthroscopic treatment is successful in relieving pain and disability caused by the anterolateral impingement in a high percentage of patients whose symptoms have failed to respond to prolonged conservative therapy (2 years in the series). The only author that reported results at different stages was Buddha [32]. In his retrospective study, he analyzed the results of arthroscopic debridement of soft tissue impingement of the ankle. The patients were evaluated clinically presurgery, after 24 months, at 48 months and at the final follow-up at a minimum of 6 years from the surgery. The author reports a remarkable improvement in the AOFAS score with values ranging from 40.6 ± 21.2, 82.6 ± 17.9, 78.4 ± 17.3 and 74.8 ± 24.3, respectively. Of the 42 patients included in the study, only 10 had anterolateral impingement and, according to Buda [32], these patients had good and excellent clinical outcomes.
In this study, we obtained a total of 96.1% of good or excellent results and 92.3% of patients declared satisfied with the surgery. However, it must be emphasized that the great majority of studies do not adopt such strict selection criteria. El-Sayed et al. [16] had 85% of good or excellent results, in a total of 20 patients, with a follow-up of 21.3 months, and 35% of their patients had associated lesion in the cartilage of talar domus. Koczy et al. [28] reported an increase in the AOFAS score from 75.4 points to 90.6 and 92, after 6 and 12 months postoperatively, respectively, in 22 operated patients. Out of these, seven had reported a previous fracture of the lateral malleolus and two had a diagnosis of isolated rupture of tibiofibular syndesmosis.
Mardani-Kivi [27] presented 91.3% of good to excellent results after 6 months postoperatively of arthroscopic debridement of the anterolateral impingement, with a significant improvement of the AOFAS score, from 59.21 in the preoperative period, to 88.13. In the same article, the author compares patients with or without chondral lesions in the talus, and concludes that although the findings show negative effects of chondral lesions, the results were not statistically significant. In our study, unlike all the studies cited, we evaluated only those patients with anterolateral ankle impingement who presented functional instability, excluding all patients with associated lesions, such as osteochondral lesions on the talus or other types of ankle impingement, as well as patients with mechanical instability.
In the present study, there are several limitations, among them the low number of patients, the absence of a control group and the lack of a preoperative evaluation. The limited number of patients is due to our strict exclusion criteria, which standardized our sample, limiting a selection bias. Only 42.3% of the patients underwent preoperative MRI. However, as the indication of surgical treatment complied with our selection criteria through a thorough physical examination and the surgical technique proposed, one of the main advantages of arthroscopic route is the possibility of identifying associated intra-articular lesions, we do not consider such a complementary examination indispensable. According to some authors, [17,33-36] the sensitivity, specificity and accuracy of MRI are relatively low, with conflicting values in literature varying from 39-100% for sensitivity, and 50-100% for specificity. For Farooki [34] the sensitivity, specificity and accuracy of MRI for the diagnosis of anterolateral impingement were 42%, 85% and 69%, respectively. Liu et al. [35] had 39% sensitivity and specificity of 50% to predict impingement with preoperative MRI, and 94% and 75% with physical examination, respectively. These authors conclude their work by suggesting that preoperative MRI is not beneficial or cost-effective in the diagnosis of anterolateral impingement and may even delay treatment, defining the diagnosis of the pathology as clinical, which ratifies our methodology by using physical examination for the diagnosis and surgery indication.
Also, we do not use any Functional Ankle Instability Questionnaire. In fact, there are seven self-reported subjective questionnaires that appear frequently in ankle instability literature. However, no test or measure has been globally agreed upon to “diagnose” FI [37]. Recently, an investigation of these instruments, failed to significantly predict ankle instability [38].
There are several positive aspects in our work, among them we can mention, the prospective nature, the uniformity of the patients, the same surgical technique performed for all patients and a mid-term follow-up. Besides, all patients were evaluated by the main author, who was not the main surgeon in any of the cases evaluated, avoiding selection and judgment biases.
There are various theories postulated as to why patients may have ongoing symptoms of functional instability following ankle injuries [39]. In the absence of changes in the normal range of motion of the joint, it has been suggested that, after an episode of ankle sprain, the he ligaments are injured, but they heal, keeping the joint mechanically stable. However, the resulting scar or ankle impingement leads to the feeling of instability during mobilization and does not allow the ankle to function as well under normal physiological loading [40].
This theory has not been fully explored so far. Despite the pain caused by the intra-articular impingement syndrome been successfully treated with arthroscopic debridement, [23,26,31,40] it has not been proved that the resection of the anterolateral impingement can also treat the FI of the ankle. In our study, different from previous studies, we evaluated the improvement of FI after arthroscopic resection of the anterolateral impingement and had 84,6% of the patients reporting no new sprain or the symptom of giving way.
In conclusion, our study supports the role of arthroscopic resection of the anterolateral impingement in the treatment of functional ankle instability. We have shown that a large proportion of patients can be expected to improve pain, the AOFAS scores and FI, avoiding more morbid and expensive procedures like ligamentoplasty.
Conclusion
The pain and functional chronic instability of the ankle can be treated simply by the arthroscopic resection of the anterolateral impingement. The arthroscopic debridement presents low complication rates, high satisfaction rate, typically low pain scores and high postoperative AOFAS score, depicting optimal ankle function.
Moreover, the present study showed that the good results of the surgery, the low pain scores and high AOFAS scores, are independent of the patient’s gender, the injury side, the time between injury and surgery and the postoperative time.
Conflicts of Interest
None
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!