Biography
Interests
Daniel Neuspiel, R.1*, Cragin Greene, W.2 & Jennifer Baxley, C.1
1Department of Pediatrics, Atrium Health, USA
2Center for Advanced Practice, Atrium Health, USA
*Correspondence to: Dr. Daniel Neuspiel, R., Department of Pediatrics, Atrium Health, USA.
Copyright © 2018 Dr. Daniel Neuspiel, R., et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
New advanced clinical practitioners (ACPs = nurse practitioners and physician assistants) seeking
positions in pediatric primary care have been hampered by lack of clinical experience.
A 12-month postgraduate fellowship program in primary care pediatrics was initiated for new
ACPs to improve their readiness for independent practice. Fellows participated in weekly team
learning discussions, monthly case presentations, quality improvement activities and supervised
pediatric office care.
From 2014-2017, 11 fellows completed the program and 2 are currently enrolled. All graduated U.S.
physician assistant (N=5), pediatric nurse practitioner (N=5), or family nurse practitioner programs
(N=3). All fellow graduates received job offers.
This fellowship program has been effective in moving ACP graduates into busy pediatric practices.
Future goals include competency-based fellow evaluations, assessing the impact of training
on patient outcomes, improved clinical site recruitment and implementing pre- and post-test
knowledge inventories that reflect the current fellowship curriculum.
Abbreviations (if used)
ACP: Advanced Clinical Practitioner
CAP: Center for Advanced Practice
CHS: Carolinas Healthcare System
FTE: Full Time Equivalent
IOM: Institute of Medicine
FNP: Family Nurse Practitioner
NP: Nurse Practitioner
PA: Physician Assistant
PNP: Pediatric Nurse Practitioner
VA: Veterans Administration
Introduction
A growing number of new nurse practitioners (NPs) and physician assistants (PAs), referred to jointly as
advanced clinical practitioners (ACPs), have sought positions in pediatric primary care, yet consideration
for hiring them has been limited by their lack of clinical experience, since practices recruiting ACPs may be
reluctant to hire inexperienced and/or inefficient clinicians. In a 2010 report, the Institute of Medicine (IOM,
recently renamed The Health and Medicine Division of the National Academies of Sciences, Engineering,
and Medicine) recommended a required postgraduate residency for nurses [1], noting increasing evidence of
cost-effectiveness of such training, although the authors observed that most of these programs to date have
been based at hospitals and focused on acute care. The IOM called for programs outside of acute care settings
to be developed and evaluated. Although the IOM recommended mandatory postgraduate training, others
believe such programs should be optional, but encouraged for new ACPs or those moving to new settings.
Team-based residencies may be of particular value to provide opportunities to improve collaboration and
training in patient-centered care [2].
The first postgraduate training program for PAs was established in New York in 1971 [3], and the initial NP residency was started in Connecticut in 2007 [4]. Postgraduate programs for ACPs have been referred to as both residencies and fellowships. Some nurses favor the term fellowship because an NP can obtain certification and licensure immediately after completing clinical training and may be more qualified for independent practice than a beginning medical resident [2].
Survey research among ACPs has supported the need for postgraduate training. Among attendees at 2 large national NP conferences in 2004, 10% of respondents perceived they were very well prepared for practice after their graduate education, while 51% felt they were only somewhat or minimally prepared [5]. Among respondents, 87% would have been interested in a residency program had one been available upon their graduation. In a survey of attendees at a regional NP residency forum in 2013, high impact/ high feasibility aspects of a NP postgraduate training were considered to be: development of strong evaluation component to quantify program results, commitment of successful resident to clinical skills mastery and developing awareness of role as team member, and outcome goals that include increased number of patients seen, administration of a burnout survey, reduced readmission rates, and orientation cost savings [6]. These investigators concluded that NP residencies must include training that is interprofessional, with components on leadership, policy, quality improvement and scholarship, diagnostic skill honing, and with dedicated mentorship and role development.
Graduates of PA postgraduate training were surveyed in 2014 to explore perceptions of efficacy and utility of such programs [7]. After completing postgraduate training, 97% of respondents felt more competitive for jobs, 74% believed time to full productivity was decreased, and 95% recommended completion of a similar program. Respondents thought the programs enhanced their professional careers, but recognized that during postgraduate training, PA residents earned 40% to 50% less than their counterparts who went directly into the workforce.
Elements of successful ACP postgraduate programs in primary care have been reported by several investigators. Meyer et al [8] studied the effect of a combined nursing/medical training model on professional identity and team development within the Connecticut Veterans Administration(VA) health system, demonstrating early evidence of successful interprofessional collaboration among NPs and internal medicine residents in a primary care training program. Goudreau et al [9] describe a 12-month NP residency within the VA system with a collaborative multidisciplinary team approach. The core concepts of this program included ensuring smooth transition into care, increased accountability of the new NP, socialization and networking with colleagues, collegiality, and mentoring support. Flinter et al [3] describe a 12-month residency for family nurse practitioners(FNPs) in primary care. Key components of this program were precepted clinics, specialty rotations, independent clinics, and didactic sessions. This program prioritized training for complex patientcentered, team based, comprehensive care with a structured, community-focused orientation. The authors describe a competitive application process with national recruitment, followed by interview of finalists and selection of candidates. Tracked resident data included preceptor evaluations, visit volume, patient panel size and composition, diagnoses addressed and procedures performed. In addition, learners evaluated each element of the program throughout the year and submitted a weekly reflective journal. Costs of this program included resident salary and benefits, program coordinator compensation, lost preceptor revenue related to decreased direct patient care volume, facility overhead and administrative expenses. To date, we are aware of no published reports of postgraduate residency or fellowship programs combining NPs and PAs, nor any such programs in primary care pediatrics.
Materials and Methods
In April 2014, we initiated a 12-month postgraduate fellowship program in primary care pediatrics open
to new ACPs or those changing career direction, based at Carolinas Health Care System (CHS, recently
renamed Atrium Health) in Charlotte, North Carolina. This program was one of several ACP fellowships
including acute care (urology, medical critical care, surgery, cardiology, hospital medicine, palliative care,
emergency medicine, cardiothoracic surgery), primary/ambulatory care (pediatrics, family medicine, internal
medicine), urgent care (general or pediatric) or hybrid programs (behavioral health, pediatric neurology,
pulmonology, oncology, women’s health) that have been established at the Center for Advanced Practice
(CAP) of CHS since 2013.
We recruited fellow applicants through contacting and visiting ACP training programs, attending ACP conferences and internet visibility. We then implemented a competitive application and interview process.
After selection of fellows, the first 3 weeks of the primary/ambulatory care fellowship programs included a joint core curriculum focusing on general orientation, clinical assignments, office skills, patient interactions and professionalism. The pediatric primary care fellowship program then offered weekly half day team learning discussions using a flipped classroom model [10] (also attended regularly by family medicine fellows and intermittently by urgent care fellows), monthly case presentations at CAP offices and supervised patient care as licensed ACPs in pediatric offices located in the Charlotte, North Carolina area.
The goals of the fellowship were:
• To allow ACPs to attain improved clinical outcomes while obtaining knowledge and expertise needed to practice at the top of their licenses;
• To achieve specialty specific competencies to prepare them for critical thinking above the level received in their prelicensure education;
• To expand their knowledge of evidence-based practice with a gradual ease into independence;
• To expand the pool of qualified ACPs available for CHS positions.
From April 2014 through March 2017, applicants were admitted every 6 months, enabling junior (first 6 month) and senior (last 6 month) fellows to interact together at team learning discussions convened by either a pediatrician medical director or a pediatric ACP fellow coordinator. We selected learning topics and readings primarily from a recognized pediatric primary care resident physician curriculum, augmented with some new topics and updated readings.
Fellows were each assigned a pediatric primary care clinical site and supervising physician within our health system network. For the first 6 months of the fellowship, they spent 4.5 days weekly at their pediatric primary care site and one half day in the team learning session. During the second half of the fellowship year fellows spent 4 days at their primary care site, ½ day in a pediatric subspecialty office and ½ day in team learning discussion. Subspecialties included: allergy/immunology, cardiology, child protection, dermatology, endocrinology, gastroenterology, genetics, nephrology, neurology, newborn nursery, oncology, ophthalmology, orthopedics, orthotics/prosthetics, otolaryngology, pulmonology, urology, and urgent care. All fellows were required to do a quality improvement project and present the results to other fellows and faculty at a session at the end of the fellowship year.
Fellows were evaluated monthly by their supervising physician and were invited to give regular feedback on their clinical experiences by the fellowship coordinator. Fellows completed a 50-item multiple-choice knowledge inventory at the beginning and end of the fellowship based on this curriculum.
Budgeted staff for the fellowship included a medical director (10% FTE), ACP coordinator (10% FTE), and shared staff from CAP. Fellows were salaried at approximately 65% of the starting salary for ACPs at CHS, and were offered a $20,000 USD retention bonus for remaining employed with our system for 2 years post-fellowship as well as 2 years of experiential credit for the one year program, enabling them to start postfellowship employment at a higher pay scale. Clinical site supervising physicians were not compensated, but their practices collected revenue generated by the fellow’s patient care billing. The clinical practices also enjoyed the benefit of trialing a potential new provider at no direct cost to their site budget.
Results
The numbers of applicants, interviewees and selected fellows are listed in the Table. As of March 2017, 11 pediatric ACP fellows completed the program and 2 are currently enrolled. The fellows were all recent graduates of U.S. PA (N=5), pediatric nurse practitioner (N=5), or FNP programs (N=3). The fellows completed their graduate professional education in eight states: North Carolina (3), Massachusetts (3), Virginia (2), and one each in Tennessee, Florida, Alabama, Texas and Pennsylvania.
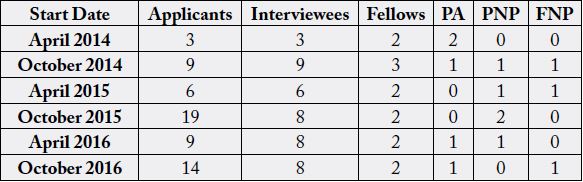
PA: Physician Assistant
PNP: Pediatric Nurse Practitioner
FNP: Family Nurse Practitioner
Among the 11 program graduates, 7 (64%) were hired by our health care system at the conclusion of the fellowship, most often in the same practices where they were based for clinical training during the program. The remaining 4 were recruited by our system but chose to work elsewhere. The average pre- and post-test knowledge inventory results for graduated fellows were 69% and 78%, respectively (p=0.0007, paired t-test), with all fellows demonstrating improved scores. Fellow feedback was uniformly positive about the program.
Discussions
After successful implementation of a novel postgraduate pediatric fellowship program for ACPs, we have encountered the following challenges and areas for improvement:
• Need for more objective, competency-based evaluations of fellows: we plan to institute an evaluation system based on pediatric residency milestones that will be implemented twice during the fellowship year.
• Alignment of evaluations with changes in curricular content: the originally designed didactic curriculum, evaluation methods and clinical experiences have changed as the program has matured over the 3 years since its inception. We plan to implement pre- and post-test knowledge inventories that align with curricular content.
• Difficulty in locating clinical sites to accept fellows and variability in fellow applicant numbers: as of April 2017 we changed to an annual admission cohort of 2 or 3 fellows to begin each October in order to allow a larger applicant pool and to facilitate recruitment of sponsoring clinical sites.
• Lack of information on the long-term benefit of this program: the impact of postgraduate ACP training on patient care outcomes, clinical efficiency, quality of care, job satisfaction and retention merits further study. We aim to follow these outcomes going forward.
Our findings support the conclusions of Harper et al [11] and Hussaini et al [12] that academically rigorous postgraduate programs for ACPs may promote the development and standardization of curricula and competencies with the goal of enhanced clinical rigor, and that future research directions in this area should include measurement of job satisfaction, clinical competencies, and patient satisfaction.
Conclusions
A unique fellowship program in primary care pediatrics was successful in training postgraduate ACPs
coming from diverse professional disciplines and retaining most of them in our healthcare system.
Acknowledgements
This research was presented in part at the Pediatric Academic Societies, May 9, 2017, San Francisco.
Conflicts of Interests
The authors report no conflicts of interest.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!