Biography
Interests
Renee Reid, Connor Sheehy & Leila Jabbour*
Department of Health Sciences, Franklin Pierce University, 40 University Drive, Rindge, NH, USA
*Correspondence to: Dr. Leila Jabbour, Department of Health Sciences, Franklin Pierce University, 40 University Drive, Rindge, NH, USA.
Copyright © 2018 Dr. Leila Jabbour, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Hospital Acquired Infections (HAIs) are a concern globally, but are of particular importance in
developing countries with less funding and knowledge on the pathology of infection. HAIs pose
a serious health risk and economic burden to hospitals in areas such as Africa.
To determine risk factors and prevention methods for HAIs in Africa to help hospitals moving
forward.
Electronic databases were investigated for relevant articles. Studies published post 2000 regarding
HAI risk factors or interventions were eligible for data analysis and organized accordingly.
Eleven risk factor articles and five intervention articles were deemed eligible and were used in
this study. Significant risk factors proved to be surgery, department patient was admitted to, poor hand hygiene, and antibiotic use. The World Health Organization’s hand hygiene protocol proved
to be cost effective and accessible in African hospitals. Educational intervention was also effective
in improving the quality of care health care practitioners gave, and decreased the number of
HAIs.
There is an obvious lack of new interventions and the ones found focused on similar topics
of hand hygiene. More creative interventions need to be designed and implemented to fit the
explanatory models African healthcare providers use in their work lives.
Introduction
Nosocomial infections are infections acquired in hospitals and are a global public safety concern for patients
and health-care providers alike [1]. Hospital-Acquired Infections (HAI) result from care the patients receive
at hospitals and can manifest in the facility or after release. HAIs often develop in patients through the use
of invasive medical devices, at the site of surgical incisions, and from antimicrobial resistant pathogens [2].
In 2003 it was estimated that 20% of all nosocomial infections could be prevented [3]. These infections
are not limited to patients, but can also affect health care providers and any other hospital staff. In Africa
specifically, over 240 health care providers have contracted Ebola as a result of treating patients, half of
which died [4]. The primary modes of transmitting infections include direct contact, bodily fluid exchange,
or airborne transmission [2].
HAIs are a critical weakness to a system in place to improve health and are ongoing in prevalence and economic burden [1,5]. Developing countries struggle in terms of education and funding for their health care system and therefore HAIs pose a greater threat to their patients when compared to developed countries. As of 2011, the prevalence of HAIs in African countries ranged from 2.5%-14.8%, which is twice as high as European countries (7.1%) and considerably higher than the United States (4%) [1,5,6]. However, the true magnitude of infections in Africa is unknown because HAIs are often unrecognized and under-reported [1]. In terms of economic burden, one meta-analysis done by Zimlichman et al. found that roughly $9.8 million dollars in the United States alone are spent annually treating HAIs [5]. It is unknown how much money is spent in Africa on HAIs, however in 2012 Eritrea, Africa had the lowest total spending per person on health at only $12 per person [7]. The United States spent roughly $8,000 per person on health care in 2012 [7]. This shows that less money is being put towards healthcare and preventing disease in developing countries.
Currently there are no up to date systematic reviews covering the issue of HAIs in Africa. This article attempts to examine interventions and observations of 16 studies focused on African hospitals to update past research. Relative studies from other countries are also used to assist with developing our conclusions. Surgical site infections are among the most common forms of HAIs due to the exposure patients have to the world from open wounds or incisions made by surgeons. We will also observe different risk factors and interventions associated with preventing HAIs in this review. The objective of this systematic review is to assist hospitals in developing new guidelines and practices to prevent nosocomial infections from happening as often as they do.
Methods
Articles regarding HAI prevention and intervention in Africa were acquired using online databases such
as ProQuest, Academic Search Complete, and Google Scholar. Research began in September of 2017
and lasted until November of 2017. Search terms included “nosocomial infections”, “hospital acquired
infections”, “Africa”, “prevention”, and “intervention”. Abstracts of all articles were read to determine if they
were applicable. If they were relevant, a more in-depth analysis was done and the article was included in the
study. Articles were excluded if they were published before 2000 or if they were not original articles that
assessed risk factors or methods of prevention. Eleven risk factor articles and five intervention articles were
identified and analyzed.
Results
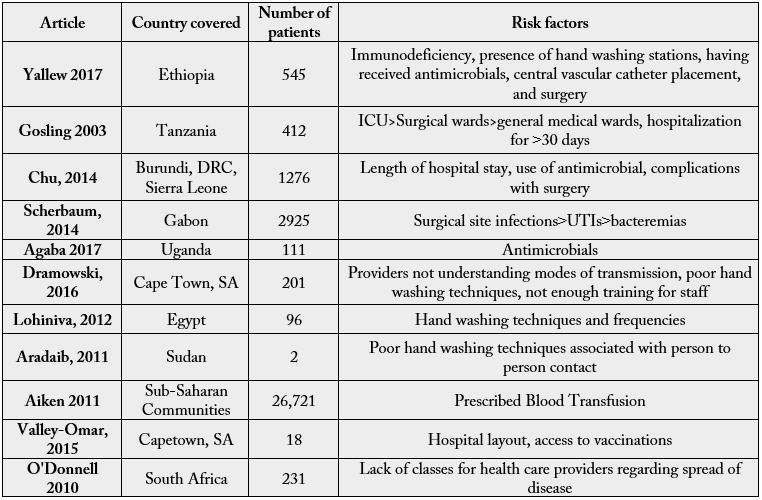
Identifying risk factors are an important way to assess causes for HAIs and help prevent them. Many
hospitals related risk factors were found in one matched case control study which monitored 545 patients
at two teaching hospitals in Ethiopia, Africa, 109 of which acquired infections during their admittance [2].
For each of these patients, the researchers investigated the presence of medical waste containers, antibiotic
use, duration of patient’s stay, patient’s immune status, use of invasive medical devices, and the department
to which the patient was admitted. Researchers discovered that patients who had medical waste devices
present in their rooms were 82% less likely to acquire infections. If patients received a general antibiotic, they
were 8.63 times more likely to become infected and 6.91 times if they had a central vascular catheter. The
researchers further determined that patients who underwent surgery or were immunocompromised were
2.35 times more likely to acquire an infection [2].
The department patients were admitted to also proved to be a risk factor. In one questionnaire-based, point-prevalence study, doctors and nurses in a hospital in Tanzania, Africa provided information about 412 inpatients of various departments to find which department had the highest prevalence of HAIs [6]. They discovered that 61 patients acquired infections (14.8%). Of these 61 infected patients, 40% of them acquired infections in the medical intensive care unit and 36.7% became infected in the surgical ward. The general medical ward accounted for 22.2% of the infections and the remaining 1.1% weren’t specified. The most common type of infection the researchers noticed were urinary tract infections and surgical wound infections. Other risk factors the researchers identified were if the patient stayed in the hospital longer that 30 days or if they were being transferred between health facilities [6].
Surgical site infection proves to be a major risk. One prospective, multi-country study observed four emergency obstetric programs in the Democratic Republic of Congo, Sierra Leone, and Burundi, Africa [8]. The researchers focused on 1,276 women who needed emergency cesarean sections from 2010-2011, 94 of which were diagnosed with an HAI at the site of surgical incision (7.3%). Other risk factors identified were hospital stays longer than seven days, young mothers, and surgical complications [8].
Similarly, a prospective case study in Gabon, Africa looked into the prevalence and risk factors of HAIs in the surgical, gynecology/obstetrics, and internal medicine departments [9]. Out of the 2,925 patients screened over the course of six months, 46 were diagnosed with an HAI (1.6%). 44% of these infections were surgical site infections, 26% were urinary tract infections, 20% were bacteremias, and the remaining 11% were other infections. The prevalence of HAIs was highest in the surgical ward, specifically after hysterectomies or cesarean sections. The researchers also found Staphylococcus aureus and Escherichia coli to be the most common pathogens infecting patients [9].
Certain types of injuries and medical devices also seem to be risky as well for HAIs. A cross sectional study focused on Ugandan hospitals aimed to determine the most common bacterial infections as well as antimicrobial susceptibility patterns. 111 adult patients were examined from two intensive care units [10]. Among the most common isolated bacteria were Klebsiella pneumoniae at 30%, Acinetobacter species at 22%, and Staphylococcus at 14%. Imipenem had the highest susceptibility rate for antibiotics with most of the bacterial species. Another factor to note is ventilator support and traumatic brain injury were associated the most with the development of nosocomial infection at P 0.003 and P 0.035 respectively [10].
Poor hand hygiene can lead to HAIs. A questionnaire administered at the Tygerberg Hospital in Cape Town, South Africa found infection control should focus largely on hand hygiene and stricter enforcement overall of good health practices [11]. 201 participants took the 37 item survey testing their knowledge and attitudes towards hospital acquired infections. There was a significant difference of the participants understanding good hand hygiene and infection transmission Albeit, medical/allied partners tended to score on the higher end of knowledge. Nurses did score higher in the attitude section compared to the other groups. Overall there was poor uptake to healthcare worker influenza vaccination and N95 mask fitting 25% and 28% respectively. 93% of participants agreed there should be more infection control training as well [11].
Another qualitative study about hand hygiene aimed to understand the behavioral determinants of hand hygiene in fourteen focus group discussions [12]. They were conducted with nurses in 2 university hospitals in Egypt. Nurses did not perceive the benefits of hand hygiene, and that they linked the need to wash hands to a sense of dirtiness. There was an obvious preference for soap and water compared to alternative products due to limited knowledge. “Environmental constraints, lack of role models and social control were identified as barriers for compliance with hand hygiene” [12].
Similarly, another study looked at the phylogenetics of the Multiple Crimean-Congo Hemorrhagic Fever in Sudan, Africa after a severe outbreak in hospitals [13]. The researchers specifically tested two infected patients to see if they had similar strains of the disease and found the two patients to have different strains of the same virus, making outbreak control difficult. Since the virus was found to spread through tick bites and contact with an infected person, the researchers indicated that a major risk factor for acquiring this infection in a hospital was poor handwashing techniques [13].
Bacteremia is a rising HAI with pressing concern at its rate. One prospective cohort study investigated the prevalence and cause of HAIs in children in the Kilifi District of Africa [14]. They analyzed data from 33,188 patients over a seven-year span and found that the risk of acquiring bacteremia in a hospital was .0059%, but the risk was rising 27% each year. The researchers also found that the mortality rate of patients with nosocomial bacteremia was 53%. Pathogens including Klebsiella pneumoniae, Escherichia coli, Staphylococcus aureus, Acinetobacter spp, group D streptococci and Pseudomonas aeruginosa were responsible for 75% of the infections. The risk factors identified were malnutrition and whether or not they received a blood transfusion [14].
Tracking diseases is an important way to prevent HAIs. One study examined the pattern of Influenza A/H1N1 epidemiology by introducing phylogenetic tracking patterns derived from 18 samples [15]. The implemented analysis suggested there were multiple instances of Influenza A entering a hospital via multiple patients. However, these patients carried identical strands suggesting traditional epidemiology would place the patients in a chain together despite a lack of contact. Analysis also suggested asymptomatic patients were also possibly involved with unknowingly spreading Influenza throughout the hospital [15].
HIV endemic areas also seem to be a risk factors. A retrospective study of 231 healthcare workers focused on determining the rate of multidrug-resistant tuberculosis (MDR-TB) in KwaZulu-Natal, South Africa [16]. Estimated incidence of MDR-TB hospitalization was 64.8 per 100,000 health care workers compared to 11.9 per 100,000 non–health care workers. It was clear in the retrospective analysis that health care workers were more likely to acquire tuberculosis in this HIV endemic area. Suggesting an urgent need for more infection control programs that deal with workplace environment infection control [16].
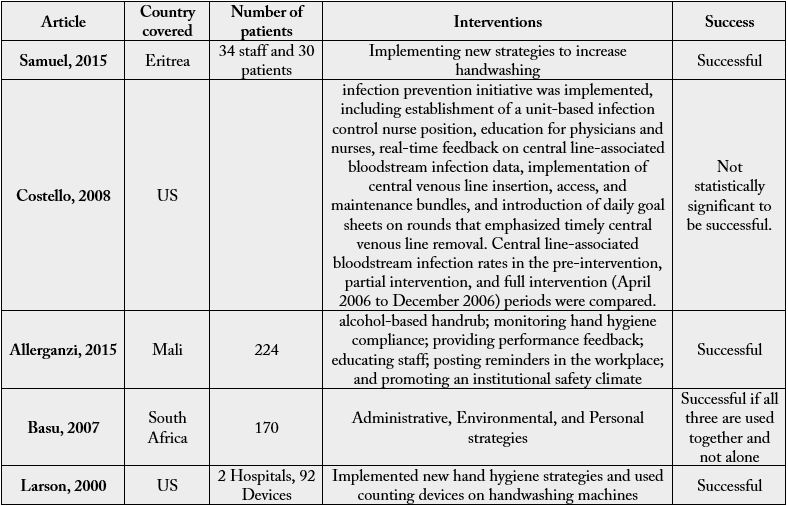
Testing new strategies that are inexpensive and increasing awareness and general knowledge are key in
preventing HAIs. In one qualitative study in a hospital in Eritrea, Africa, 34 hospital staff members and 30
patients were interviewed on their handwashing practices to determine the quality of care given to patients
to prevent infections [17]. They discovered that only 30% of the staff washed their hands after visiting
each patient, however all of the staff seemed eager to learn better hand washing practices. Researchers
offered incentives for handwashing and implemented educational programs for the staff, which improved
handwashing practices drastically. Post-intervention handwashing increased from 76% to 100%, cleaning
beds and bedside equipment increased from 12% to 87%, and the availability of isolation rooms for infectious
patients increased from 24% to 90% [17].
Increasing education about HAIs is close to being a statistically significant intervention. One retrospective, interventional study with a time-series design aimed to determine the efficacy of a nosocomial infection prevention protocol and its impact on HAIs, specifically central line associated bloodstream (CLAB) infections in the ICU [18]. The intervention involved further educating physicians, nurses, and hospital staff, promoting a nurse to a position more dedicated to infection prevention, and implementing a formal protocol when using a CLAB. Over the course of three years, rate of infections decreased from 7.8 infections per 1000 catheter-days to 2.3 infections per 1000 catheter-days, which was not statistically significant, but an improvement regardless [18].
Another education intervention did show education interventions to be helpful with a statistically significant margin. One before and after study in Mali, Africa, tested the efficacy of the World Health Organization’s multimodal hand washing improvement strategy to prevent infection [19]. This protocol included educational seminars on hand washing techniques, implementing alcohol based hand soaps, posting reminders at hand washing stations, and monitoring their performance to provide feedback to 224 health care providers. This practice was found to be successful as compliance increased from 8% to 21% which was statistically significant. Increases in safer handwashing practices lead to a staff more educated on infections and how to prevent them [19].
Mathematical models have also been used to determine interventions for hospitals. An epidemiological study focusing on extensive drug resistant tuberculosis examined several interventions and their effectiveness on preventing the spread of the disease [20]. Specifically, administrative, environmental, and personal infection were investigated using a mathematical model that relied on a two-year longitudinal inpatient and community-based data. In their predictions, the investigators predicted 1300 new cases of extensive drug resistant (XDR) tuberculosis. Wearing a mask alone could prevent fewer than 10% of these cases, and combining that measure with other preventative measures could increase prevention by 34-50% of these cases. This study shows that a combination of multiple interventions is the better course of action to preventing diseases [20].
Changing hand washing culture was also an effective intervention. A quasi-experimental study focused on improving handwashing while also examining the effectiveness of handwashing [21]. Two hospitals were part of the experiment and 92 handwashing devices were introduced with counters, integrated to trackZMM
Discussion
Public health safety is a pressing concern for healthcare providers and their support structures. Among
the discussion, HAIs are a frequent topic in regards to these concerns with current statistics and future
preventative measures being up to date, but without any literature combining it all [1]. The concern in
HAIs and implementing preventions also stems from the prohibitive cost incurred when such infections
delay treatment of patients. In the US alone, the cost is $9.8 million dollars annually [5]. Patients and
healthcare workers alike are both at risk, placing pressure on healthcare facilities to maintain a healthy staff
and avoid keeping patients longer than they should [4]. The frequency of HAIs are higher in developing
countries than developed countries. Additionally, developing countries are more likely to not be able to
meet the economic burden of HAIs the way first world countries do. Therefore, identifying risk factors and
preventative measures to reduce the frequency of HAIs is critical [1,5].
Four out of the sixteen articles analyzed in our review identified the department the patient was admitted to as a major risk, with the surgical ward ranking the highest. Infections at the surgical site seem to be most common [2,6,8,9]. Staff and patients not taking enough precautions to keep the site of incision clean was the root of such high incidence of infection, stemming from lack of education or supplies. Similarly, seven articles specifically stressed the importance of handwashing stations and educating practitioners on the importance of safe cleaning methods [2,11-13,17-19]. Along these lines, invasive medical devices proved to be a source of infection. Two articles identified urinary tract infections from urinary catheters to be a risk and two found central line catheters significant as well [2,6,18]. Knowledge of disease transmission proved to be low in Africa, which indicates that more educational programs need to be implemented.
Increased handwashing practices and educating staff about HAI pathology seemed to be beneficial in preventing HAIs, however more research regarding interventions needs to be conducted in developing countries. Two out of the five intervention articles that were analyzed were conducted in the US, which has a different budget, culture, and general knowledge about HAIs than developing countries such as those in Africa. Hand sanitizer is a tool used to eliminate microbes on one’s hands, but the economic burden to keep a steady supply is costly for African hospitals as demonstrated in a randomized trial by Wolfe 2016 [22]. Moreover, hand sanitizer may be an inefficient method in Egypt because the culture in Egyptian hospitals does not identify with the protocol and purpose of hand sanitizers [12]. A 2012 qualitative study found that hospital staff viewed the need to wash hands only if there were visible signs of filth.
More research regarding patient and staff safety against HAIs is pivotal in the future of African health care. There is a lack of new or creative interventions in Africa because three of the five total intervention articles focused largely on hand washing [17,19,21]. Enforcing hand hygiene is among the top interventions, but there is also a concerning disconnect between the practice of hand hygiene and the culture it is being implemented in. It seems two of the five interventions being studied are US based while studies identifying risk factors were overwhelmingly African based [18,21]. This is likely attributable to the funding US hospitals have to try new interventions versus the larger number of HAIs in African hospitals lacking the same funding [1,5,6]. That is not to say the interventions in the US would have the same effect with countries in Africa. Different cultures develop their own explanatory model regarding the same disease and will therefore treat diseases in different fashions that fit these models [23]. Future intervention studies should be based in Africa to evaluate how effective they are.
Conclusion
Public health safety is a pressing concern for healthcare providers and their support structures. Among
discourse, HAIs are a frequent topic in regards to these concerns. Current statistics beg for more preventative
measures to be adopted [7]. The concern in HAIs and implementing preventions also stems from the
prohibitive cost incurred when such infections delay treatment of patients. In the US alone, the annual
cost is close to 10 billion dollars per a study that analyzed 5 types of infections [5]. Patients and healthcare
workers alike are both at risk, placing pressure on healthcare facilities to maintain a healthy staff and avoid
keeping patients longer than they should [7]. The frequency of HAIs are higher in developing countries than
developed countries. Additionally, developing countries are more likely to not be able to meet the economic
burden of HAIs the way first world countries do. Therefore, identifying risk factors and preventative measures
to reduce the frequency of HAIs is critical [5,7].
Four out of the twelve articles analyzed in our review identified the department the patient was admitted to as a major risk, with the surgical ward ranking the highest. Infections at the surgical site seem to be most common. Staff and patients not taking enough precautions to keep the site of incision clean was the root of such high incidence of infection, stemming from lack of education or supplies. Similarly, all articles stressed the importance of handwashing stations and educating practitioners on the importance of safe cleaning methods. Knowledge of disease transmission proved to be low in Africa, which indicates that more educational programs need to be implemented.
Another risk factor identified was antibiotic use. Certain bacteria are more common than others in Africa. Certain antibiotics are ineffective against specific infections, which makes using the correct antibiotic paramount in preventing antimicrobial resistance. Healthcare practitioners need to thoroughly test the infection and identify causative agent, and treat accordingly. Incidences of antimicrobial resistance can be reduced or else HAIs will occur more often and be more challenging to treat.
Increased handwashing practices and educating staff about HAI pathology seemed to be beneficial in preventing HAIs, however more research regarding interventions needs to be conducted in developing countries. In a 2016 randomized trial regarding hand sanitizers to prevent the spread of Ebola, two out of the five intervention articles that were analyzed were conducted in the US, which has a different budget, culture, and general knowledge about HAIs than developing countries such as those in Africa. Hand sanitizer is a tool used to eliminate microbes on one’s hands, but the economic burden to keep a steady supply is costly for African hospitals [22]. Moreover, hand sanitizer may be an inefficient method in Egypt because the culture in Egyptian hospitals does not identify with the protocol and purpose of hand sanitizers. A 2012 qualitative study found that hospital staff viewed the need to wash hands only if there were visible signs of filth.
More research regarding patient and staff safety against HAIs is pivotal in the future of African health care. There is a lack of new or creative interventions in Africa. Enforcing hand hygiene is among the top interventions, but there is a concerning disconnect between the practice of hand hygiene and the culture it is being implemented in. It seems most interventions being studied are US based while studies identifying risk factors were overwhelmingly African based. This is likely attributable to the funding US hospitals have to try new interventions versus the larger number of HAIs in African hospitals lacking the same funding [5,6,7]. That is not to say the interventions in the US would have the same effect with countries in Africa. Different cultures develop their own explanatory model regarding the same disease and will therefore treat diseases in different fashions that fit these models [23]. Future intervention studies should be based in Africa to evaluate how effective they are.
Acknowledgement
The authors wish to thank Professor Molly Badrawy of the Wensberg Writing Center at Franklin Pierce
University for her editorial guidance in revision of this manuscript. Dr. Jabbour is supported by NH-INBRE
(Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the
National Institutes of Health (NIH) - grant number P20GM103506)
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!