Biography
Interests
Fakhsheena Anjum1*, Sana Ahmed1, Saqiba Rasool1, Juweria Khan1 & Samina Faiza2
1Dow College of Pharmacy, Dow University of Health Sciences, Karachi, Pakistan
2Faculty of Pharmacy, University of Karachi, Karachi, Pakistan
*Correspondence to: Dr. Fakhsheena Anjum, Dow College of Pharmacy, Dow University of Health Sciences, Karachi, Pakistan.
Copyright © 2019 Dr.Fakhsheena Anjum, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
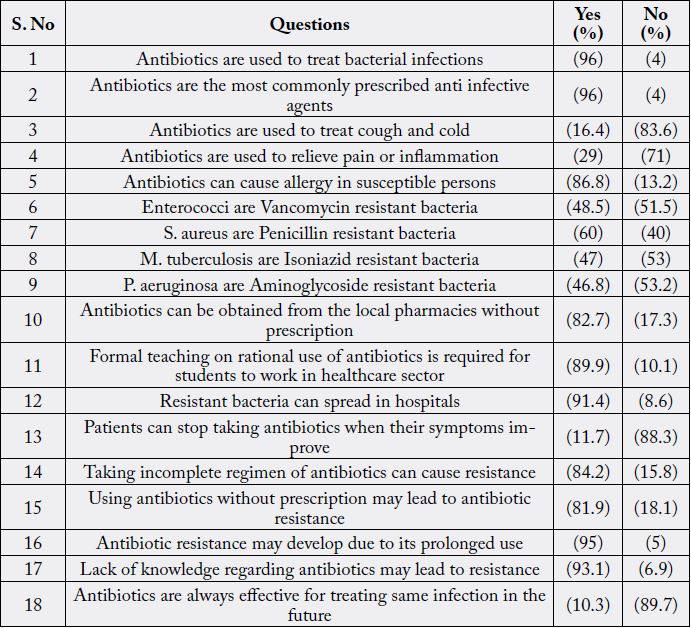
To assess knowledge about antibiotics and their resistance among Pharmacy under graduate students, this study was undertaken from July to November 2015 in three public sector universities located in Karachi, Pakistan, offering Pharm-D program. Completed questionnaires were collected by the researchers for descriptive analysis using SPSS version 16.0. Out of n= 150, n= 132 completely filled questionnaires were collected from the students (response rate= 88%) of final year Pharm. D. Around 96% results showed that the students knew that antibiotics are used for bacterial infections and they are considered as most commonly prescribed anti-infective agents by prescribers. More than 80% students knew that antibiotics should not be used for cold, cough, inflammation or pain and about 85% students thought that allergy may be developed due to antibiotic use in susceptible persons. Around 50% students had no idea that enterococci are Vancomycin resistant bacteria; about 60% replied that S.aureus are Pencillin resistant bacteria; almost 60% denied that M. tuberculosis are Isoniazid resistant bacteria whereas around 50% students had no idea that P. aeruginosa are Aminoglycoside resistant bacteria. Almost 80% students agreed that antibiotics could be obtained without prescription from local pharmacies of the city. It was seen that almost 85% students knew that incomplete antibiotic regimen may cause resistance and about 95% had knowledge that antibiotic resistance may also be developed due to prolonged use. About 90% students thought that formal teaching on rational use of antibiotics is required to reduce burden of antibiotic resistance. The knowledge about antibiotics and their resistance was found quite satisfactory among under graduate Pharm-D students but still improvement is required specially for those students who would be practicing in the health care sector in future.
Introduction
There has been an increase in the prevalence of antimicrobial resistance due to non judicious use of antibiotics
[1,2]. Antimicrobial resistance is a crucial public health catastrophe [3-6]. More than 80% of Chinese
outpatients were reported in a systematic review to be prescribed with antibiotics, who were suffering from
upper respiratory infections [7]. Antibiotic self-medication by patients contributes to its misuse, and this is
due to easy access from pharmacies in particular, in several developing states [8]. Antibiotic misuse may also
surge due to knowledge and behaviours of doctors and also the pressure from patients [9]. Several studies
have described medical students’ Antibiotic related behaviours of medical students have been reported by
many studies conducted in Pakistan [10], Nepal [8], the USA [11] and Europe [12-14].
The crisis of antibiotic resistance crisis is crucial in developing countries and this is because of various factors like irrational practice of antibiotics, availability of antibiotics without prescription, etc., [15]. It had been observed that more than 50% of antibiotics were sold or bought without prescription [16]. Proper understanding of resistance patterns to develop antibiotic guidelines and rational practices is necessary. Taking this into consideration, there are several studies that highlighted revision of junior healthcare professionals curriculum for promoting rational use of antibiotics [17]. Moreover, WHO has also highlighted importance of undergraduate training in judicious prescribing practice [18]. Pharmacists help in the optimal and rational use of drugs. The education, training, and skills of pharmacy students also influence the patterns of antibiotic use in various settings [19].
The world is moving towards a ‘post-antibiotic era” as per World Health Organization (WHO). According to WHO global action plan, improvement in cognizance and understanding of antibiotics and their resistance to control further expansion of antibiotic resistance by means of education, training and effective communication, is essential [20]. Pharmacists are significant part of healthcare team. They are key persons to advice for proper medicine use [21,22]. In fact, competent and trained pharmacists have the potential to impact behaviour of other health professionals and patients [23,24] thereby ensure rational use of drugs [25]. Insufficient education and inadequate training of pharmacist in some countries may lead to inefficient practices [26,27] that may give way to pharmacists for irrational use and supply of antibiotics [28] and also sales of antibiotics without prescription, in community pharmacies [29].
Methods
This study was conducted from July to November 2015 in three public sector universities of Karachi, Pakistan
offering Pharm. D. program. The questionnaire was adapted and modified from previously done researches
and was focused on the knowledge of students regarding antibiotics and resistance. The completely filled
questionnaires were collected by the researchers and analyzed using SPSS version 16.0.
Results
The response rate of the students for this survey-based study was 88%. From the given table it can be seen
that majority students were well aware about general knowledge regarding antibiotics and resistance.
Discussions
In this study, it was seen that around 96% students knew that antibiotics are used for bacterial infections
and they are considered as most commonly prescribed anti-infective agents by prescribers. It is evident from
recent studies that non judicious and irrational use of antibiotics may lead to their resistance which has
become a grave predicament universally [30]. In this study, almost 85% students responded that incomplete
antibiotic regimen may give rise to resistance and about 95% had the knowledge that antibiotic resistance may also be developed due to prolonged use. In a similar study conducted by Akram Ahmad et al. (2015), the
knowledge of pharmacy students was considered as remarkably high regarding most of the questions about
antibiotics; it was reported that 98.14% participants identified antibiotic resistance as a serious public health
issue [31]. The results of other studies are also in line with the results of this study, suggesting satisfactory
knowledge of pharmacy students regarding antibiotic use and resistance [32,33].
Regarding knowledge about micro organisms versus antibiotics, around 50% students recruited for this study had no idea that enterococci are Vancomycin resistant bacteria; about 60% replied that S.aureus are Pencillin resistant bacteria; almost 60% denied that M. tuberculosis are Isoniazid resistant bacteria whereas around 50% students had no idea that P. aeruginosa are Aminoglycoside resistant bacteria. One Chinese study (2014) revealed that the undergraduate pupils had insufficient knowledge and unsuitable practices regarding antibiotics, with a high rate of self-medication [34]. In another study (2015), it was observed that pharmacy students had many unused antibiotics either due to non compliance or unsuitable antibiotic use signifying antibiotic resistance development [35]. Therefore, to control antibiotic resistance, it is crucial to change the behavior of providers and consumers [36].
It was established in a research by Akram Ahmad et al. (2015) that only 62.03% participants responded that bacteria are not responsible for common cold and flu [31] but in our study, more than 80% students knew that antibiotics should not be used for cold, cough, inflammation or pain and about 85% students thought that allergy may be developed due to antibiotic use in susceptible persons. Similarly, in another study (2014), 95% students correctly responded that antibiotics should not be used in common cold and flu [32]. A recent research by M. H. F. Sakeena et al. (2018) showed that more than half of the junior pharmacy students incorrectly replied that antibiotic use is suitable to manage cold and flu [19].
Almost 80% students in this study agreed that antibiotics could be obtained without prescription from local pharmacies of the city. Easy access to antibiotics from pharmacies in several developing countries was reported in a study conducted in Nepal (2016) which was considered as contributor to self medication of antibiotics by patients [8]. In another study done in Kosovo in 2016, half of the students admitted that they self-medicated antibiotics but majority specified that they will not give antibiotics without prescription [13].
In our study, around 90% students thought that formal teaching on rational use of antibiotics is required to reduce burden of antibiotic resistance. Scaioli et al. (2015) also found out that further awareness and training on antibiotic consumption and resistance was required during the degree courses in the core curriculum of European School of Medicine [12]. Also, several researchers (2004) highlighted about inadequate training of healthcare professionals in their undergraduate program regarding antibiotic use and resistance [37]. Many other researches have emphasized that substantial effect on professionals’ attitudes and behaviour about antibiotic use can be seen after educating undergraduates about antibiotics and their appropriate use. This is in particular for students of professional health care degrees i.e. pharmacy, medicine and nursing [38,39].
Conclusion
A good understanding regarding antibiotic and its resistance was shown from the students in this study.
There is a room for improvement in the existing curriculum of Pharm.D. which is being taught in various universities in Karachi. Educational trainings can certainly contribute towards judicious use of antibiotics
and prohibition of antibiotic dispensing without prescription.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!