Biography
Interests
Khalid S. Aljabri, MD, FRCPC, FACP1*, Ibrahim M. Alnasser, MD2, Facharatz2, Samia A. Bokhari, MD, SBEM1, Muneera A. Alshareef, MD, SBIM1, Patan M. Khan, MD, MRCP1, Abdulla Mallosho, MD1, Hesham M. AbuElsaoud, MD1, Mohammad M. Jalal, MD, Rania F. Safwat, MD1, Rehab El Boraie, MD1, Nawaf K. Aljabri, MLT3, Bandari K. Aljabri, MS4, Arwa Y. Alserihy, MS4 & Amjad I. Hawsawi, MS4
1Department of Endocrinology, King Fahad Armed Forces Hospital, Jeddah, Kingdom of Saudi Arabia
2Department of Radiology, King Fahad Armed Forces Hospital, Jeddah, Kingdom of Saudi Arabia
3Department of Laboratory, Northern Armed Forces Hospital, Hafr Al-Batin, Kingdom of Saudi Arabia
4College of Medicine, Um Al Qura University, Makkah, Kingdom of Saudi Arabia
*Correspondence to: Dr. Khalid S. Aljabri, MD, FRCPC, FACP, Department of Endocrinology, King Fahad Armed Forces Hospital, Jeddah, Kingdom of Saudi Arabia.
Copyright © 2019 Dr. Khalid S. Aljabri, MD, FRCPC, FACP, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
To estimate retrospectively the frequency of hyperprolactinemia in patients with primary empty
sella (PES).
All MRI pituitary records were collected from the radiology department data base between January
2008 and November 2018 at King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia. MRI,
clinical Records and serum prolactin of patients were thoroughly analyzed. Serum prolactin <324mU/l was considered to be normal for our laboratory reference.
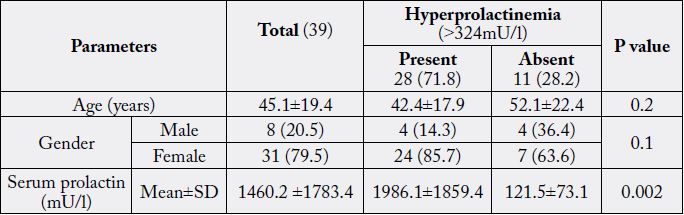
Over the 10-year period, 39 subjects were identified to be diagnosed with PES. There were 8
(20.5%) male and 31 (79.5%) were female with mean age 45.1±19.4. The mean and median serum
prolactin were 1460.2±1783.4 and 604 respectively. Among them we found 28 (71.8%) cases with
hyperprolactinemia. Among cases of hyperprolactnemia, there were 24 (85.7%) cases were female
and 4 (14.3%) were female with male to male ratio of 6.0 to 1.0 p=0.1. Cases with hyperprolactinemia
were nonsignificantly younger than cases with no hyperprolactinemia, 42.4 ±17.9 vs. 52.1±22.4
respectively, p=0.2. There were a nonsignificant decreasing trend of Cases with hyperprolactinemia
over advanced age groups which was predominant in females. Serum prolactin level significantly
correlated negatively with increasing age, r= -0.3, p=0.04.
In our study, the frequency of hyperprolactinemia in patients with PES was high and was more
common in middle aged female. Larger cooperative studies involving diverse population samples
could help to provide further information on the true frequency nationally.
Introduction
Empty sella (ES) is characterized by the herniation of the subarachnoid space within the sella, which is often associated with some degree of flattening of the pituitary gland [1-3]. The condition was first described in adults by Busch in l951 [4]. In the case of primary empty sella (PES), several etiopathogenetic hypotheses have been proposed, including a congenital incomplete formation of the sellar diaphragm and supra sellar factors such as stable or intermittent increase in intracranial pressure as well as volumetric changes in the pituitary [1-3,5]. On the other hand, secondary empty sella may be caused either by pituitary adenomas undergoing spontaneous necrosis (ischemia or hemorrhage) or by infective, autoimmune, and traumatic causes or by radiotherapy, drugs, and surgery.
Hyperprolactinemia is the most common endocrine disorder of the hypothalamic-pituitary axis. It is estimated to occur in 9%-17% of women with reproductive disorders [6]. There is a wide variation in the reported prevalence of endocrine abnormalities in PES. It was noted that endocrine dysfunction in 50% of PES patients while De Marinis et al. found endocrine abnormalities in 19%. Hyperprolactinemia was the most common endocrine abnormality observed [2,7]. In PES particularly, mild hyperprolactinemia has been frequently reported [7]. This is thought to be due to pituitary stalk compression as a consequence of the remodeling of the hypothalamo-pituitary region and altered cerebrospinal fluid dynamics. The differential diagnosis of hyperprolactinemia includes hypothalamic/pituitary tumors, of which the prolactinoma is the most common [6]. The importance of recognizing ES resides in its superficial resemblance to pituitary tumours. In some cases, the roentgenographic and hormonal manifestations of ES syndrome can be almost identical to those pituitary tumours. The objective of this study, therefore, is to estimate retrospectively the frequency of hyperprolactinemia in ES cases.
Methods
All MRI pituitary records were collected from the radiology department data base between January 2008
and November 2018 at King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia. MRI and clinical Records
of patients were thoroughly analyzed. Out of the initial screening of 630 subjects, 39 subjects were identified
to be diagnosed with PES. Information was collected from two resources such as clinical case records of
subjects seen at the endocrinology or other services and the data on hormonal analysis. Serum prolactin
<324mU/l was considered to be normal for our laboratory reference. The total number of cohort were
separated on basis of age values into three groups: <40 years, 40-59 years and ≥60 years.
Continuous variables were described using means and Standard Deviations . Univariate analysis of baseline
demography both between groups, were accomplished using unpaired t-test and nonparametric and Chi
square test were used for categorical data comparison. Pearson correlation between variables. P value <0.05 indicates significance. The statistical analysis was conducted with SPSS version 22.0 for Windows.
Results
Over the 10-year period, Out of the initial screening of 630 subjects, 39 subjects were identified to be
diagnosed with PES. There were 8 (20.5%) male and 31 (79.5%) were female with mean age 45.1±19.4,
table 1. The mean and median values were 1460.2±1783.4 mU/l and 604 mU/l respectively. Among them
we found 28 (71.8%) cases with hyperprolactinemia were 24 (85.7%) cases were female and 4 (14.3%) cases
were male with female to male ratio of 6.0 to 1, p=0.1. Cases with hyperprolactinemia were nonsignificantly
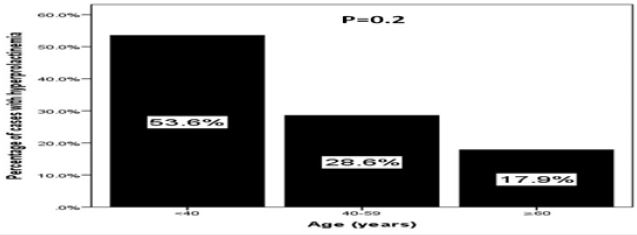
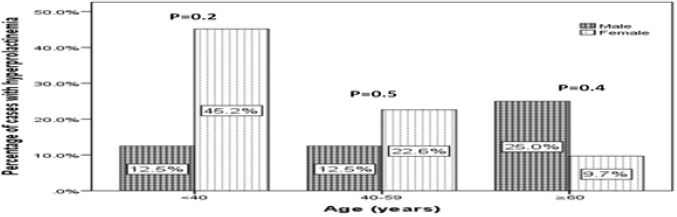
younger than cases with no hyperprolactinemia, 42.4±17.9 vs. 52.1±22.4 respectively, p=0.2. There were
a nonsignificant decreasing trend of Cases with hyperprolactinemia over advanced age groups which was
predominant in females., figure 1 and 2. Serum prolactin level significantly correlated negatively with
increasing age, r= -0.3, p=0.04.
Discussion
There is a wide variation in the reported prevalence of endocrine abnormalities in PES. Prolactin (PRL)
is unique among the pituitary hormones in that the predominant central control mechanism is inhibitory,
reflecting dopamine-mediated suppression of PRL release. This regulatory pathway accounts for the
spontaneous PRL hypersecretion that occurs with pituitary stalk section, often a consequence of compressive
mass lesions at the skull base [8]. Normally in PES, the pituitary stalk is compressed, thereby dopamine does
not reach the pituitary gland. Hence PRL levels are increased.
Hyperprolactinemia and intermittent increases in PRL levels have both been associated with the PES, and as many as 25% of women with an ES have elevated PRL levels which is lower than our result (85.7%). Hyperprolactinemia has been frequently associated with PES with incidence ranging from 10-37.5% according to the literature, and it has been proposed as the most common endocrine abnormality [2,7,9]. Ghatnatti et al. noted endocrine dysfunction in 50% of PES patients and hyperprolactinemia was the most common endocrine abnormality observed in their study [7]. The degree of hyperprolactinemia found in ES syndrome is moderate (usually less than 2100mU/l) compared to prolactinomas with levels greater than 4200mU/l) which is within our finding (1460mU/l) [10].
We found the prevalence of hyperprolactinemia was more prevalent in cases younger than 40 years and there were a nonsignificant decreasing trend of Cases with hyperprolactinemia over advanced age groups which was predominant in females, figure 1 and 2. Female predomonance was found by others [9]. PES occurred with the greatest frequency at the fourth decade which was older than our result [11]. In a large epidemiological study, signs of primary empty sella were found in 140 out of 500 (38%) consecutive patients, aged 11-82 years, who underwent MRI imaging of the brain for a variety of conditions not related to pathologic processes of the sellar or juxtasellar regions [9]. Treatment of patients with PES consists in appropriate hormonal substitution for the detected deficits and correction of hyperprolactinemia with dopamine agonists in patients with symptoms of this condition [2].
We aimed to identify the frequency of hyperprolactinemia in patients with PES as screened by MRI scans. Furthermore, due to the retrospective nature of this study, the observed population reflects a selected yet comprehensive group of patients referred for pituitary MRI, rather than the general population as would be encountered in an autopsy series. Our study could be limited by the question of clustering of cases within the study region and the effect that might have on our estimates, in addition, the current study population may appear limited in size and therefore may underestimate the true frequency of hyperprolactinemia in the general population. In addition, the study shares the limitations of all retrospective studies.
In conclusion, in our study, the frequency of hyperprolactinemia in patients with PES was high and was more common in middle aged female. In the absence of registry data, larger cooperative studies involving diverse population samples from multiple centers could help to provide further information on the true frequency nationally.
Acknowledgement
The author would like to thank all colleagues from the Department of Endocrinology for helping in data
collection.
Conflict of Interests
The authors declare no conflict of interests.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!