Biography
Interests
Essohanam Tabana MOUZOU1*, Sarakawabalo ASSENOUWE1, Pikabalo TCHETIKE2, Eyram Yoan Makafui AMEKOUDI3 & Tchaa Hodabalo TOWOEZIM4
1Resuscitation Anesthesia Department at the Kara-CHU, Uttar Pradesh
2CHU-Sylvanus Olympio Anesthesia Resuscitation Department in Lomé, Togo
3Medical Resuscitation and Nephrology Service of the CHU-Kara, Togo
4CHU-Kara Traumatology Department, Togo
*Correspondence to: Dr. Essohanam Tabana MOUZOU, Department of Medicine and Medical Specialties (Anesthesia, Resuscitation and Emergencies), University of Kara, Togo.
Copyright © 2023 Dr. Essohanam Tabana MOUZOU, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction
Mortality is a demographic phenomenon of great concern in developing countries, especially in sub-Saharan
Africa. The interest in the analysis of this phenomenon takes into account the fact that, as a component of
the population dynamics, mortality also remains an indicator of the social development of a country. It
allows not only the evaluation of health programs but also the social, economic and natural environment that
give an idea of the living conditions of the population [1].
Death is a major event that constitutes an element whose evaluation and analysis are necessary in a resuscitation service [2].
In France, the mortality rate of patients admitted to the intensive care unit was 18% in 2007 [3]. In India, the mortality rate was estimated at 30.6% in 2005 [4].
In Africa, in Morocco, the ICU mortality rate was 33.4% in 2017 [5]; in Mali, 41.46% in 2006 [6]; in Togo 32.38% in 2014 [7].
In order to reduce mortality in the surgical intensive care unit since the arrival of the anesthesiologist, it was essential to conduct a study on mortality in the intensive care unit with the general objective of taking stock of mortality in the surgical intensive care unit of CHU-Kara.
Methodology
Our study took place in the surgical resuscitation department of the University Hospital of Kara (CHUKara),
a national reference center in the northern part of Togo.
The resuscitation department occupies the first floor of a multi-storey building. It is composed of a room
facing the operating room. It is occupied by eight (8) beds, equipped with two multiparametric monitors,
one of which is functional, a functional respirator, an electric syringe pump, a saturometer, emergency drugs
and a laryngoscope.
The medical care was ensured by: a resuscitating doctor in charge of the service; three paramedics including
a supervisor of the service; four nurses; four nurses on duty.
A team composed of a nurse, a paramedical anaesthetist and a nurse on duty ensured every day including
weekends and holidays.
Study Methods
This was a 12-month retrospective study from November 1, 2019 to October 31, 2020.
Patients who died in the surgical resuscitation department during the period from November 1, 2019 to October 31, 2020 were included.
All records of patients who died during the study period were included in the study.
Records of patients who died before admission to the ICU were excluded from the study.
We used medical records, therapeutic and monitoring charts, anesthesia records, operative report registers, and surgical resuscitation registers.
We collected data from medical records, anesthesia records, therapeutic charts, operative report registers, and the interrogation of the department supervisor.
The parameters studied were:
sociodemographic and epidemiologic aspects; date and time of admission;
time of admission; initial diagnosis; vital function status on admission:
(respiratory impairment; hemodynamic impairment; neurological impairment); pathological history; pathologies; treatment performed in surgical resuscitation; complications; causes of death; length of stay in resuscitation.
Data processing was done manually, and data entry was done using Excel 2016 software. Statistical analysis of the data was performed using EPI data 3.1 and Microsoft Excel 2016 software.
The quantitative variables were described in numbers and percentages; and were compared using the chisquare or Fisher tests, with a p-value of less than 0.05 as the threshold of significance.
For the realization of the study, a written request had received a favorable opinion of the director of the
CHU allowing the investigation on October 07, 2020.
Results
During the study period, 70 deaths were recorded out of 900 patients admitted, i.e. 7.8% deaths.
The mean age was 48.70 ± 20.65 with extremes of D2 and 80 years.
There were 49 (70%) male and 21 (30%) female deaths with a sex ratio of 2.33.
Emergency 52 cases (74.3%); surgery 15 cases (21.4%); gynecology and obstetrics 3 cases (4.3%).
The average admission time was 17.5 hours. 62 cases (88.6%) had a delay of less than 24 hours,
Initial pathologies:
Surgical pathologies 59 cases (84.3%); medical pathologies 5cas (7.1%);
Obstetrical pathology 3 cases (4%); not known 3 cases (4.3%).
Forty-eight (48) patients (68.6%) had urgent pathologies.
Medical pathology
Envenomation 2 cases; erysipelas of the leg 2 cases; metabolic disorder 1 case.
Surgical pathologies
Envenomation 2 cases; erysipelas of the leg 2 cases; metabolic disorder 1 case.
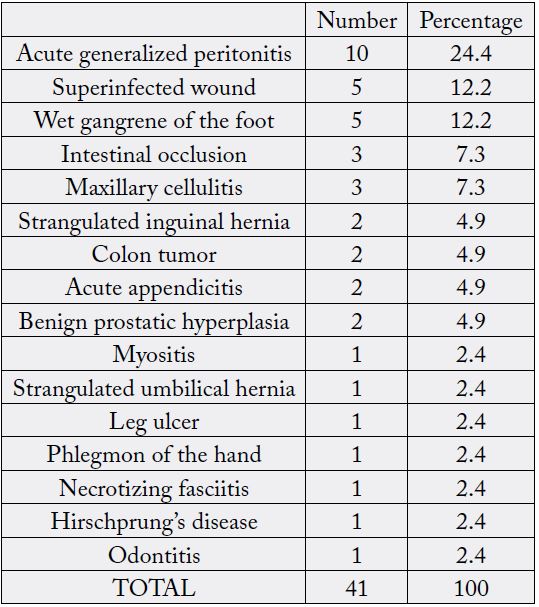
Forty-one (41) patients (69.5%) had non-traumatic pathologies and 18 (30.5%) had traumatic pathologies.
o Traumatic surgical pathologies
Cranioencephalic trauma 6 cases (33.3%); polytrauma 6 cases (33.3%)
Abdominal contusion 3 cases (16.7%); spinal cord compression 1 case (5.5%);
severe thermal burn 2 cases (11.1%).
Non-traumatic surgical pathologies
Obstetrical pathologies
Ectopic pregnancy 1 case; eclampsia 1 case; postabortal hematuria 1 case.
Severe coma 16 cases (22.9%); moderate coma 5 cases (7.1%): mild coma 6cas (8.6%);
Normal consciousness 37 cases (52.9%); Unknown 6 cases (8%).
Altered consciousness concerned 27 patients (38.6%).
Eighteen (18) patients (25.7%) had respiratory distress.
Fourteen (14) patients (20%) had hemodynamic shock.
HTA 8 cases (11.4%); diabetes 4 cases (5.7%); peptic ulcer 3 cases (4.3%);
asthma 1 case (1.4%); stroke 1 case (1.4%); HIV 1 case (1.4%).
One patient had one or more associated pathologies.
Treatments
Sixty-six (66) patients (94.3%) had medical treatment and 4 patients (5.7%) had medical treatment after
surgery.
Medical treatment without surgery
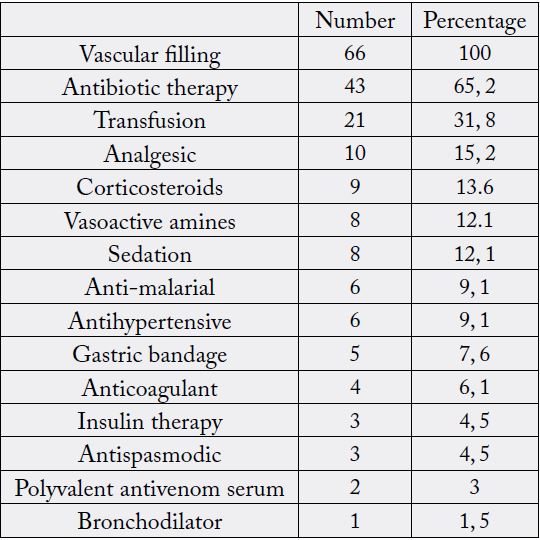
One patient had one or more treatments.
Vascular filling 4 cases (all); antibiotic therapy 4 cases (all); analgesic 4 cases (100%); hemostatic 3 cases
(75%); vasoactive amines 1 case (25%); sedation 1 case (25%); transfusion 1 case (25%).
One patient had one or more treatments.
Digestive surgery 2 cases; Neurosurgery 1 case; Maxillofacial surgery 1 case.
Oxygenation was done with a face mask in 25 patients (35.7%) and with a tracheal tube in 7 patients (10%).
Treated Evolution
Thirty (30) patients (42.9%) had complications.
Cardiocirculatory 24 cases (80%); infectious 15 cases (50%); respiratory 11 cases (36.7%); metabolic 6 cases (20%); neurological 3 cases (10%); renal 1 case (3.3%).
One patient had one or more complications.
02 to 08h: 13 cases (18.6%); 8 to 14h: 11 cases (15.7%); 14 to 20h: 20 cases (28.6%);
20 to 02h: 22 cases (31.4%); 4 cases (5.7%) not known.
- Risk factors for death.
Infectious 31 cases (44.3%); cardiovascular 24 cases (34.3%); respiratory 14 cases (20%)
Neurological 4 cases (5.7%); renal 3 cases (4.3%); metabolic 2 cases (2.9%); toxic, digestive and refusal of care 1 case each; not known 24 cases (34.3%)
One patient had one or more risk factors.
The average length of hospitalization was 4.6 days with extremes of 0 and 64 days.
Nearly 43 cases (61.4%) had a length of stay of 0 to 2 days.
Discussion
Our discussion focused on:
Sociodemographic and epidemiological aspects; Pathological aspects;
Initial diagnosis
Status of vital functions on admission
Pathological history
Pathologies
Treatments carried out in surgical resuscitation;
Evolution treated;
Complications
Causes of death
Length of stay in the intensive care unit.
Sociodemographic Aspects
Our study included 70 deaths (7.8%) during a 12-month period in the surgical intensive care unit of the
CHU-Kara. This death rate is largely due to traumatic pathologies and non-traumatic emergencies. This
low number would be related to less complex pathologies that surgeons were not yet used to. This period
corresponded to the new arrival of the intensive care anesthetist. This rate is almost identical to that of
Mbengono JAM, Bengono RB, Nkodo JM, Essame TC, Amengle AL, Minkande JZ [8] in Cameroon with
7.8%. Higher rates were found among Egbohou P, Mouzou T, Tomta K, Sama H, Assénouwè S [7] in Togo,
Sougane M. [6] in Mali and Koukous A. [9] in Morocco with respectively 32.38%, 41.46% and 25.8%. Our
rate is low compared to those of developing countries because of the high number of women who underwent
caesarean section with fewer deaths and less complex pathologies.
Our study included 70 deaths (7.8%) during a 12-month period in the surgical intensive care unit of the
CHU-Kara. This death rate is largely due to traumatic pathologies and non-traumatic emergencies. This
low number would be related to less complex pathologies that surgeons were not yet used to. This period
corresponded to the new arrival of the intensive care anesthetist. This rate is almost identical to that of
Mbengono JAM, Bengono RB, Nkodo JM, Essame TC, Amengle AL, Minkande JZ [8] in Cameroon with
7.8%. Higher rates were found among Egbohou P, Mouzou T, Tomta K, Sama H, Assénouwè S [7] in Togo,
Sougane M. [6] in Mali and Koukous A. [9] in Morocco with respectively 32.38%, 41.46% and 25.8%. Our
rate is low compared to those of developing countries because of the high number of women who underwent
caesarean section with fewer deaths and less complex pathologies.
The sex ratio was 2.33. The male predominance reflects the higher exposure to the risk of death probably
related to trauma because men would be more active in reckless driving of machinery and in occupations with traumatic potential such as motorcycle drivers for the most part. Our ratio is similar to that of Egbohou
P [7] with 2.2. Lamine N [13] in Mali found a lower sex ratio than ours, respectively 1.6 and 1.94. Zhu Z.
Shang X. Peiyi Qi1 and Shengli Ma [14] in China found a high value 3.23. In most studies, men are more
exposed to death.
Seventy-four point three percent (74.3%) of patients came from the emergency department. The emergency
department is a landmark of patient entry to the hospital. Our rate is higher than that of Moulay EK. [15]
in Morocco with 57.62%. But ours is lower than Lamine N and Maiga O [13, 16] with respectively 81% and
78.59%. The lack of emergency gestures in the emergency department are factors favoring a high mortality.
In our context, it was simply a reception and orientation service, nothing more.
The average admission time was 17.5 hours. It is thought to be related to referral difficulties and insufficient
financial means of the parents. The majority of patients who died (88.6%) were admitted within the first
24 hours. There were also a few hours between the emergency department and the intensive care unit for
the preparation of a medical record. The work of Al-Maimouni AY [10] in Morocco reported 53% of
admissions within the first 24 hours. The seriousness of the accidents and pathologies of the patients in our
context directed their admission in surgical resuscitation to less than 24 hours, especially since it was simply
a reception and orientation service. In our context, there was no EMS.
The longer the delay, the more the patients are exposed to the risk of aggravation and therefore morbidity and mortality.
Pathological Aspects
Deaths related to surgical pathologies were higher (84.3%). The surgical resuscitation unit of the CHUKara
was not a polyvalent resuscitation unit. It received mainly surgical pathologies.
Our rate was higher than that of Egbohou P [7] in Togo with 76.37%. The difference observed would be related to the performance of his study in the polyvalent surgical resuscitation.
Envenomation and leg erysipelas were the two dominant medical pathologies. Their complications led to
their management in surgery and thus in surgical resuscitation. Sougane M [6] and Maiga O [16] in Mali
and Konan KJ, Babo CJ, Ayé YD, Bouh K J, Kouamé YS, Soro L et al [17] in Côte d’Ivoire reported a
predominance of cerebrovascular accidents (CVA) with respectively 57.14%, 23.28% and 26.30% in the
multipurpose intensive care units. Stroke is a rare pathology in non-multipurpose surgical intensive care
units, yet its management is a public health problem.
Non-traumatic surgical pathologies dominated (69.5%) followed by traumatic pathologies (30.5%).
Infectious surgical pathologies dominated non-traumatic surgical pathologies and explained their high
rate. Moulay EK [15] in Morocco found a low percentage of both surgical pathologies with respectively
24.71% and 16.85%. Other authors reported a predominance of traumatic surgical pathologies such as Al-
Maimouni AY and Egbohou P. [10, 7] with respectively 14.9% and 31.22% of non-traumatic pathologies
then 29.6% and 45.15% of traumatic pathologies. For the latter, the high frequency of public road accidents
would explain this high rate of traumatic pathologies. Their etiologies should be investigated in order to
prevent them.
Traumatic pathologies were dominated by severe head trauma (TCE) and polytrauma (33.3% each). The
inadequacy of the technical platform and the seriousness of these pathologies associated with the delay of
first aid would explain their high mortality. According to Al-Maimouni [10], TCE accounted for 80%. In
our context, the rate is close to that of Egbohou P [7] with 34.18% for severe TCE.
TCE and polytrauma are serious pathologies and their high mortality rates constitute a public health problem in our context. Preventive measures should be associated to reduce their number, severity and mortality.
They were dominated by peritonitis (24.4%). Their mortality would be linked to the diagnostic and therapeutic
delay, to the insufficient financial resources of the parents and to the insufficiency of the technical platform
of the surgical resuscitation.
Our results are superior to those of Egbohou P [7] with 8% of generalized peritonitis.
It would be necessary to educate for health, to solicit the Togolese State to make universal health insurance effective for the entire population.
Altered consciousness was the most represented vital distress (38.6%). This is probably related to severe
CTE, polytrauma and generalized peritonitis with septic shock.
Our results are similar to those of Lamine N [13] with 38.77%.
Mbengono, Maiga O and Sougane M [8, 16, 6] had higher figures with respectively 51.3%, 54% and 76.96%.
Altered consciousness is a risk factor for mortality. The more it is associated with other pathologies, the more it increases mortality by its gravity.
Respiratory impairment (25.7%), this rate was almost similar to that of Egbohou P [7] in Togo with 21.9%. Like altered consciousness, respiratory damage increases mortality by hypoxia or tissue anoxia.
Hemodynamic shock (20%) in peritonitis and polytrauma was certainly a risk factor for mortality due to decreased perfusion and tissue oxygenation.
The majority of patients had hypertension (11.4%) followed by diabetes (5.7%). They were factors favoring
the risk of mortality by decompensation. Our results are lower than those of EL-Fassi A and Al-Maimouni
AY [18, 10] with respectively 33.7% and 19.9% for hypertension and 24% and 14.5% for diabetes.
The difference in these figures is due to the high frequency of these associated pathologies in these populations (pathologies of well-off people).
Reatments Received
Antibiotic therapy represented 65.2% of the treatment received due to the infectious surgical pathologies
in our context. Our result is superior to that of Moulay EK. [15] with 61.23%. Infection is a factor of
aggravation of mortality leading to severe sepsis.
Vascular filling for all surgical resuscitation patients was the rule.
Blood transfusion was performed in the case of hemorrhagic shock (31.8%) caused by polytrauma and peritonitis. This rate is lower than that of Moulay EK [15] with 48.87%. This low rate of transfusion was related to the unavailability of blood products which was also a risk factor for mortality in our context.
Oxygen therapy in the context of respiratory distress and hemorrhagic shock was done with a face mask (35.7%) and tracheal intubation (10%). This rate is lower than those of Al-Maimouni AY and Moulay EK [10, 15] with respectively 42.1% and 92.70%. Oxygenation had allowed the avoidance of hypoxia and anoxia which favored the reduction of morbidity and death.
Evolution
Complications accounted for 42.9%. They were dominated by cardiovascular complications, followed by
infectious and respiratory complications. Peritonitis and polytrauma would probably be at the origin of
cardiovascular complications, which are additional factors for the high mortality. On the contrary Al-
Maimouni AY and Moulay EK. [10, 15] found nosocomial infections predominant with respectively 10%
and 37.64%.
Complications accounted for 42.9%. They were dominated by cardiovascular complications, followed by infectious and respiratory complications. Peritonitis and polytrauma would probably be at the origin of cardiovascular complications, which are additional factors for the high mortality. On the contrary Al- Maimouni AY and Moulay EK. [10, 15] found nosocomial infections predominant with respectively 10% and 37.64%.
In our context, infectious complications would be related to peritonitis, polytrauma and even nosocomial infections. Respiratory complications were also important and related to peritonitis, polytrauma and severe TCE.
All these complications were the bed for the mortality of these patients. Preventive measures against infections in the intensive care unit should be associated.
There were more deaths between 8pm and 2am followed by 2pm and 8pm then 2am and 8am. There were
more deaths at times when paramedics were alone and especially at night (50%).
The absence of MARs during these hours explains in large part this higher mortality.
Also, the lack of staff on duty was an important factor in the number of deaths, with one nurse per 8 beds. This was similar to the conditions of Egbohou P and Moulay E.K [7, 15] with respectively 51.9% of deaths between 5pm and 7am and 48.31% between 9pm and 7am. This rate was lower in Takongmo S [19] with 58.6% of deaths between 17 hours and 7 hours. This is explained by the overload of the on-call team for night care administration. This increase in deaths began during the period 14:00-20:00 where the nurse was alone without the resuscitating physician.
In our context, infections were the main causes of death (44.3%) followed by cardiovascular causes (34.3%).
They were related to peritonitis and polytrauma. Our results were superior to those of Koukous A and
Moulay E.K [9, 15] with respectively 39.2% and 33.7% of infectious causes then 6.15% and 9.55% of
cardiovascular causes. The high value of these causes contributed to the high mortality rate. It is necessary to
take preventive measures against infections in intensive care.
The average length of hospitalization was 4.6 days with extremes of 0 and 64 days. The highest death rate
was between 0 and 2 days (61.4%). The inadequacy of the technical platform is a risk factor for mortality,
as well as the delay in diagnosis and treatment, the long delay in admission, the insufficient financial
resources of the patient’s relatives, and the complexity and severity of the pathologies were all factors that
contributed to early death after admission to the surgical intensive care unit. Our results were superior to
those of Sougane M [6] with 1.40 days and similar to those of MAIGA O and Ouédrago N [16, 20] with respectively 4.60 and 4.69 days. Our mean duration of hospitalization is lower than those of Koukous A and
Moulay E.K [9, 15] with 11.69 and 10 days respectively, as well as those of Rosenberg A and Rocker G [21,
22] with 11.8 and 9 days respectively. This difference is due to the difference in the patients recruited and
also to the speed of patient management and the availability and quality of the technical facilities.
Conclusion
This was a 12-month retrospective study of the records of patients who died during this period.
The mortality rate in surgical resuscitation was 7.8%.
Young people and young adults were more affected. The male gender was more represented. Most of the patients passed through the emergency department, which is a reception and referral service. The admission time was long due to the lack of a permanent emergency service. The initial pathologies were mostly surgical. The latter were non-traumatic, followed by traumatic pathologies (severe head trauma and polytramatic), all of which were associated with vital distress.
The patients before their death had benefited from medical and surgical treatment. The medical treatment had dominated the management. It was centered on the care of the resuscitation.
The evolution under treatment was marked by complications among which infections. The hours of death were in the afternoon and at night marked by the absence of MAR and the insufficiency of the paramedical staff.
The causes of death were dominated by infectious and cardiocirculatory causes from digestive pathologies (acute generalized peritonitis), polytrauma and severe head trauma. Other associated factors were the inadequacy of the technical platform, the delay in diagnosis and treatment, poverty, and the severity and complexity of the pathologies.
This high mortality rate requires advocacy for material and personnel resources to improve the quality of care and reduce the number of avoidable deaths; better organization of intensive care (several medical and paramedical teams with 8 hours of work per day for the paramedics); raising the population’s standard of living to reduce poverty and increase income for better health care and the introduction of universal health insurance, which is in the process of being implemented in the country; and the establishment of a SAMU (emergency medical service) and better organization of the emergency department.
Conflicts of Interest
None of the authors have any conflicts of interest.
Funding
We pay on our own funding.
Thanks
We would like to thank Isabelle Mouzou for her secretarial work and Afi Hégbor for the English translation.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!