Biography
Interests
Dr. Khaled Alawany
Consultation Orthopaedic Surgeon, Dr Sulaiman Alhabib Hospital, UAE
*Correspondence to: Dr. Khaled Alawany, Orthopaedic Traumatology Department, Consultation Orthopaedic Surgeon, Dr Sulaiman Alhabib Hospital, UAE.
Copyright © 2018 Dr. Khaled Alawany. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Hip Dysplasia with Acetabulofemoral CAM impingement treatment through minimal invasive Hip arthroscopy.
In the Case study I show using Hip arthroscopy to treat the CAM impingement in acetabulofemoral type, in Dysplastic Hip several degenerative changes appears in the hip regarding the Osteoarthritic changes and Labrum degenerations.
In this Case of Female young Patient I treated the degerative Labrum and CAM impingement through partial resection of the Femur neck, with Capsule release and resection of calcified soft tissue in the Acetabulum rim.
Short term follow up shows a good result in:
1.Decrease in Pain
2. Increase rang of movement
3. No limping on the leg.
Introduction
Hip dysplasia is a treatable developmental disorder that presents early in life but if neglected can lead to chronic disability due to pain, decreased function, and early osteoarthritis. The main causes of hip dysplasia in the young adult are residual childhood developmental dysplasia of the hip (DDH) and adolescent-onset acetabular dysplasia. These two distinct disease processes affect the growing hip during different times of development but result in a similar deformity and pathomechanism of hip degeneration. Routine screening for DDH and counseling regarding risks for acetabular dysplasia in families with a history of early hip osteoarthritis may allow early identification and intervention in these hips with anatomical risk factors for joint degeneration.
Hip dysplasia is a dynamic, mechanical disorder that causes structural damage to the hip. Abnormal hip anatomy results in abnormal hip mechanical behavior, which in turn, causes more anatomical abnormalities. Hip dysplasia is an unstable ball-in-socket hip joint that is characterized by a shallow acetabulum that does not cover the femoral head sufficiently. This anatomical aberration produces instability of the hip and increased mechanical stress at the acetabular rim, leading to hypertrophy and tearing of the fibrocartilaginous acetabular labrum and more rapid degeneration of the hyaline articular cartilage. If left untreated, hip dysplasia will cause pain, decreased function, and eventually result in hip osteoarthritis.
The incidence of hip dysplasia is reported to range from 1.7 to 20 % in the general population, with most studies finding the incidence between 3 and 5 % [1-5] Females have a two to four times increased relative risk of hip dysplasia [4,6,7] but males with hip dysplasia tend to have a higher incidence of concomitant hip deformities such as acetabular retroversion and a CAM deformity at the femoral head-neck junction that may need additional consideration during hip dysplasia surgery to prevent iatrogenic creation of femoroacetabular impingement . A family history of hip dysplasia also increases the relative risk of having hip dysplasia by 1.4 to 1.7 % [4,6,7]. More than 50 % of patients with hip dysplasia have a positive family history of hip disease [8].
Hip dysplasia is the leading cause of early onset hip osteoarthritis before the age of 60 years [1,9-12]. In a recent study of patients under 50 years old undergoing total hip replacement for osteoarthritis, 48.4 % were found to have underlying hip dysplasia as the etiology of hip osteoarthritis [12].
In general, the more severe the dysplasia, the higher the risk is of developing osteoarthritis. Globally dysplastic hips with combined deficiencies in both anterior and lateral coverage have a higher risk of incident osteoarthritis, with an odds ratio of 5.45 compared to 2.26 if only lateral undercoverage is present [13].
The occurrence of a tear of the acetabular labrum, the fibrocartilage ring at the acetabular periphery that provides compensatory hip stability and which is subjected to higher mechanical stresses with acetabular rim loading in hip dysplasia [14], also increases the risk of osteoarthritis [15].
Structural Damage
CT and MRI studies have demonstrated that dysplastic hips have less surface contact area between the acetabulum and the femoral head as compared to normal hips. Using MRI, Steppacher and colleagues found the articular cartilage surface area in the dysplastic acetabulum to be 16 % smaller than normal [16]. The dysplastic hip’s smaller acetabular cartilage surface area results in a 26 % smaller cartilage contact area between the acetabulum and the femoral head, which causes a 23 % increase in contact pressure within the joint [17]. Subluxation of the femoral head, if present, further decreases contact area between the acetabulum and the femoral head, compounding the already elevated joint contact pressure.
Over time, the increased cartilage contact stresses cause early cartilage degeneration. Compared to normal hips, dysplastic hips have higher peak and cumulative contact stresses. Mavcic and colleagues followed 58 asymptomatic hips with acetabular dysplasia for a minimum of 20 years and compared them to 48 hips without disease [18]. They found that cumulative contact stress was the best predictor of developing osteoarthritis and that the prevalence of osteoarthritis in patients with dysplasia at age 58 was the same as in patients with normal hips at age 68. Linear extrapolation data demonstrated that the normal hips would only achieve dysplastic-level cumulative contact stresses at the age of 90 years. In other words, dysplasia effectively causes “premature aging” of the hip.
Since the rim of the dysplastic acetabulum is abnormally located directly superior to the femoral head, within the main weight-bearing zone of the hip joint, structural damage develops at the acetabular rim where abnormal loading causes concentrated contact stress, resulting in degenerative labral tears, full-thickness labral tears, intra-substance labral ganglions and paralabral cysts, and acetabular rim bone cysts and fractures [14,19,20]. Contact stress increases with worsening severity of acetabular dysplasia [21]. Severity of dysplasia is commonly measured by the lateral center edge angle (LCEA), which is formed by two lines from the center of the femoral head to the lateral edge of the roof of acetabulum and directly vertical, respectively. LCEA reflects the severity of dysplasia by measuring the degree of lateral femoral head coverage by the acetabulum. A similar measurement, which requires “false profile” radiographic views of the hip, is called the anterior center edge angle (ACEA), which reflects anterior coverage insufficiency in dysplasia. LCEAs less than 25° have been associated with a 4.3-fold increased risk of incident radiographic osteoarthritis [22] and increased risk of progression of such osteoarthritis over time [23]. Thomas and colleagues found that with each degree decrement in LCEA less than 28°, there was a 13 % increased risk of osteoarthritis and an 18 % increased risk of future total hip replacement [24].
Clinical Presentation and Diagnosis of Hip Dysplasia in Young Adults
The most common presenting symptoms of acetabular dysplasia in the skeletally mature individual are insidious onset of activity-related groin pain and/or lateral hip pain [25]. Matheney and colleagues recently found that severe dysplasia (LCEA˂5°) and high activity level (UCLA score 8–10) are independent predictors of younger patient age at presentation for surgical treatment [26]. Diagnosis is made through physical exam and radiographic findings. Up to 48 % will have a limp during gait and 97 % have a positive anterior impingement test [25]. Anteroposterior pelvic radiographs show a LCEA less than 25°, an ACEA less than 20°, and a more obliquely oriented sourcil, or weight bearing roof of the bony acetabulum, with an elevated Tönnis Angle greater than 10° [27,28].
Treatment
The periacetabular osteotomy (PAO) was first described by Professor Reinhold Ganz nearly 30 years ago and has become the treatment of choice for symptomatic acetabular dysplasia in the skeletally mature patient [29]. The PAO allows complete reorientation of the acetabulum to provide more lateral and anterior femoral head coverage by the acetabulum, reduce hip subluxation and medialize the hip joint center, redistribute the high contact stresses from the acetabular rim to the entire articular surface, and to transform the dysplastic hip’s shear stresses across the articular cartilage into compressive stresses that are more favorable for cartilage longevity [21,30].
In this case, the patient is treated surgically through Hip arthroscopy for Cartilage, Labrum evaluation,debridment of the labrum and refixation of torn part and excision of Osteophytes on the Acetabulum rim and partial resection of the femur neck by CAM impingement.
39 years old Female, 165cm tall, 85kg weight, not working, no health problems, no medication, family history of joint osteoarthritis (Dysplastic joints is unknown through her family).
The patient started to have pain in the right groin since 05.2017, no history of trauma, the patient increases with standing and walking, after long time walking she starts limbing on her right leg, no rest pain, pain with driving or sitting when she flex the hips.
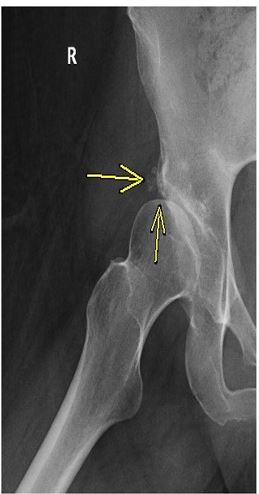
After 2 months from start of pain she was investigated through Xray hips in 2 views AP.Lat
Laboratory CBC, CRP, Uric Acid, Rheumatoid factor, ESR.
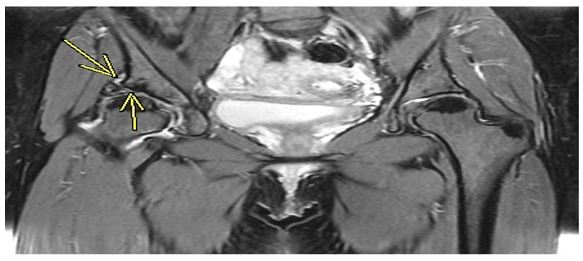
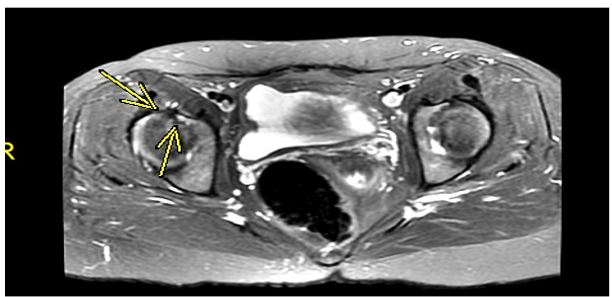
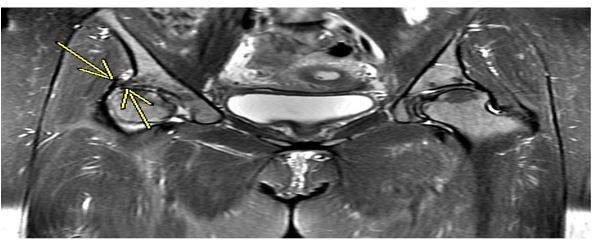
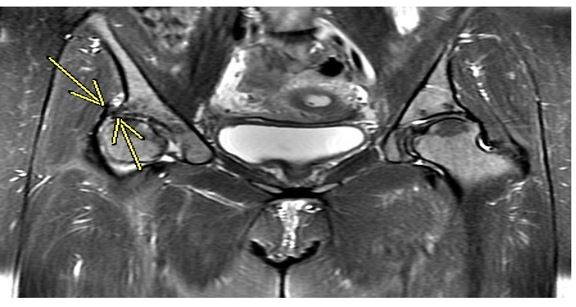
MRI Hips
Bilateral ovoid morphology of the femoral heads, under-coverage by the acetabula, and with lateral subluxation on neutral view. This suggests congenital hip deformity/coxa valga. Clinical correlation should be made.
A chronically displaced small ossific density is seen along the lateral aspect of the right acetabulum, query prior trauma, versus degenerative.
Mild right hip arthritic changes.
Trace right greater trochanteric spur.
No plain radiographic evidence of acute fracture or dislocation.
No visible suspicious osseous lytic or blastic lesions.
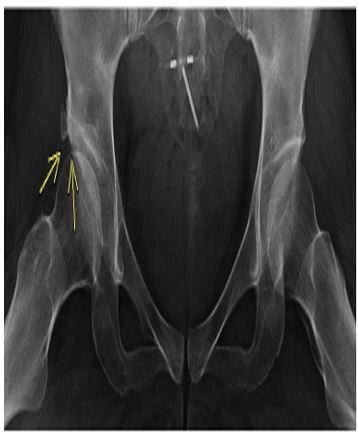

1. Imaging findings compatible with developmental hip dysplasia, more on the right, and likely predisposition to femoroacetabular impingement. Clinical correlation should be made, and also consider whole lower limb XR correlation.
2. Chronically displaced small ossific fragment of the lateral aspect of the right acetabulum, possibly from impingement/impaction injury.
3. Mild-moderate right hip arthritic changes.
4. Mild-moderate right, and mild left hip joint fluid.
WBC 4.9, HB 10.1, CRP 1, ESR 16, Uric acid 3.5, Rheumatoid F less than 10.
Right Hip Pain by Acetabulufemurar impingement, mild osteoarthritis, Labrum degeneration by Hip Dysplasia causing Ossific fragment on the Acetabulum Rim.
1. Rest avoid long time standing and long-time walking and rotation of the Hip joints.
2. Antiinflammatory medication (Loxoprufen) Muscle relaxant (Tolperisone 150) with PPI (Esomeparazole).
Slight improvement, still limping on her right leg, night pains in the right Groin.
3- C-arm Guided intra articular injection of (a. xylocain2%, b. Steroid (Kenalog40mg), c. Hyaloronic acid).
Time of injection 30.09.2017.
1. After 1 week from Injection:decreased, pain in sitting, night pain decreased, limping only after vlong time walking.
2. Follow up in 4 weeks: pain increased, Rang of movement of the right hip limited because of pain, mechanically free rang of movement, limping after ling time walking.
3. Follow up 3 months: patient has continues pain , limping with short time standing and walking, Rang of movement is limited in all direction because of pain.
As patient had short term improvement after Steroid, Hyaloronic Acid injection intra articular It is indicated to Surgical treatment:
Hip Arthroscopy Diagnostic, Chondroplasty, Labrum debridment and or Refixation of Torn part, Resection of Ossified Fragment on acetabular Rim, Capsule release, Partial synovectomy, partial resection of Femur neck.
Date of Surgery: 04 April 2018
Surgery Duration: 120 minutes
Surgery Special Needs: C-Arm, Traction table, Optic 70 and 30 degree, Curved soft tissue shaver, arthroscopic cautery, arthroscopic Bullet cutter.
Number of Portals: 3 Anterior lateral and anterolateral portal.
1. Labrum degenerative tears superior, anterior.
2. Mild to moderate Chondromalacia Acetabulum II degree, Femur CM I degree.
3. Loose soft tissues in intra articular space.
4. Mechanical Acetabulofemural impingement.
5. Hip joint capsule hypertrophy, mild Synovialitis.
6. Calcified triangular fragment intra capsular superior on the acetabular rim.
3rd generation cephalosporins, NSAID, Subcut Anticoagulant (Clexan 0.4).
1st Day: Pain on the site of portals, muscle pain (Quadriceps muscles).
7th Day: No pain, muscle sprain (Quadriceps muscles), full weight baring mobilization No assistive tools (Crutches).
21st Day: No Pain, no Muscle pains, no limping, full weight baring mobilization.
28th Day: Pain Score VAC 0, full rang of movement.

Conclusion
In this study, it shows that the hip right Pain caused by Hip dysplasia from Impingement component CAM, and degenerative changes on the Labrum with loose soft tissues intra articular.
Using the surgical treatment with minimal invasive Hip arthroscopy to make Capsular release and resection of Ossified fragment with partial resection of the Femur neck, improve the rang the rang of movement of the hip joint and the debridement of degerative Labrum helps to decrease strain over the Labrum which play role on decrease pain on the Hip joint.
Long term study for 6 months and 12 months is needed to evaluate the radio-graphic changes on the hip joint in comparison to the other side which has dysplastic changes without symptoms [31-33].
Recommendation
Hip joint arthroscopy as surgical option in treatment of Hip Pain by Hip
Dysplasia can be method of choice to delay process of Cartilage degeneration.
Specially in mild to moderate hip osteoarthritis, with CAM impingement.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!