Biography
Interests
Dalal Naeem, M. I.1 & Ravi Paul2*
1Department of Psychiatry, School of Medicine, University Teaching Hospitals Adult Clinic 6, Lusaka, Zambia
2Department of Psychiatry, School of Medicine, Consultant Neuropsychiatrist, University Teaching Hospitals,
Adult Clinic 6, Lusaka, Zambia
*Correspondence to: Dr. Ravi Paul, Department of Psychiatry, University Teaching Hospital, Zambia.
Copyright © 2019 Dr. Ravi Paul, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Despite progress in psychiatry and mental health, the treatment gap remains high in Zambia. A
study done in 2015 by Paul et al [1] looking into treatment seeking behaviours in mental health,
it was found that the Zambian culture, myths and stereotypes hinder open discussions regarding
mental health (MH) and its complications such as suicide which in seemingly on the rise [2]. A
holistic approach to treating MH involves a treatment model known as the biopsychosocial (BPS)
approach of management. The BSP uses a person centred view of illness, rather than simply a disease
centred one [3] Currently, there is no set standard Mental Health (MH) screening in Primary
Health Care (PHC). This study identified an innovative, scalable and sustainable solution in a
resource-constrained health system. MH services to be developed as alternatives to institutionalised care. With motivation of available staffing by promoting and delivering MH with available resources
at the Health care centre.
Introduction
Since 1949, there had been no revision of the Mental Health disorders act. However, Zambia on the 4th of
April 2019 passed the Mental Health Act which is the 6th act of 2019. The MH Act brings a much needed
push to the practice of MH in Zambia as it allows education and promotion of MH services and the much
needed acceptance of MH in Zambian communities. Mental health (MH) has been hidden behind a curtain
of embarrassment and discrimination for too long. The suffering and burden in terms of disability and costs
for individuals, families and communities are overwhelming. You will scarcely hear of someone dying from
a direct result of a mental health disease. But the functional disability caused to an individual with a mental
health disease and the number of years lost due to disability and not being able to perform at full capacity
equates to a great loss to the family, communities and nation at large. Currently in Zambia, there is no set
standard MH screening in PHC. With the campaign and adoption of Universal Health Coverage (UHC)
and health for all, the branch of Mental health services are lacking.
MH is more than the lack of mental sicknesses. World Health Organization (WHO) defines health as: “A state of complete physical, mental and social well-being and not merely the absence of disease or disability.” According to WHO, Mental, neurological and substance use (MNS) conditions account for 13% of the global burden of disease. Yet between 75-90% of individuals with MNS conditions do not receive the treatment they require although effective treatment exists. This represents the mental health treatment gap [4] MH should be a concern for all of Zambia, rather than only for those who suffer from a mental disorder. In the last few years, many communities in Zambia have become more aware of this burden.
Chainama Hills College Hospital is Zambia’s national tertiary psychiatric referral institution with a bed capacity of 210. The institution is operational since 1962. Many Zambians think that Chainama is a hospital for the “crazy” people. A very thoughtful shame. However the Ministry of Health through Chainama Hospital provides mental health treatments, occupational therapy, psycho-social counselling therapy, recreation therapy, psychology services and offers various baseline laboratory investigations.
MH affects society as a whole, and not just a small, isolated section. No group is safe from mental disorders, but the risk is higher among the poor, homeless, the unemployed, persons with low education, victims of physical and verbal abuse, children and adolescents, and the neglected elderly. And this has been the trend at Chainama where majority of the clients that seek help come from low-socioeconomic backgrounds. Of note however is that individuals from high socio-economic backgrounds are not safe from mental health illnesses. At Chainama a high percentage of low mood also known as clinical depression, and substance abuse which are illicit drugs and alcohol, is recorded among the above average in society.
The leading causes of mental health admissions for all ages at Chainama over the past years from 2017 - 2019 has yielded a common trend of conditions [5]. Substance use disorders, especially alcohol use mental disorder remains the number one leading cause of admission at an average of 38.5% of total admissions. Other substances include cannabis, cocaine and heroin at 12.4%. This remains a public health concern and Chainama has recently noticed an increased trend of admissions in the younger generation. The Ministry of Health has continued to intensify its efforts to educate Zambians on the negative challenges via community psychiatric services and radio programmes.
Other leading causes of admissions include Brief Psychotic disorder due to acute stressor at 16.2%, Mood disorders which is a spectrum of hyperactivity and low mood at 14.3%, Seizure disorder known as epilepsy with psychosis at 12.2%, Schizophrenia at 11.1%, and general medical diseases with psychiatric features such as HIV-AIDS, syphilis etc.
The leading causes of referrals at Clinic 6, UTH also remains almost along the same lines as those for inpatient treatment [6].
Community psychiatry is the branch of psychiatry concerned with the detection, prevention, early treatment and rehabilitation of mental disorders as they develop within a community with an aim to achieve full social integration. The need to incorporate MH services in communities is needed as evidenced by the patient loads seen at Kanyama first level hospital. There are a number of models of community psychiatry that are used to organize services and manage cases within the community. The model used was the balanced care model.
EIGHT good reasons for integrating mental health into non-specialized health care
1. The Treatment gap and burden of mental disorders is great.
2. Mental and physical health problems are interwoven.
3. Enhance access to MH care.
4. MH closer to homes
5. It is affordable and cost-effective.
6. Generates good health outcomes.
7. To decentralise Chainama Hospital (Main tertiary hospital offering mental health services in Zambia)
8. Promote respect of human rights.
The MH gap in Zambia remains high not just due to lack of Mental Health services but also due to lack of MH specialists. As of July 2019, Zambia has an estimated population of 17 million with only 7 consultant psychiatrists registered with the Health Professional council of Zambia. However, there are many registered Mental Health nurses and clinical officer psychiatry stationed in practice.
This study identified an innovative solution by using the WHO Mental Health Gap (mhGAP) intervention tool in a resource-constrained health system. MH services to be developed as alternatives to institutionalised care. With motivation of available staffing that promotes and delivers MH with available resources. The mhGAP is a WHO programme, launched in 2008, to scale up care for MNS disorders. The programme asserts that, with proper care, psychosocial assistance and medication, tens of millions of people could be treated for depression, psychoses and epilepsy, prevented from suicide and begins to lead normal lives – even where resources are scarce. Its focus is to increase non-specialist care, including non-specialized health care, to address the unmet needs of people with priority MNS conditions.
Objectives
- To assist mental health care providers at Kanyama 1st Level Hospital to review and plan mental health
services effectively for their local population.
- To promote and provide an efficient, predictable format for assessment, treatment and monitoring using
the World Health Organisation Mental Health Gap Intervention tool.
Methods
A descriptive intervention study over a 12-week period (72 hour contact period). Out-patient review clinic
was carried out by a psychiatry registrar in Kanyama.
A mental health unit comprising of: - 2 Mental Health nurses, - 1 Clinical officer psychiatry, and - 2 counsellors (Psychology) was identified and trained using the WHO mhGAP-IG.
Kanyama First level Hospital in Lusaka, Zambia. Borders with Chobolya which is known to be a hub of
illegal drugs and alcohol in Lusaka, Zambia.
Psychiatrist registrar delivered a trainer of trainee using the WHO mhGAP-IG which was taught to the
core mental health unit. Delivered as a Trainer of trainee model to enable the core staff to guide others on
site in the absence of the psychiatrist registrar. The Intervention delivered was using the WHO mhGAP-IG
training of health-care provider (ToHP)
•ToHP teaches 12 core competencies relevant to assessing, managing and following-up people with MNS conditions.
•Training was interactive and enabled participants to practise using the mhGAP-IG in the safety of the training room through:
- Role plays and case presentations of Clients
- group discussions
- familiarization with the mhGAP-IG.
- Out patient clinics with MH team.
- On site clinical teaching and guidance.
- Grand ward round set up.
See one ------→Do one ------→ Teach One
i- Identified and diagnosed patient using WHO Mental Health Gap, observation- question and answer.
ii- Allowed to asses’ patients under supervision.
iii- Teach/Impart skill to fellow Staff Training concluded with a Trainer of Trainers workshop/Lecture.
In Out Patient Clinics the following academic and clinical skills inferred to MH staff. Allocation of referrals.
Managing waiting lists & caseloads Patient reviews
- Investigations & prescriptions
- Monitoring of medication & side effects
- Counselling & therapy services
Results
- Financial saving, (cost effectiveness)
- Community centred care, (Belonging)
- Integration in PHC, (Efficient)
- Reduced level of referrals.
- Outpatient treatments, promote dinstutionalisation.
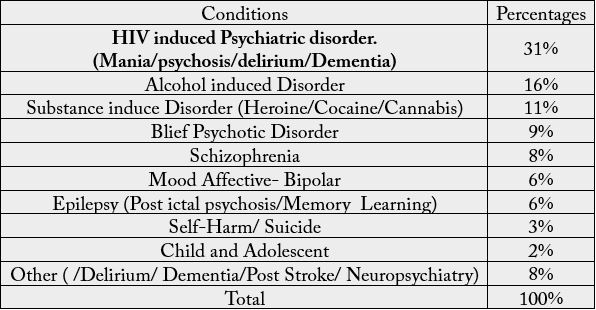
A total of 358 patients were reviewed in clinic as out-patients, highest percentage of patients reviewed were HIV induced psychiatric disorders (31%) followed by Alcohol induced disorder at 16%.
i- Primary prevention
ii- Secondary prevention
iii- Tertiary prevention
Advocacy - awareness and anecdotal experiences of staff from Kanyama 1st level Hospital. Staff where
mentored to deliver MH discussions on National Media such as Zambia National; Broadcasting Corporation
programme titled, Doctor on Air - National Radio stations
- Early detection, diagnosis and treatment of disease.
- Allocation of referrals
- Managing waiting lists and caseloads
- Patient reviews (New/Routine/Discharge)
- Biopsychosocial approach of treatment
- Occupational counselling and family counselling
At Hospital:
- Referrals:
i- Reduced number of referrals by 65% to Chainama Hospital
ii- Improved quality of referrals.,ii- Improved quality of referrals.,
- Point of care support,
- Community: fight stigma and improved awareness
- Decongest tertiary mental health hospitals, Chainama/UTH
- Outpatient treatment for relapses and
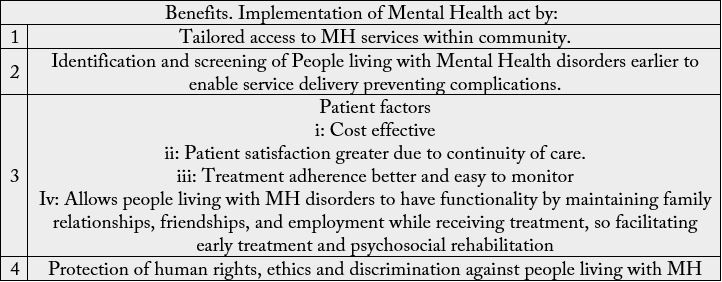
- Implement the 6th Act of parliament, Mental Health Act.
Discussion
Mental health is crucial to the overall well-being of individuals and communities in Zambia. Unfortunately,
in most parts of the country, mental health and mental disorders are not given anywhere the same importance
as physical health due to the embarrassment faced by individuals and their families. Rather, mental health
has been unnoticed or ignored due to lack of awareness or cultural ideations. In the past few years it has
become evident that Chainama hospital is not an institution for the “crazies” but a hospital where the mind
and all its disabilities are identified and where possible treated. One of the leading referral communities
from where Chainama hospital receives their patients is from Kanyama township.
Kanyama First level hospital has an overall staffing of 347 members and caters to a population of 273,000 in Kanyama township. It has 5 departments and has 6 satellite clinics that send referrals to it. Prior to the intervention, Kanyama Hospital used to send Mental Health patients to the tertiary hospitals such as University Teaching Hospital- clinic 6 or Chainama which are located over 30km away. A one day 5-hour clinic in the duration of 12 weeks yielded an increase of mental health patients seeking services at Kanyama First level hospital. Shift of patients from tertiary mental health hospitals such as University Teaching Hospital Clinic 6 and Chainama Hospital was recorded which proved the need for services closer to individual’s homes. The pre and post assessment of Core MH Team coupled with the number of case reviews audited provides insight on the need for strengthening MH- PHC care. The patient cases and percentages showed a similar number and pattern of cases. HIV induced psychiatric disorders and Substance use disorder being the most common presentations.
The Mental Health Gap Intervention Guide, (mhGAP-IG) is a technical tool for non-specialized healthcare providers to assess, manage and follow-up people with MNS conditions. However, looking at the content of the tool, it is detailed enough to be used by health staff in PHC to offer basic assessment and treatment of mental health. The mhGAP-IG training of health-care providers can be tailored to integrate mental health care into non-specialized health settings. This training has allowed an introduction of a MH unit at Kanyama First Level Hospital and built the skills and confidence required to use the mhGAP-IG in clinical workplaces.
Tailoring the mhGAP-IG with available resources can aid in setting up, plan and administer mental health care in community setting and demonstrate improvement in the quality of mental health care to the users of community based service.
Community psychiatry is the branch of psychiatry concerned with the detection, prevention, early treatment and rehabilitation of mental disorders as they develop within a community with an aim to achieve full social integration. The need to incorporate MH services in communities is needed as evidenced by the patient loads seen at Kanyama first level hospital. There are a number of models of community psychiatry that are used to organize services and manage cases within the community. The model used was the balanced care model.
The ideal treatment of MH services in Zambia is still far however with the use of available resources in the health system couple with personnel, the balanced care model can be applied in PHC. There may be no strong evidence that a comprehensive system of mental healthcare can be provided by hospital-based care, but nor is there strong evidence that it can be provided by community-based services. Rather, a balance is necessary which includes both hospital and community components [7].
This study has helped innovate and integrate MH services in PHC and has the potential for a scale up with adequate resources and funding to all basic health care centres to strengthen MH Care in Zambia.
The study has demonstrated skill and understanding in formulating, developing and implementing a quality of care improvement project. It offers an alternative to the existing systems in place and cushions the MH burden currently faced by the tertiary MH Hospitals in Zambia.
Recommendations
1- Use of WHO mental health gap intervention tool to carry out trainer of trainee to impart up to date skills
among mental health staff to improve MH service delivery in PHC screening.
2- Introduce community MH centres at each general hospital, a move of MH services from specialist
mental hospitals to general hospital sites.
3- Use of Smartphone for consultation liaison for reviews and emergencies in MH delivery, scale up to
telemedicine.
Proposed scale up by authors
- Open line of consultation liaison via smart phone and tele-medicine
- Communication of referrals prior to sending to tertiary hospitals
- Provide similar training to local clinics that refer to Kanyama 1st level hospital.
- Source for grants to support medication supplies
- Continued site visits by psychiatrist registrar
- Continued motivation to core staff team by Continued Medical Education. (Invite to Chainama hospital
for clinical presentations and placements)
- Introduce shadowing of staff to tertiary hospitals such as Chainama Hospital or University Teaching
Hospitals.
Limitations
Challenges: Taking into consideration of integration and lack of financial availability:
- Medication: lack of Psychotropic drugs for diagnosed patients at PHC level
- Staff: Limited staff working in all departments at PHC.
- Social welfare: lack of social services at PHC level [8-10].
Conclusion
In keeping with the above observations, the optimal method of delivery of mental health care to the patient
is not through tertiary-care mental hospitals alone, as is the case currently but through the Primary Health
care system supported by tertiary level health care. Thus having a potential to reach out to remote and rural
areas. A tailored approach use of the World Health Organisation Mental Health Gap intervention tool is a
good source to incorporate into PHC service delivery of Mental Health to strengthen links and bridge the
MH Gap.
Acknowledgments
Dr Sanjase, Dr S. Nyangu, Mr Mills, Sister Grace, Kanyama First Level Hospital.
Dr. S. Chanda, Dr. M Mataa, University Teaching Hospitals.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!