Biography
Interests
Dr. Hala El-Hadary1*, Dr. Dadour, N. M.2, Dr. Ahmed, H.3 & Dr. Moenes, D.3
1Consultant of Rheumatology & Immunology, Kasr El-Ainy, School of Medicine, Cairo University, Egypt
2Specialist of Rheumatology & Rehabilitation, Egyptian Fellowship, Cairo, Egypt
3Resident of Rheumatology & Rehabilitation, ELKatib Hospital, Cairo, Egypt
*Correspondence to: Dr. Hala El-Hadary, Consultant of Rheumatology & Immunology, Kasr El-Ainy, School of Medicine, Cairo University, Egypt.
Copyright © 2018 Dr. Hala El-Hadary, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Hypereosinophilic syndrome (HES) is a myeloproliferative disorder (MPD) characterized by persistent eosinophilia that is associated with damage to multiple organs.
Anderson first described the Peripheral eosinophilia with tissue damage in 1968. In 1975, Chusid defined the three features required for a diagnosis of hypereosinophilic syndrome: a sustained absolute eosinophil count (AEC) greater than >1500/μl, which persists for longer than 6 months, No identifiable etiology for eosinophilia and Signs and symptoms of organ involvement.
However, due to advances in the diagnostic techniques, secondary causes of eosinophilia can be identified in a proportion of cases that would have otherwise been classified as idiopathic hypereosinophilic syndrome.
Secondary eosinophilia is a cytokine-derived (interleukin-5 [IL-5]) reactive phenomenon. Parasitic diseases are the most common cause, whereas in developed countries world widely, but allergic diseases are the most common cause in developed countries. There are other causes such as: Malignancies, Metastatic cancer, Tcell lymphoma, colon cancer, pulmonary eosinophilia, Loffler syndrome, Churg-Strauss syndrome, allergic bronchopulmonary aspergillosis, Connective tissue disorders - Scleroderma, polyarteritis nodosa, Skin diseases, Dermatitis herpetiformis, Inflammatory bowel disease, Sarcoidosis and Addison disease.
Clonal eosinophilia is diagnosed by bone marrow histology, cytogenetics, and molecular genetics.Like Acute leukemia, PDGFRA (platelet-derived growth factor receptor, alpha polypeptide, PDGFRβ-rearranged eosinophilia, KIT-mutated systemic mastocytosis Myelodysplastic syndrome (MDS) etc.
Idiopathic eosinophilia is a diagnosis of exclusion when secondary and clonal causes of eosinophilia are excluded.
Introduction
Rheumatoid arthritis is a chronic inflammatory disorder that can affect more than just your joints. In some people, the condition also can damage a wide variety of body systems, including the skin, eyes, lungs, heart and blood vessels. The inflammation associated with rheumatoid arthritis is what can damage other parts of the body as well. While new types of medications have improved treatment options dramatically, severe rheumatoid arthritis can still cause physical disabilities.
Hyper eosinophilic syndrome (HES) is a term used to describe a wide variety of eosinophilic disorders without a known etiology [1]. The hallmark characteristics of this syndrome are a persistent eosinophilia combined with unexplained organ-system dysfunction [2,3]. HES has substantial clinical heterogeneity and a highly variable prognosis [4]. As late as the 1970s, HES was associated with an extremely poor prognosis with a mean survival duration of 9 months and a 3-year survival rate of only 12% [5]. Recent advances in the management of HES, including earlier diagnosis and improved management of cardiac sequelae, have extended survival in HES patients. We here present a case of a patient with long‐standing rheumatoid arthritis (RA) who developed idiopathic hyper eosinophilic syndrome (HES).
Case History
Female patient of age 46 years presented to fever, arthritis, angioedema and generalized bony aches for 2 months with history of Rheumatoid Arthritis for 18 years. She was on Methotrexate25 mg/week S.C. injection, prednisone 5 mg oral/day for 1 year then tapered it & NSAIDs with improvement. Off treatment for 4 years.
On examination there was swelling of all MCPs, PIPs both wrists and knees, puffiness of face, tender shoulders, Limited range of motion of right elbow, limitation of ROM of knees, all other findings were within normal limit. Family history was irrelevant, temp. 38°C rest of Vital signs were all normal.
Routine blood investigations showed mild hypochromic anemia HB 11.3gm/dl, marked leukocytosis 33.000ul, marked Eosinophilia 86%, absolute neutropenia, Anticcp positive high titer 212.6 U/ml, ESR 55mm/hr., CRP 74.2mg/l, CA125 normal, B-HCG quantitative normal, Urine culture showed growth of klebseila and E.coli, Rheumatoid factor positive high titer, rest of labs and autoimmune profiles were negative.
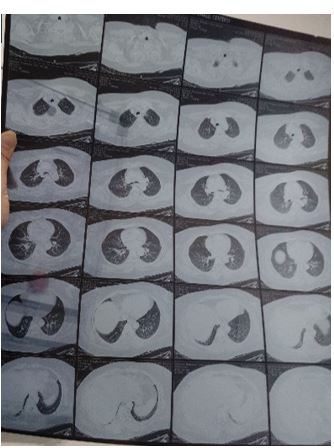
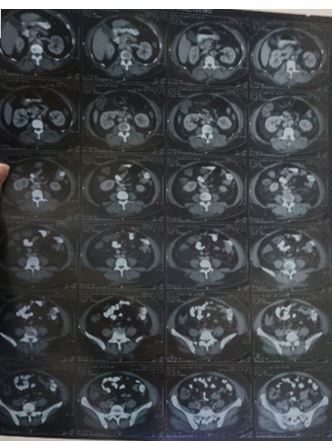
X-rays hands (Figure 1) showed multiple erosions, CT chest (Figure 2), Abdomen and pelvis (Figure 3) bilateral diffuse pulmonary ground glass densities, mild stranding of bilateral perinephric as well as mesenteric fat wit few subcentimetric mesenteric lymph node likely inflammatory sequel, right ovarian simple cyst, mild hepatosplenomegaly.
Patient was on broad spectrum antibiotic, antifungal, antipyretic and proton pump inhibitor.

Discussion
Idiopathic (Hypereosinophilic Syndrome) is a disease of exclusion. Eosinophilia in rheumatoid arthritis patients has been directly related to increased disease activity and various other extra-articular manifestations like rheumatoid nodules, vasculitis, neuritis, pulmonary fibrosis and cutaneous infarctions [6-8]. Our patient reported a deterioration in joint pains and swelling at the time of development of eosinophilia, hence it can be linked to increased disease activity.
Persistent eosinophilia can be found in 10 to 40% cases of rheumatoid arthritis [9]. Eosinophilia has been known to occur in patients receiving gold therapy in rheumatoid arthritis [10]. Gold therapy is no longer given these days. Although rare, articular manifestations of HES (Hypereosinophilic Syndrome) have been described in the past, mimicking features of rheumatoid arthritis [11-15]. Tay described ten patients of acute onset polyarthritis with hypereosiniphilia as “eosinophilic arthritis” [16]. Our patient already had long standing history of rheumatoid arthritis and so co-existence of the two diseases could be a possibility
Other causes of eosinophilia must be ruled out before a diagnosis of HES can be made. Common causes of secondary elevated blood eosinophilia include helminthic parasite infections, atopic and allergic diseases and adverse drug reactions. Stools examination ruled out parasitic infestation, our patient was off treatment for the last four years which ruled out drug reaction and no history of allergic or atopic diseases were present. Several other causes of eosinophilia exist including systemic rheumatic diseases e.g. Churg-Strauss syndrome (CSS), eosinophilic pneumonias, lymphoid malignancies and solid tumor neoplasia, systemic mastocytosis and primary immunodeficiency diseases, eosinophilic gastrointestinal diseases and nonhelminthic infections e.g. scabies, fungi and tuberculosis [17]. Primary skin diseases associated with blood eosinophilia include atopic disease, autoimmune blistering diseases such as bullous pemphigoid, cutaneous T-cell lymphoma, angiolymphoid hyperplasia and Kimura disease, eosinophilic cellulitis, panniculitis and vasculitis, and eosinophilic postural folliculitis [18]. Evidence of these disorders was ruled out by an extensive investigation program.
HES are a potentially lethal disorder. Most organ systems can be involved e.g. heart, vascular system, skin, central and peripheral nervous system, gastrointestinal tract, and eyes [19]. The symptoms are variable related to the organs involved and to the nature and severity of organ damage either caused by eosinophilic infiltration or thromboembolic events.
Controlling the eosinophilia in blood and tissue is important in order to prevent end organ damage from eosinophils. Despite improvements in medical management, HES remains a serious condition with a poor prognosis for the majority of patients. Currently available therapies for HES are not adequate; an effective, safe, and tolerable treatment option is required to minimize the morbidity and mortality associated with HES. A better understanding of eosinophil biology and HES pathogenesis has resulted in new therapies directed at novel targets.
Conclusion
This case holds importance as it is not only a rare case of hypereosinophilic syndrome with rheumatoid arthritis. It also highlights the importance of eosinophilia in rheumatoid arthritis. Steroids proved to be useful in treating eosinophilia in our patient.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!