Biography
Interests
Salem Bouomrani1,2*, Mouna Dey3, Nesrine Rgaïeg1,2, Houda Ghorbel4 & Mayada Ben Hamad1,2
1Department of Internal Medicine, Military Hospital of Gabes, Gabes 6000, Tunisia
2Sfax Faculty of Medicine, University of Sfax, Sfax 3029, Tunisia
3Department of Nephrology, Gabes Regional Hospital, Gabes 6000, Tunisia
4Department of Infectious Diseases, Gabes Regional Hospital, Gabes 6000, Tunisia
*Correspondence to: Dr. Salem Bouomrani, Department of Internal Medicine, Military Hospital of Gabes, Gabes 6000, Tunisia.
Copyright © 2018 Dr. Salem Bouomrani, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Systemic lupus erythematosus (SLE) is an autoimmune disease that classically affects young
women. The onset of the disease after the age of 65 (a very late-onset lupus) remains exceptional and
unusual. We are reporting an original observation of aseptic lymphocytic meningitis inaugurating
a very late-onset lupus in a man.
A 73-year-old man, with no pathological medical history, was hospitalized in the department of infectious diseases for aseptic lymphocytic meningitis occurring after a simple flu syndrome. Initial
explorations were negative and he was treated as herpetic meningoencephalitis. After four months,
he presented edema of lower limbs with 24h proteinuria at 2g, aseptic leukocyturia at 30,000/ml
and hematuria at 1,000/ml. Subsequent investigations supported the diagnosis of SLE with extra
membranous lupus nephritis and central meningeal and parenchymal neurolupus.
The patient was treated with three boli of methylprednisolone followed by prednisone and hydroxychloroquine with a favorable evolution: negativation of proteinuria, normalization of lumbar puncture, leukocyte count, and urinary sediment at one month of treatment.
As exceptional as they may be, very late-onset forms of SLE must be known by hospital practitioners
to avoid diagnostic delays and improve the prognosis of this potentially fatal disease. Our observation
is distinguished by the male sex, the very late-onset of the disease, and by the revealing clinical
presentation. To our knowledge this is the first case of very-late onset lupus revealed by aseptic
lymphocytic meningitis.
Introduction
Systemic lupus erythematosus (SLE) is an autoimmune disease that affects young women of childbearing
age with a sex ratio of 9 women for one man. It is a systemic disease with multi-visceral and multi organ
involvement, the most severe of which are renal (lupus nephritis), neurological (neurolupus) and cardiovascular
(angiolupus) dominating the prognosis [1].
The disease can, however, occur at any age, and late forms of the disease are arbitrarily defined by onset after the age of 50 [2,3]. These forms represent approximately 3-20% of cases according to series [2,4,5]. The onset of the disease after the age of 65 (a very late-onset lupus) remains exceptional and unusual [6-8]. The frequency of these very late forms is estimated at 5% [7-9]. They are therefore very little known and little studied, representing a real diagnostic challenge for the clinician [6-8]. Indeed, only four studies have focused on very late-onset lupus occurring after the age of 65 [6-9].
In these forms, the specific neurological manifestations of the disease, and in particular aseptic lymphocytic meningitis, are exceptional and unusual.
We are reporting an original observation of aseptic lymphocytic meningitis inaugurating a very late-onset lupus in a man.
Case Report
A 73-year-old man, with no pathological medical history, was hospitalized in the department of infectious
diseases on the 19-09-2016 for acute and invalid headaches with arhtromyalgia and fever occurring after a
simple flu syndrome.
Initial examination noted fever at 39°C, regular tachycardia at 100/min, palpation-induced myalgia, and mental confusion. The biological assessment done in the emergency department eliminated an acute metabolic cause of this confusion: glycemia at 7.8mmol/l, creatinine at 80mmol/l, urea at 3.8mmol/l, calcemia at 2.52mmol/l, natremia at 138mmol/l, serum potassium at 4.15mmol/l, hemoglobin 13.8g/dl, leukocytes 11,100/mm3, platelets 159,000/mm3, aspartate aminotransferase at 32UI/l, alanine aminotransferase at 28UI/l, prothrombin time at 100%, and arterial blood gas without abnormalities. On the other hand, a marked biological inflammatory syndrome was noted with an erythrocyte sedimentation rate at 102mmH1 and a C-reactive protein at 46mg/l.
Cerebral computed tomography did not object infarction, tumor, intracranial hypertension or cerebral thrombophlebitis.
The ophthalmological examination with fundus was without abnormalities. The lumbar puncture returned a clear, normotensive, citrus-yellow cerebrospinal fluid, and the cytological and biochemical analysis confirmed the diagnosis of lymphocytic meningitis: leucocytes at 151 elements/mm3, of which 70% were lymphocytes and 30% were neutrophils, red blood cells at 4 elements/mm3, albuminorrachie at 0.42g/l, glucorrachia at 3.52mmol/l for a concomitant blood glucose concentration of 6.34mmol/l. Direct bacteriological, viral, fungal, and culture examinations were negative.
The cultures in the blood and the urine were negative. The search for tuberculosis was also negative, as were the serodiagnostics of human immunodeficiency virus, brucellosis, leptospirosis, and typhoid fever.
The West Nile virus serologies favored an old infection: IgG +/IgM- in the blood and IgM- in the cerebrospinal fluid.
No recent traumatic brain injury or suspected drug or toxic use was noted. The electrocardiogram, the chest X-ray, and the echocardiogram were without abnormalities.
The patient was treated with intravenous Aciclovir (zovirax®) 750mg eight times a day in the aftermath of herpetic meningoencephalitis.
The evolution was favorable with apyrexia on the fourth day and gradual disappearance of headache and arthromyalgia.
During his regular monitoring at the outpatient clinic, on 19-01-2017, was noted the appearance of painless and keeping the bucket edema of lower limbs. The patient was referred to the cardiologist and the nephrologist for advice and adapted explorations. The cardiological examination, the electrocardiogram, and the echocardiogram were without abnormalities. The 24h proteinuria was at 2g. Examination of the urinary sediment showed aseptic leukocyturia at 30,000/ml and hematuria at 1,000/ml. Creatinine was at 90mmol/l, plasma electrophoresis, and immunoelectrophoresis were without abnormalities. Thus a renal biopsy puncture was performed objectifying an extra membranous glomerulonephritis. The patient was referred to us for aetiological assessment of this glomerulonephritis.
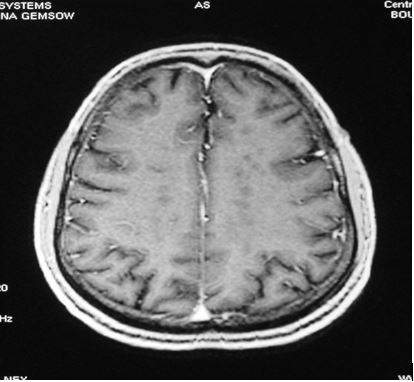
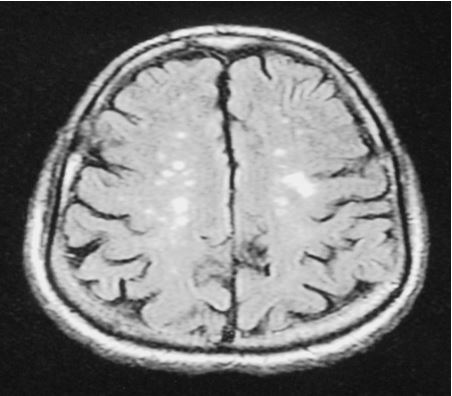
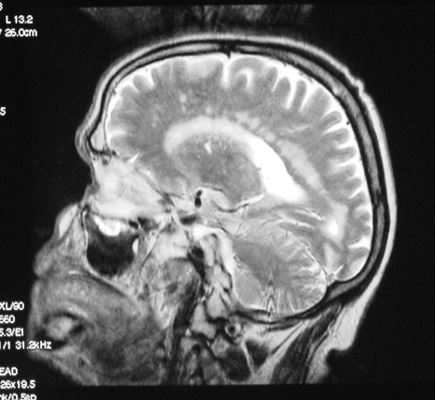
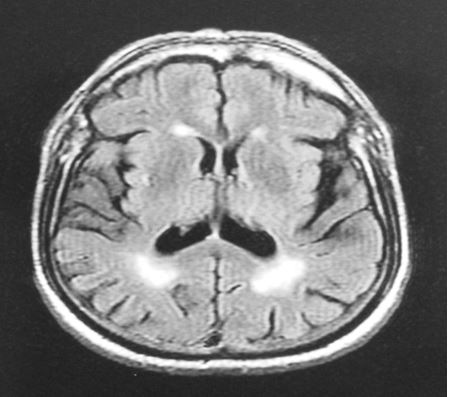
Subsequent investigations supported the diagnosis of SLE with positive native anti-DNA antibodies, positive anti-nuclear antibodies at 1/640 with speckled immunofluorescence, positive anti-nucleosome antibodies, lymphopenia at 1,240/mm3, and aseptic lymphocytic meningitis. Cerebral magnetic resonance imaging showed moderate cortical and sub-cortical atrophy, multiple periventricular and sub-cortical white matter lesions with T1 hyposignals, T2 and FLAIR hypersignals, particularly in semi-oval centers and posterior junctional zones (Fig 1 & 2), as well as multiple punctiform sup tentorial and occipital periventricular confluent plaques with T2 hypersignal, T1 hyposignal, and enhancing homogeneously after gadolinium injection (Fig 3 & 4).
Thus the diagnosis of SLE with lupus nephritis and neurolupus was retained.
The patient was treated with three boli of methylprednisolone (1g/day for three days), followed by prednisone (1mg/kg/day for one month and then gradual decrease) and hydroxychloroquine (400mg/day) with a favorable evolution: negativation of proteinuria, normalization of lumbar puncture, leukocyte count, and urinary sediment at one month of treatment. MRI brain monitoring is scheduled six months from the beginning of corticosteroid therapy.
Discussion
Very late-onset forms of SLE are exceptional; indeed the review of the literature finds only 4 studies about
this topic:
- Only 21 patients with very late-onset lupus were found in the Taiwanese series of Pu Sj et al, spread over
11 years [6],
- Only 18 patients with lupus revealed after the age of 65 years were identified in the Zulfiqar AA et al.,
series, over a period of 29 years (1985-2013), and in four French hospitals [7],
- Similarly, only 17 patients were collected over a period of 13 years in the series of Goujard S et al, in four
French university hospitals [8],
- And finally only 30 patients were collected over a period of 15 years in the Italian series of Padovan M et
al [9].
Other observations are reported as sporadic cases.
The diagnosis of these late-onset forms of the disease is often very difficult because of atypical and nonspecific [4,5,7,10,11], insidious [2], and sometimes unusual clinical presentations [12,13], making these forms a real diagnostic challenge for the clinician [2,11].
The main clinical manifestations in these late-onset forms of lupus are mainly: deterioration of general condition, arthritis, cutaneous manifestations, thromboembolic complications, pleurisy, dry syndrome, and psychiatric manifestations [2,7,8]. Neurological manifestations are exceptionally revealing of these forms [7,8].
These late-onset forms are characterized by a less marked female predominance and much longer diagnostic delays compared to the classic forms of SLE in young adults [6,7,9]. Iatrogenic complications are also significantly frequent in these late-onset forms requiring special attention in therapeutic prescriptions [2,6- 8].
Compared to early-onset forms, neurological manifestations are rare in late-onset lupus: 6.6% versus 36.6% in the Tomic-Lucic A et al., series [14]. This has also been verified in the very late-onset SLE series in subjects over 65 years of age [6-9].
Of all the possible neurological manifestations of SLE, acute meningitis remains exceptional [15,16]. They can often be of infectious origin because of the state of immunosuppression caused by the disease itself and the therapeutics used (corticosteroids and immunosuppressive agents); indeed, in the Kim JM et al., series, acute meningitis was noted in 1.4% of lupic patients and was infectious in more than 55% of cases [15].
Aseptic lymphocytic meningitis specific of SLE was found in only 0.63% of cases [15]. This non-infective aseptic meningitis in the elderly pose the problem of their etiological diagnosis, especially that other etiologies are particularly common in these subjects, especially neoplastic meningitis and drug-induced meningitis [16,17]. No case of aseptic meningitis has been found in the series studying the very late-onset forms of lupus [6-9].
Conclusion
As rare as they may be, very late-onset forms of SLE must be known by hospital practitioners to avoid
diagnostic delays and improve the prognosis of this potentially fatal disease.
Our observation is distinguished by the male sex, the very late-onset of the disease, and by the revealing clinical presentation. To our knowledge this is the first case of very-late onset lupus revealed by aseptic lymphocytic meningitis.
Thus, the diagnosis of SLE must always be evoked in front of any aseptic lymphocytic acute meningitis of the elderly subject that is not proven.
Conflicts of Interest
None
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!