Biography
Interests
Chukwurah Ejike Felix1, Obeagu Emmanuel Ifeanyi2* & Nome Esther ogechi3
1Department of Haematology and Immunology, Faculty of Clinical Medicine, Ebonyi State University, Abakaliki,
Nigeria
2Department of Medical Laboratory Science, Faculty of Health Sciences, Imo State University, Owerri, Nigeria
3Department of Medical Laboratory Science, Faculty of Health Sciences, Ebonyi State University, Abakaliki, Nigeria
*Correspondence to: Obeagu Emmanuel Ifeanyi, Department of Medical Laboratory Science, Faculty of Health Sciences, Imo State University, Owerri, Nigeria.
Copyright © 2019 Obeagu Emmanuel Ifeanyi, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Prevalence of some blood borne viral infection such as human immunodeficiency virus (HIV), hepatitis B virus (HBV), and Hepatitis C virus (HCV) among road accident victims in Federal Teaching Hospital Abakaliki was estimated. This is to assess the rate at which these viral infections occur and to emphasize on the need for strategies to minimize the risk of transmission to health workers. One hundred and ten (110) subjects of both sexes (77 males and 33 females) of different age groups were included in this study. Blood samples were obtained through vene puncture into a plain tube, allowed to clot and the sample centrifuged to obtain the serum. The serum was applied to the sample pad of the strips used for HIV, HBV, and HCV using immunochromatographic method for antibody detection. The test strips were placed horizontally on non-absorbent surface and allowed for about 10 to 20 minutes. The result showed that 3 subjects were HIV positive with prevalence of 2.72%, and 9 subjects were HBV positive with prevalence of 8.18% while 6 subjects were HCV positive with prevalence of 5.45%. Total numbers of males positive were 13 while 5 females were positive. A total of 18 (16.36%) were positive while 92 (83.64%) were negative. There was also a case of co-infections in a subject with HBV and HCV. The result of this study thus indicate that HBV was more prevalent, followed by HCV and HIV. This suggests that health workers should be vaccinated against HBV and also observes the standard precautions in handling patients so as to prevent or reduce the risk of transmission of these blood borne viral infections.
Introduction
Blood borne viral infections are those viruses that can be spread through contamination by blood or other
body fluids. The most common examples of blood borne viral infections are human immunodeficiency virus
(HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV) [1]. Blood-borne infection such as HIV,
HBV, and HIV infection vary in prevalence between countries in both the developed and developing world.
The risk of parenteral transmission of each of these viruses also varies, with HBV being ten times more likely
to be transmitted than HCV, and HIV much less likely to be transmitted than either of these. Blood borne
viruses are most commonly spread within the healthcare environment by needle stick or sharps injuries
during medical procedures, or through mucocutaneous exposure. With estimates of the number of health
care workers worldwide varying between 35 and 100 million, the potential number of people at risk is
extremely high. Fortunately, numbers of actual infections attributed to occupational exposure are relatively
low with 65,000 HBV infections, 16,400 HCV and 1000 HIV infections in 2000. However, most if not all
of these infections could have been prevented, usually by the health professionals [2,3].
In 1999, newly infected persons with HIV, the causative agent of acquired immune deficiency syndrome (AIDS) was 5.4 million worldwide; an estimated rate of eleven (II) persons per minute or 15,000 new infections per day. Hepatitis B caused by hepatitis B virus is the leading cause of chronic liver disease and liver cancer, the third most common cause of death in countries with high HBV endemicity [4]. HTV and HBV co-infections have been reported and co-infected individuals are 17 times more likely to die than those with hepatitis B alone [5]. Reports have shown that HBV protein accelerates on-going HIV-1 replication (Gomez et al., 2001), while HIV decreases the rate of HBV clearance in acute infection and enhances the progression ul liver disease in those with chronic hepatitis B [6]. Hepatitis C is a blood borne pathogen that poses a significant threat to public health worldwide [7]. Globally an estimated 170 million people or three percent (3%) of the world’s population may be infected with hepatitis C. Data on estimated prevalence of hepatitis C in Nigeria showed 2.1 percent in the general population [8].
The problem of viral hepatitis and HIV in hospital populations around the world has been studied especially because of the fact that hospitalized patients represent a possible source of infection to health care workers. Health workers are at risk for blood borne infections like HIV and viral hepatitis and can also act as focal point in their onward transmission. Vaccination is one of the best methods of protection against blood borne infections. However, vaccinations are currently available only for hepatitis B virus [9]. Occupational exposure to blood borne pathogens can result from needle stick injury, mucocutaneous contact or blood contact with non-intact skin [10]. This exposure can lead to infections with HBV, HIV, HCV and other blood borne pathogens like cytomegalovirus (CMV), herpes simplex virus and parvo virus. The risk of transmission of hepatitis B infection by needle stick injury is up to 30 percent for susceptible health care workers without post exposure prophylaxis or sufficient hepatitis B vaccination [11]. The risk of hepatitis C virus infection is estimated at between 3 and 10 percent. It increases greater than 10 folds if the source patient has high levels of virus load [12]. A lower risk of infection is found for HIV at less than 0.3 percent (cardo et al., 1997). It remains a challenge in terms of counseling individual caregivers with respect to their own personal risk of infection, for instance after a needle stick injury [13].
There are also divergent views on the risk factors associated with these infections in Nigeria. However, low levels of literacy, cultural practices including polygamy, poverty and lack of access to appropriate reproductive health services as well as nonchalant attitudes to HIV infection have been pointed out as definite risk factors at Makurdi, Nigeria [14]. To others lack of sincerity, poor funds administration, unclear motives and lax attitudes of government official toward national health issues has indirectly fuelled the spread of the infection.
Furthermore, there is a high prevalence of health conditions requiring blood transfusion in many parts of sub-Saharan Africa. Many endemic diseases such as malaria that result in anemia or reduction in hemoglobin levels, fatal automobile accidents, surgical and obstetric emergencies that necessitate blood transfusion as well as malnutrition are all rampant in the region. Thus, there is always high demand for blood, a situation that epidemiologically increases chances of transmission of viral hepatitis and HIV through contaminated blood. This view is aptly supported by reports that a significant proportion of the world’s blood supply particularly in the developing countries is either unscreened or poorly screened [15]. Hence, blood transfusion accounts for 5 to 10 percent of HIV and viral hepatitis in sub-Saharan Africa (Field and Allain, 2007), and 12.5 percent of blood transfused patients are reported to be at risk of post transfusion hepatitis [16].
Often times in emergency situation, national medical response team (NMRT) who are equipped to handle victims of accidents may not be present thereby exposing non-health workers and untrained health personnel who in attempt to save life fail to observe the safety precautions leading to the risk of infection transmission. For this reason, this research work is aimed at determining the prevalence of some blood borne viral infections among road accident victims and its clinical implications.
Aim
The aim of this study was to determine the prevalence of some blood borne viral infections among road accident victims.
Materials and Method
This investigation was carried out at Federal Teaching Hospital Abakaliki, which is a major hospital in
Ebonyi State Located at the South Eastern part of Nigeria.
This study was carried out on road accident victims of both males and females of different age groups.
Two milliliters of venous blood was collected from 110 subjects each through vene-puncture at the antecubital
fossa and placed in a clean plain tube. The samples were allowed to clot and then centrifuged for 5
minutes. The serum was used for analysis.
Approval was obtained from the Ethical and Research Committee of Ebonyi State University Abakaliki.
Written and oral informed consent was obtained from each subject prior to sample collection.
The method used was immunoehromatographic method sourced from abbot determine HIV ½.
The samples were centrifuged and the sera extracted. The protective foils cover was removed from each test
kits (HIV-1 and HIV-2 determine kits). About 50 microlitres (uL) of the sera were applied to the sample
pads with the aid of Pasteur pipette. They were kept for 15 minutes (up to 60 minutes) and results were read.
The method used was one step immunochromatographic HBsAg test strip by Qumica Clinica Applicade
(QCA).
The retracted blood samples were spun for 5 minutes. The expressed sera were collected in clean test tubes.
The strips were immersed into the tubes containing the sera. The results were read after 10 minutes.
One step immunochromatographic method by ACON-HCV was used. It detects the presence of antibodies
to hepatitis C antigen using a membrane based immunoassay. It takes 6 to 8 weeks following infection
before the immunoassay will yield a positive result.
The procedure is the same with that of HBV except that simple HCV repid kits by ACON were used for
HCV test.
Data were expressed as percentage. Chi-square test was used to establish relationship between the observed
and expected. The statistical package used was SPSS 20 for windows. Statistical significance was set at P<
0.05.
Results
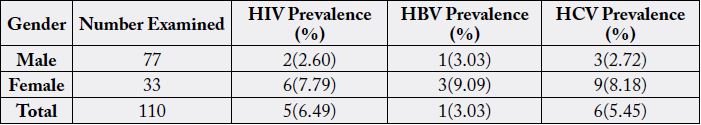
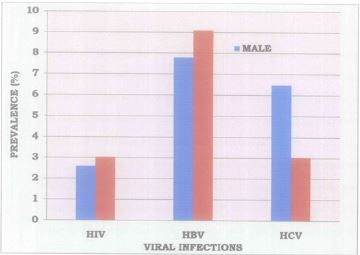
The result of this study showed that among 110 subjects studied, 77 (70%) were males while 33 (30%) were
females. A total of 18 (16.36%) were positive for the three viral infections while 92(83.64%) were negative.
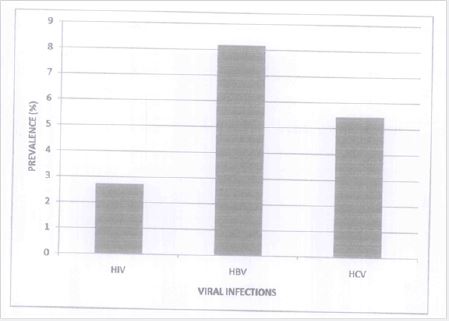
The number of subjects infected with HIV are 3(2.72%), 9(8.18%) were HBV positive while 6(5.45%)
were HCV positive. Out of the 3 HIV infected, 2(2.60%) were males while only 1(3.03%) was female.
Six (7.79%) out of the 9 HBV positive subjects were males while 3(9.09%) were females. Out of 6 HCV
positive subjects, 5(6.49%) were males while 1(3.03%) was female.
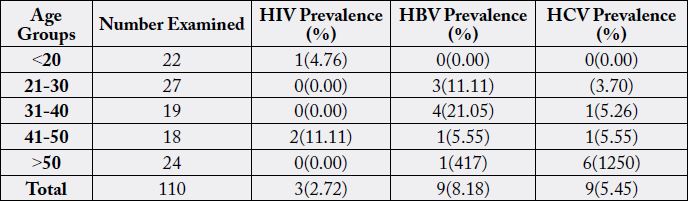
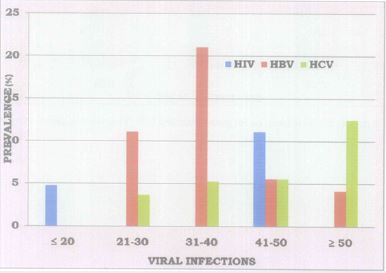
From table 1, HIV has a higher prevalence among age group between 41 to 50 than in any other age groups studied. HBV was more prevalent in subjects between 31-40 years, 4(21.05%). HCV was more prevalent in subjects greater than 50 years. Single case of co-infection was observed with HBV and HCV.
Discussion
Human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV) have similar
pattern of infection, mainly through exchange of blood and blood products, sexual intercourse and vertical
transmission (that is from mother to child) health care workers (HCWs) are exposed to these blood borne
pathogens. Infections by these agents often lead to chronic and fatal illness, which are expensive and difficult
to treat.
The findings from this study provided both supporting and conflicting result. High HBV prevalence of 9 (8.18%) was observed in this study when compared to HCV with prevalence of 6 (5.45%) and HIV prevalence of 3(2.72%), agree to the research recorded by Emmanuel et al. (2014) [17] who observed high HBV prevalence among groups that were considered low risk such as accident victims (16.2%) and blood donors (15.3%), when compared to HCV and HIV. High HBV prevalence recorded in this study may be due to the rate at which HBV is transmitted. Comparison of these three viral infections showed that HBV is extremely easy to transmit; HCV is easy to transmit while HIV is not easy to transmit. Another reason for this could be due to high rate of awareness and priority given to HIV without corresponding alertness to HBV. In Federal Teaching Hospital Abakaliki (FETHA) for instance, there is HIV clinic but no HBV clinic. In contrast to this study, Odimayo et al. (2010) [18] reported high HIV prevalence of 27.5% than HBV and HCV in their study in Abwa, a rural community in Benue state. This disagreement could be because of current awareness geared toward HIV in Ebonyi State. High HBV prevalence reported could pose high risk on health care workers and others who may be of assistance in safe guarding the lives of these victims and so, the health workers should be vaccinated against HBV. Also safety precaution must be adhered to since HBV is extremely easy to transmit.
Co-infection with HBV and HCV observed in this study is in accordance to co-infections with HIV, HBV, and HCV reported by other researchers [19]. Co-infection with HCV/HIV and HBV/HIV were observed by Chukwurah and Nneli (2005) [20] in Enugu, South Eastern State of Nigeria. It has been document that co-infections with HCV in individual infected with HFV is associated with a high incidence of liver injury, hepatitis decomposition and decreased survival time than that seen in HIV mono-infected population (Agwale et al., 2004). The reason for these co-infections may be because these viruses share common transmission pathway mainly through blood, vertical and sexual intercourse.
High prevalence of these viral infections was observed among males when compared to females as shown in table 1. This result is in contrast to Erhabor et al. (2007) [21] who recorded high prevalence of these infections in females 61.5% than males with prevalence of 38.5%. This contrasting result may be due to the 48 number of either males or females involved in the study as higher number may tend to give high prevalence. The result of this study is in line with the study by Emmanuel et al. (2014) [17] who recorded high HBV prevalence of 14.3% in males 11.0% in females. This may be due to promiscuous (Polygamous) life style of males when compared to females. In respect to age, prevalence of the three viral infections was seen more in subjects above 20 years than those below 20 years as shown in table 2. This could be because; people above 20 years are more sexually active than those below 20 years as unprotected sexual behaviour is the most important means of contracting these infections [22].
Conclusion
In conclusion, hepatitis B virus has been found to be more prevalent among road accident victims and for
this reason, health care workers especially those in emergency department should be vaccinated against
HBV and also abide strictly by the standard precaution to reduce or avoid the risk of transmission of these
blood borne infections since there were also positive cases in hepatitis C virus and human immunodeficiency
virus. Nevertheless, additional study using different criteria (subjects) might be useful to further estimate the
prevalence of these virals infections in Ebonyi State.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!