Biography
Interests
Elizabeta Popova Ramova* & Leonid Ramov
Training Implementation Center, Bitola, R.Macedonia
*Correspondence to: Dr. Elizabeta Popova Ramova, Training Implementation Center, Bitola, R.Macedonia.
Copyright © 2018 Dr. Elizabeta Popova Ramova, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Rehabilitation for patients with stroke is generally divided in acute, sub-acute, and chronic stage. Tertian prevention is based on activities for stroke survivors like community-based rehabilitation to increase quality of life (QOL), usually until the end of life. The purpose of our research was to assess the QOL of stroke survivors and the level of tertian prevention in our society.
We had 80 stroke survivors, with minimum 2 years passed after stroke, they were from the southwest
region of our country, divided in two groups according to their place of living. Group A, living in
town, and group B living in villages. The assessment of QOL was done with SS-QOL, and a
questionnaire for socioeconomic and healthcare data.
60% male and 40% female, with age over 65 and with left side disability 65%, were all analyzed.
Acute rehabilitation was present in (65%), subacute in(100%), and tertian prevention in 40%,
orthotic and healthcare supplies were used in 47%, medication in 100%, social help was given to
50%, 95% live with their family, and 55% were receiving their own funds. The QOL assess with
SS-QOL scale was 49% from Group A, and from Group B 45%
The WHO defines quality of life as an “individual’s perception of their position in life in the context
of the culture and value systems in which they live in relation to their goals and expectations.
Health-related quality of life instruments commonly comprise physical, social, and mental domains,
aligning with the notion that health is a state of complete well-being and not just an absence of
disease.
most of stroke survivors have complete health care in acute and subacute stages, but QOL is 49-41
or they need help from other person. They live with their families, and home rehabilitation program
can increase QOL.
Introduction
Stroke is one of the leading causes of death among the population [1]. This is due to the high prevalence and
increase of patients with increased body weight, type 2 diabetes, stress, poor lifestyle and increased blood
pressure [2,3]. Stroke management programs are established in many modern Health systems world-wide
[4]. The good management of emergency interventions and medications at the intensive care units, led the
survival rate after stroke over 60%. The guides for patients after a stroke consist of the emergency procedures
for emergency services, then the activities and interventions in the intensive care unit, followed by either as
being a neurology of internist patient, and a more comprehensive rehabilitation program that includes more
health services and social worker, speech therapist and psychologist [5]. With the activities in the field of
physical therapy in the acute, post-operative and chronic phase, it is important to improve the motor and
sensory functions, as well as to be able to provide for the adult population and professional rehabilitation
[6,7]. For a good quality of life after 1-2 years after stroke, interventions from the health and social segment
of the society are needed, in order to reduce the disability in stroke survivors, and the extra costs. With
interventions within tertiary prevention and rehabilitation at home, it can improve QOL in stroke survivors
[8,9]. This service should ensure mobility of patients, use of public transport, prescribing devices, continuous
rehabilitation through various forms of outside health institutions and assessment of nutrition and health
care [10,11]. In our healthcare system, patients have primary, secondary and tertiary health care, which is
borne by health insurance.
The aim of our research was to determine the quality of life in patients after stroke in the rural and urban environment
Material and Method
For the realization of our research, we applied a questionnaire for obtaining data from 40 patients living in urban environment and 40 living in the rural environment, from the southwestern part of Macedonia. The questionnaire consisted of several parts: 1) personal data (sex, age, side of confiscation, comorbidity), social status, supported person or person with their own means of funding, 2) assessment of primary healthcare (whether there is available prescription of drugs, how many times does he/she measure their blood pressure weekly, whether there is a doctor at their place of residence) and an assessment of secondary health care (how the rehabilitation process started, how many times a year was on rehabilitation, 3) estimation of the use of medical devices, 4) assessment of the functional ability after a stroke with SS-QOL scale. Criteria of inclusion in the research: to live with a family, to have no aphasia, and that there has been a minimum of 2 years passed after the stroke.
The applied questionnaire for assessing the quality of life of SS-QOL consists of 47 questions for 12 assessments, of which 1 full point is given for full assistance. 5. The maximum score in our examined groups, namely A-town environment and B -Rural environment, for each of them was 47Х5Х40 = 9400 points. In addition, 0-20% strongly dependent, 21-40% can do quite a lot of things alone, 41-60% needs help, 61-80% needs a little help and 81-100% need no help.
We presented the data in tabular and graphical way and we determined the significance with T-test and difference of proportions and significance from p<0.05
Results
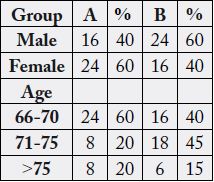
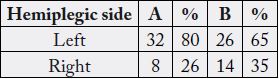
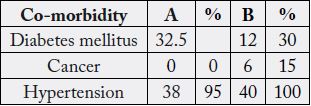
The data from part 1 of the questionnaire are showed in table 1 in terms of gender and age, and in terms of
hemiplegic side in table 2, and the co-morbidity in table 3.
In the urban environment, the percentage of respondents with a stroke, and with a younger age of up to 70 years, is higher. The representation of the female sex is greater in the urban environment compared to men in the rural environment
Marital status and social status are showed in Table 4, it is analyzed whether the family lives with the spouse and whether it has its own means of life (pension), and whether it receives a care supplement by another person.
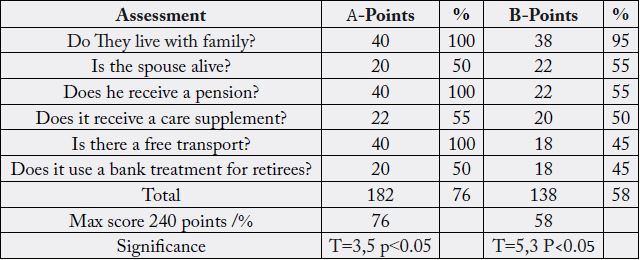
Both groups have significant high social status, it is better for people from town, T=1,08 p>0,05, but not significant.
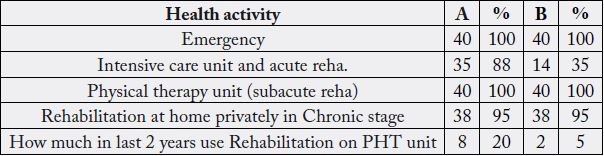
PHT-physical therapy unit
Both groups, did not use rehabilitation in hospitals, at least the last two years, T=18, P<0.05 it is significant and it can increase complications of discontinuation of rehabilitation process.
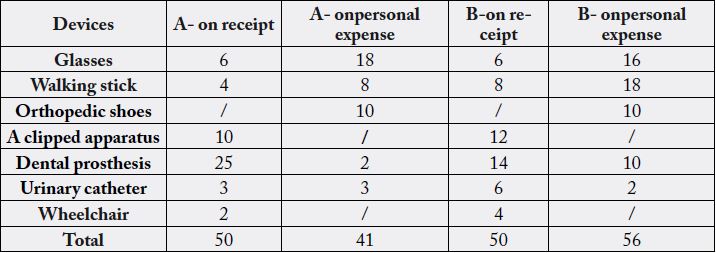
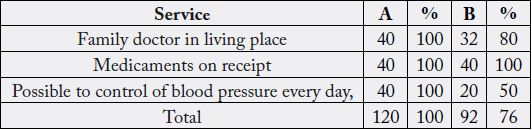
Patients living in the city needed 91 devices, 45% of them procured privately, while those in the village had a total need of 106 devices, 52% of which were procured privately. Obtaining prescription drugs, as well as the physician’s availability in the community, is shown in Table 7.
The assessment of quality of life is showed in table 8 for both groups of stroke survivors.
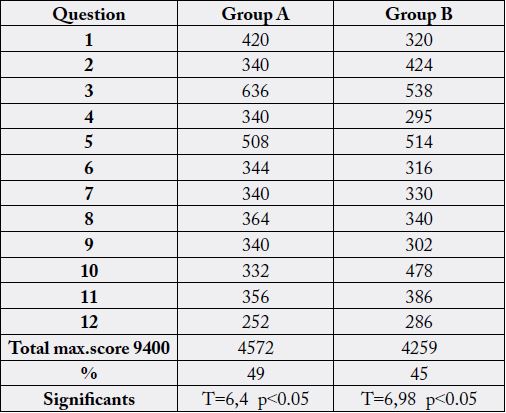
Both groups have significant low level of QOL.
Discussion
The quality of life after a stroke depends heavily on the rehabilitation in the acute, sub-acute and chronic
stages. It also depends of the economic conditions of impairment in which the patients’ needs should be
provided with assistive devices and tertiary prevention at the place of residence [12].
The social status of those living in the countryside is lower than those in the city in our research.
In highly developed and developed countries, despite good medical care and modern protocols that are managing these patients, the conditions and the quality of life depend on the level of health insurance [13].
Table 3 shows that hypertension is still a highly common disease requiring regular control of hypertension and drug regular therapy.
From table 7, we can see that primary health care in rural areas is less accessible and is represented by 76% for the same conditions of participation in the health care system, compared with patients from town.
In the middle-developed and underdeveloped countries, we are faced with the problem of lack of basic conditions for tertiary prevention and adaptive devices because of the low economic status of the patient and society. After acute care of the condition, patients do not have adequate rehabilitation because the situation is redistributed or preference is given for urgent cases and infectious diseases [14].
From Table 5 it can be noted that the emergency medical services were available to all but 88% of the city used the intensive care unit and only 35% of the village as they were mostly treated at home (perhaps because of the easier form of stroke). The home treatment, however does not give early and it is denied to these patients. They all had subacute rehabilitation, which is in the first 6 months after a stroke. Later, however in the chronic phase in order to maintain the condition because of the lack of rehabilitation at home, they applied home rehabilitation at a private expense.
Our country is middle-developed, where almost all people have health insurance and the same conditions for treatment in state hospitals, also rehabilitation carried out at the expense of the health care system is available only in hospitals, while the rehabilitation at home is only available if self-funded.
In our research, healthcare in terms of hospital treatment, the prescription of drugs and devices is the same regardless of the place of residence of the patient.
Both groups of patients showed that chronic rehabilitation was practiced on a personal burden of means, with a therapist at home (95%), and tertiary rehabilitation in the urban environment was 20%, while in rural 5%.
The devices that were bought by the health fund received both groups with a prescription, while the rest were at a personal expense, privately.
Both groups of patients with a pervading stroke over the age of 60 have a quality of life of 41-60% or need help, but all live with their families, which is also important for the care given to them, and therefore they are not accommodated in old people’s homes.
The assessment of the quality of life after a stroke can be introduced in the practice of the family doctor with one of the recognized scales as we did with the use of SS-QOL scale [15]. It is significant and gives good guidance on whether the patient will stay with the family or must be placed in a foster care facility.
Foster homes - working on the principle of paid private care, and medical interventions, medicines and aids on the burden of the health fund. Some families whose budget cannot pay the accommodation in the home are forced to keep the patients at home, without professional care and continuous rehabilitation, because it is not performed in home conditions [16,17]. Continuing life expectancy with interventions in the acute phase of treatment leads to a high survival rate [18].
The increased percentage of the old population and their care needs, as well as the large number of comorbidities, are perceived by the WHO as the leading demographic characteristic of the population in the 21st century; therefore, in their 21st century strategy, rehabilitation has become one of the five key strategies for incorporation in health systems around the world [19].
Rehabilitation in home conditions has not only improved the quality of life of the population, low and middle-developed countries, but also a positive economic benefit in terms of accommodation capacities and costs of care outside the family [20-22].
Developing tertiary prevention and rehabilitation in the community are opportunities for more economical, more accessible healthcare that will also give a better quality of life for multiple chronic illnesses, and not as we estimate for stroke survivors [23].
Conclusion
Rehabilitation programs in the acute and subacute phase are applied in our country according to the
standards introduced in the health care system around the world. The quality of life can be improved if home
rehabilitation is introduced, as opposed to inpatient treatment, whose facilities cannot meet the chronic
illness. The use of scales for assessment and good management of patients in domestic conditions has many
benefits, primarily early detection of risk factors, the patient is staying with the family, and the prevention of
inactivity complications, with greater economic benefits for the family and society.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!