Biography
Interests
Shimon Shatzmiller
Department of Chemical Sciences, Ariel University, Ariel 40700, Israel
*Correspondence to: Dr. Shimon Shatzmiller, Department of Chemical Sciences, Ariel University, Ariel 40700, Israel.
Copyright © 2020 Dr. Shimon Shatzmiller. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
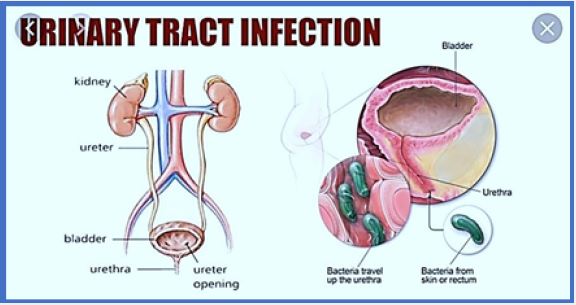
Urinary tract infections (UTis) are caused by bacteria that increase the body's defenses in the urinary tract. They can affect the bladder, kidneys, and the ducts that run between them [1].
Urinary tract infection, like any other infection, refers to the invasion and multiplication of one or more pathogens that are not usually found in your urinary tract. The urinary tract is composed of the urethra, bladder, urethra and kidneys, and infection can be in one or more of these (see our chart below).
When urinary tract infections continue to recur:
Unless you are in the unlucky minority of the person who has never had urinary tract infection (UTI), you are well acquainted with the symptoms. You may feel frequent urination to urinate, but move urine slightly as you walk. Your urine may be cloudy, tingling with blood and stinky. For 25% to 30% of patients with urinary tract.
Infection, the infection recurs within six months. Image: Thinkstock If you have repeated UTls coming back, you have experienced the toll they charge for your life. However, you may take a little comfort knowing they may not be the result of anything you did. "UTls are returningaren't due to poor hygiene or something else that women have brought on themselves.
Urinary tract infections (UTis) are a severe public health problem and are caused by a variety of pathogens, but most often by Escherichia coli, Klebsiella pneumonia, Proteus mirabilis, Enterococcusfaecalis and Staphylococcus saprophyticus. High recurrence rates and increased antimicrobial resistance among osteopaths threaten to considerably worsen the economic load of this disease. In this review, we discuss how basic scientific studies elucidate the molecular details of the confluence that occurs in the host-pathogen interface, as well as the implications of these interactions on the pathophysiology of UTis. We also describe current efforts to translate this knowledge into new clinical therapies for UTis [2].
Urinary tract infections (UTls) are some of the most common bacterial infections, affecting 150 million people every year worldwide [3]. In 2007, in the United States alone, there were
Estimate office visits of $ 10.5 million for UTI symptoms (accounting for 0.9% of all ambulatory visits) and about 2-3 million emergency department visits 2-4. Currently, the social costs of these infections, including health care costs and time off work, are about US $ 3.5 billion a year in the United States alone. UTIS is a major cause of morbidity in infants, older men and females of all ages. Serious sequences include frequent recurrence, sepsis, renal damage in young children, preterm birth, and complications caused by frequent antimicrobial use, such as high-grade antibiotic resistance and Clostridium difficile colitis.
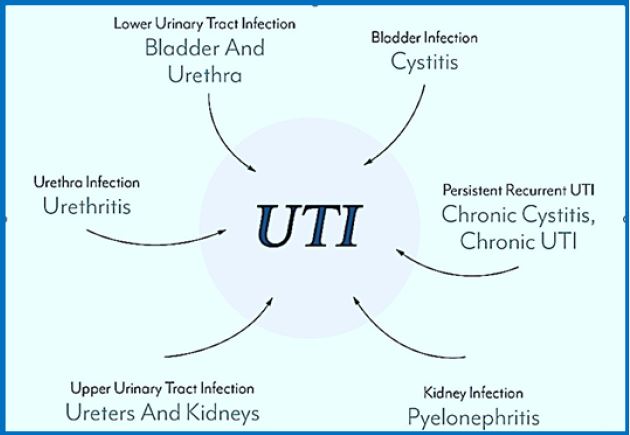
Clinically, UTls are classified as complex or complex. Uncomplicated external devices usually affect people who are otherwise healthy and do not suffer from structural or neurological urinary disorders. These infections are differentiated to lower UTls (cystitis)
And upper pyelonephritis [4-6]. A number of risk factors are associated with cystitis,
Includes female sex, prior UTI, sexual activity, vaginal infection, diabetes, obesity, and genetic susceptibility. Disease, immune suppression, kidney failure, kidney transplant, pregnancy and the presence of foreign bodies such as calculations, residence
Catheters or other drainage devices [7-10]. In the United States, 70-80% of complicated UTIs are
Can be attributed to residential catheters, which are $ 1 million in cases 4. Catheter-related UTIS cells (CAUTis) are associated with increased morbidity and mortality and together they are the most common cause of secondary bloodstream infections. S. factors.
The gut microbiome, as a pathogenic target for the dollar.
Understanding the urinary microbiome [11,12].
While previous studies have investigated the role of the gut microbiome in US dollar pathology, the role of the urinary microbiome cannot be focused on. "This is the first, to the best of our knowledge, metanomic research that really compares the urinary microbiome between healthy populations and dollar patients," says Aaron Miller. , Ph.D., Project Scientist, Lerner Research Institute and Urological and Glycology Institute, and Senior Research Fellow.
The researchers analyzed the microbiota from the gastrointestinal and urinary tract of 67 individuals (43 people with no history of the US dollar and 24 patients with active USD), and performed a metabolic analysis of urinary metabolism (all small molecular chemicals produced by cell metabolism).
Their analysis found that the urinary microbiota changed based on antibiotic use, family history of dollars, and sex - factors related to USD but not related to urinary microbiome. Among the health and dollar groups, urinary microbiota were significantly different, whereas their gut microbiota showed only slight variability.
"The urinary microbiome associated with the disease is much stronger than the stomach microbiome. "People sometimes assume that the gut microbiota is where all the action takes place. Although, here, the greatest density and diversity of bacteria is found, in this case, the urinary microbiome plays more of a role."
In addition, there is an intuitive relationship between the urinary microbiome and the progression of the dollar, because urinary tract is a stone. Although not surprising given the proximity, there is a common misconception that the urinary tract is sterile, even though it contains a natural bacterial community [13- 15]. Recent studies in the application of molecular techniques have shown the presence of urine Microbiota has not been identified by standard microbiological techniques. These have been found in the urine of healthy people and with clinical symptoms. The present findings of these studies to date and describes The molecular techniques, and specifically, any difference in microbiome with respect to urogyncological disease. Furthermore, the role of commune bacteria in the lower urine Path is considered
Contaminants are complex aggregates of crystals that are poured into an organic matrix Closely associated with urinary tract infections. Christian Patient Management Pollution is challenging because of the complexity of calculations and high recurrence rates. The formation of contaminants is a multifactorial process that can be driven by urine chemistry, Urinary microenvironment, presence of urinary modulatory agents, associations with Bacteria, and biofilm development. Despite decades of investigation, the mechanisms of The formation of contamination stone is still well understood. Understanding of the formation and growth of pollution stones - including the role of organics in the stone matrix, Microorganisms, and biofilms in stone formation and their influence on the properties of stone - and The medical implications of these insights may be crucial to the development of improvement Treatments. Tools and approaches used in various fields (e.g., engineering, chemistry, Mineralogy and microbiology can be applied to understand better the microorganism - a mineral Interactions leading to stones formation in pollution. Therefore, the use of a variety of Essential multidisciplinary approaches to improve diagnosis, prevention and treatment of infection stones.
What Causes A Urinary Tract Infection?
We should address them as with any other type of infection - by performing appropriate tests to find the
reason for their further occurrence, and consequently make a logical conclusion: effective treatment
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!