Biography
Interests
Essohanam Tabana MOUZOU1*, Sarakawabalo ASSENOUWE1, Pikabalo TCHETIKE2, Eyram Yoan Makafui AMEKOUDI3 & Tchaa Hodabalo TOWOEZIM4
1Resuscitation Anesthesia Department at the Kara-CHU, Uttar Pradesh
2CHU-Sylvanus Olympio Anesthesia Resuscitation Department in Lomé, Togo
3Medical Resuscitation and Nephrology Service of the CHU-Kara, Togo
4CHU-Kara Traumatology Department, Togo
*Correspondence to: Dr. Essohanam Tabana MOUZOU, Department of Medicine and Medical Specialties (Anesthesia, Resuscitation and Emergencies), University of Kara, Togo.
Copyright © 2023 Dr. Essohanam Tabana MOUZOU, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Post-operative care in digestive surgery is care after surgery on the digestive tract and its annexes.
This surgery is burdened with morbidity and mortality. To have data on postoperative management
of this surgery and contribute to the reduction of morbidity and mortality, we initiated this study.
Evaluate postoperative management in digestive surgery at the CHU Sylvanus Olympio.
This was a prospective observational and descriptive study on postoperative care in digestive surgery
which took place from May 02 to August 03, 2019. The sociodemographic and clinical aspects,
peranaesthetics, postoperative care and patient evolution were studied.
220 patients of all ages operated for digestive surgery were concerned. Digestive surgery had occupied
the 3rd place of the surgical activities of the CHU SO. The male gender predominated (63.2%).
Surgical emergencies predominated (64.5%). General anesthesia predominated (71.4%). In 71.2%
of cases, anesthesia was performed by a single anesthetist paramedic. Postoperative analgesia was
not administered in the theater in 5.9% of patients.
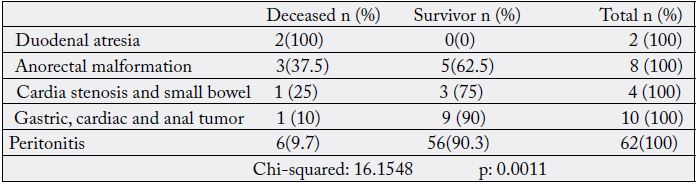
Postoperative treatment was poorly respected in 80.9% of operated patients. None of the operated patients benefited from a postoperative pain assessment. The analgesia schedule was not respected in 82.7%. The most monitored constants were temperature and BP (84.1%). The average postoperative hospital stay was 8.7 days. Malformative conditions were the most lethal: duodenal atresia (100%), anorectal malformations (37.5%).
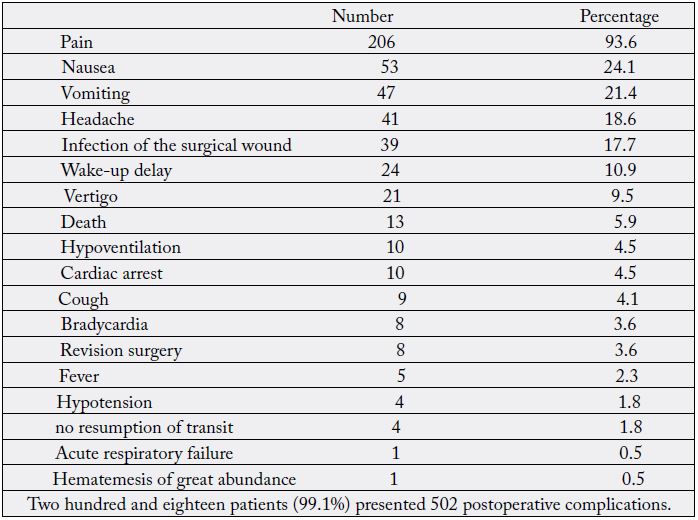
218 patients presented 502 postoperative complications, neurological (53.4%), digestive (22.5%), infectious (17.7%), anesthetic (10.9%), cardiovascular (4.4%), respiratory (4.1%) and 5.9% postoperative mortality.
Postoperative management was multifactorial and insufficient with several associated factors. It
was associated with very high morbidity and high mortality. To reduce morbidity and mortality,
it is important to have sufficient human and material resources and to organize ourselves in an
appropriate way.
Introduction
Digestive surgery is a surgical treatment of the organs of the digestive tract associating an attack on the body
that may be the cause of morbidity and mortality. To reduce this morbidity and mortality, it is necessary to
optimize postoperative care [1].
It is also important to have a complete description of the complications that will help all surgeons involved in new practices of surgical treatment of digestive diseases [2].
In order to provide data on the postoperative evolution of patients in digestive surgery and to contribute to the reduction of morbidity and mortality, we evaluated the postoperative management in digestive surgery at the CHU Sylvanus Olympio (SO) of Lomé.
Methodology
The study took place at the CHU SO in the postoperative care services for digestive surgery; the multipurpose
intensive care unit; the pediatric surgery department; the visceral surgery department A and the medicalsurgical
clinic (CMC).
This was a three-month observational and descriptive prospective study, from May 2 to August 3, 2019.
All patients who underwent digestive surgery under anesthesia were included.
Any patient who did not consent to the study or any patient operated on during the study period for digestive surgery who was discharged against medical advice was excluded.
In Practice
Patients were admitted after surgery to the post-intervention monitoring room (SSPI) or hospitalization or
resuscitation room for postoperative care until discharge.
After study authorization from the ethics and patient protection committee of the CHU SO, data collection was carried out from the interview of patients or accompanying persons, hospitalization registers, postoperative monitoring sheets, medical records, anesthesia sheets, registers of reports from surgeons and anesthesiologists, direct observation.
The information collected was: epidemiological, ASA classification, surgical indication, Altémeier classification, duration of intervention, type of operators, anesthesiologists, intraoperative complications, postoperative care, length of hospital stay, postoperative course.
The counting was manual. The chi-square test was used to compare qualitative variables. A value of p ≤ 0.05 was considered significant.
Results
During the study period, 235 patients were operated on for a digestive pathology in 2008 (11.7%) in the
CHU-SO. 220 patients (93.6%) were selected for the study.
The average age of patients was 35 ± 20.8 years with 18.2% under 15 and 2.7% over 75 years old.
Antibiotic therapy was done in 68.2% of cases and antibiotic prophylaxis 31.8% of cases.
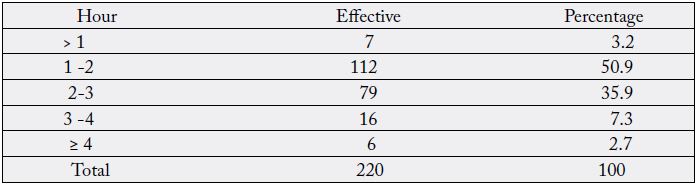
The average duration of the interventions was 1h52mn ± 49mn.
Table IV: Postoperative patient admission service
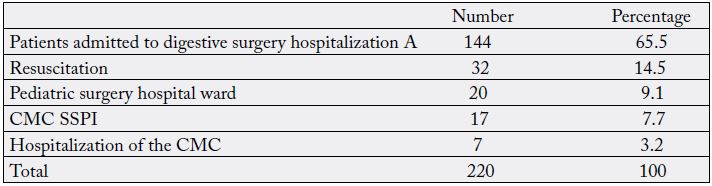
Among 7.3% intubated admitted to intensive care, 3.2% were not extubated before their death.
Abdominal drainage was performed in 19.1% of operated patients. 11.8% of operated patients had a bladder
catheter.
The nasogastric tube was placed perioperatively in 23.2% of operated patients.
The postoperative care protocol was established in 93.4% of operated patients and not established in 6.6%.
In 80.9% of operated patients, the daily treatment protocol was poorly respected
No operated patient benefited from a postoperative pain assessment.
The analgesia schedule was not respected in 82.7% of operated patients.
Postoperative analgesia was multimodal except in neonates.
Consciousness (12.3%); diuresis (11.8%); respiratory rate (11.4%); bleeding (5.9%); ECG (0.9%) were
poorly monitored.
Postoperative ventilatory assistance concerned 14.5% of patients with 2.7% mechanical ventilation.
24 patients had received labile blood products.
12.7% patients had received anticoagulant postoperatively.
Postoperative Evolution
All patients admitted to SSPI had spent less than 24 hours.
For patients admitted to intensive care, 34.7% had spent less than 24 hours, 51.0% between 24 and 72 hours and 14.3% more than 72 hours.
Resumption of transit: 1.8% not resumed before death.
Postoperative oral refeeding was not done in 2.7% of patients before their death
The state of the wound at the first dressing was: 2.3% suppurative
The dressing not carried out for 2.3% before their death.
The average length of hospitalization was 8.7 days with extremes of 1 and 79 days.
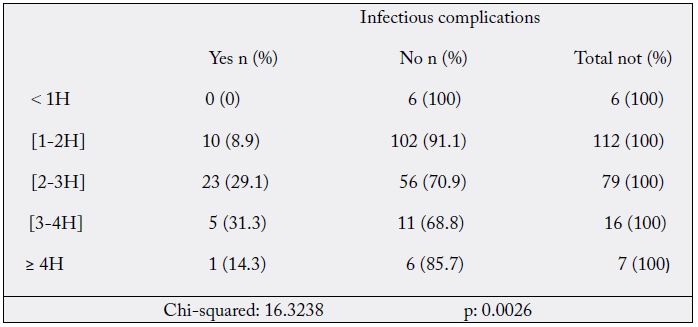
H: hour.
Discussion
We wanted to remain practical through this prospective study to discover and describe the reality on the
ground. The work takes into account a preoperative part and the intraoperative phase which can influence
postoperative care. This work concerns general surgeons, anesthesiologists as well as other doctors and
paramedics on the evolution of the surgical and anesthesiological management of digestive pathologies.
220 patients out of 235 cases of digestive surgery were included in the study (93.6%). The average age of
the patients was 35 years. The study involved all ages. The mean age was almost identical to the data in the
African literature according to Assouto and Ndayisaba [3, 4] (30 years; 31.5 years) but very low compared
to the data from developed countries. In our context, these were young patients, which could result in a
decrease in the number of able-bodied patients.
The male sex was predominant with 63.2% of the cases. This male predominance was reported by Solagbérou [5] with 69.1%, while Pimston [6] found a female predominance with 67.0%. Here again, the consequence could be the decrease of the valid arms.
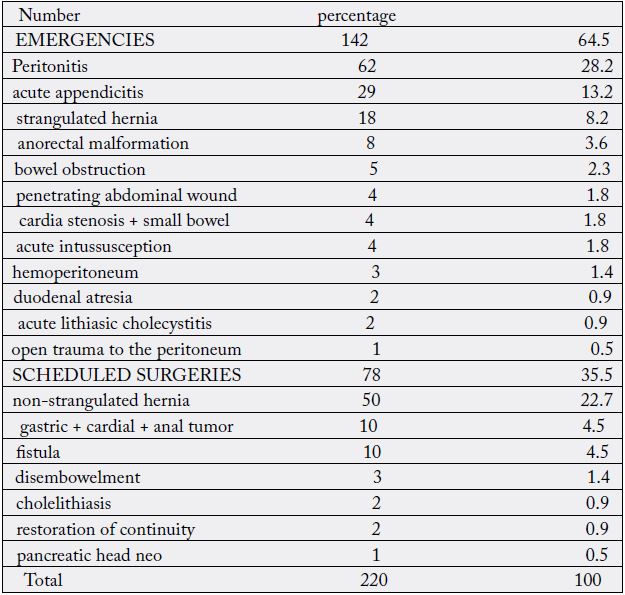
Acute peritonitis (28.2%) was the main indication for emergencies and non-strangulated hernia (22.7%) for
programs (table1). Emergencies predominated and peritonitis was the leading cause of abdominal surgical
emergencies. Several digestive surgical pathologies could be complicated by peritonitis in the absence of
adequate and early management. 64.5% of the patients were operated on as emergencies. The predominance
of emergencies was reported by Attipou [7] with 65.1%. Patients should be made aware of the advantages of
undergoing cold surgery and the risks in case of complicated disease. The context of digestive emergencies
is a real risk factor for intraoperative and especially postoperative complications. It is essential to prevent these risks by taking measures before, during and after the operation. It is these risk factors that the actors
of anesthesiology and digestive surgery management must master to optimize postoperative care.
ASA1 and 2 classes were predominantly represented (60.5% and 29.5%). The low rate of history would explain the predominance of ASA 1. The same observation was made by Scott [8]. ASA 1 patients should also be the object of particular attention, like the others, in the postoperative period, and care should be taken to resume the previous treatment of ASA 2 and more patients because of their associated pathologies. In our context, this majority of ASA 1 and 2 patients would constitute a lower risk factor for the occurrence of postoperative complications.
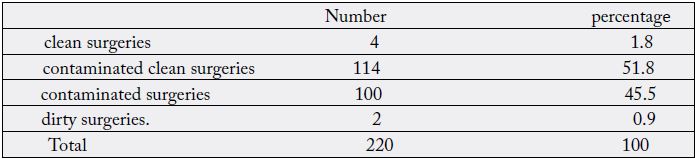
Clean contaminated surgery was 51.8% (table II) and antibiotic therapy was used in 68.2% of cases. The predominance of the use of antibiotic therapy here can be explained by the high prevalence of digestive emergencies, which were very often associated with an infectious syndrome, and the duration of the operations, which was also an infectious risk factor, as well as the state of asepsis in the operating theatres, and the septic behaviour of the intraoperative staff. This predominance was reported by Attipou [7] with 87.6% of antibiotic therapy. Because of the increased risk of intraoperative contamination, the actors should reinforce hygiene measures in the operating room (site, personnel and materials) and in the hospital wards.
Intraoperative Data
General anesthesia was used in 71.4% of cases. This predominance was reported by Eledjam [9] with 70%
of cases. It is a factor of hemodynamic imbalance which combines with that created by peritonitis to give
rise to intraoperative and postoperative complications. Anesthesiologists must control it and take preventive
measures against the occurrence of these complications.
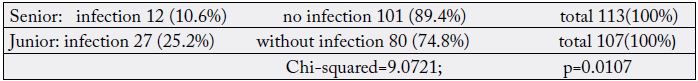
Surgical procedures were performed by senior surgeons in 51.4% of cases. The rate of infectious complications for junior surgeons was 25.2% (Table VI) and 10.6% for seniors. The senior surgeons had performed the majority of the surgical cases with the aim of transmitting knowledge, know-how and skills with a good application of the techniques, thus influencing the quality of the postoperative follow-up. This would explain the difference in the rates of infectious complications. According to Ki-zerbo [10], the risk of infection is high if the surgeon has less than two years experience. In our context this concept is applicable.
In 71.2% of the cases, anesthesia was performed by a single paramedic anesthetist and 135 complications occurred in 108 patients (49.1%), including 3.6% recovered cardiac arrests. Almost three quarters of the cases of anesthesia were conducted by a single paramedic. The terrain, the predominance of emergencies and the inadequacy of the anaesthetic staff were the factors favouring the occurrence of these complications. The insufficiency of the MARs for the supervision of anesthesia and the management of critical situations was an aggravating factor, approved by Arbous [11].
In our context, the inexistence or the great insufficiency of the MAR increases the anesthesiological insecurity in the surgical management of digestive pathologies which are already complex by their nature. The medicalization of anesthesiology in our context should be encouraged. 5.9% of the patients operated on did not receive postoperative analgesia in the operating room: by omission or negligence. According to Scherpereel [12], systematic analgesia is preferable to analgesia on demand. Prevention of postoperative pain was therefore necessary for all the patients. Here again, the presence of MAR is necessary.
Only the CMC SSPI was functional. Chobli [13], had well notified its importance in terms of patient
safety (table IV). It is the place where patients who should be admitted to hospital are monitored for
vital parameters and immediate postoperative pain management. This was lacking in our context and the
insecurity continued in the hospital ward, except for the patients admitted to the polyvalent intensive care
unit.
14.5% of the operated patients were admitted to the intensive care unit for postoperative monitoring of a major operation or for the prevention of a postoperative complication following an intraoperative complication (table IV). Of these 14.5%, 7.3% were admitted intubated to the ICU and 3.2% died without being extubated. This intubation arrangement was necessary at this stage to maintain vital functions. Some deaths occurred despite this. It is essential for the management of patients in digestive surgery to set up a resuscitation for heavy and complex surgeries.
Abdominal drainage was performed in 19.1% of the patients operated on, essentially 28.2% of peritonitis with effective surveillance in our context, it completes the intraoperative peritoneal lavage.
Bladder catheterization was performed in 11.8% of the patients operated on. According to Alves [14], bladder catheterization should not be systematic, which was the case in our context to avoid a urinary infection.
Nasogastric catheterization was performed in 23.2% of the patients operated on. The predominance of emergencies, including peritonitis, required the insertion of a nasogastric tube. It is variable according to Mariette and Gerald [15, 16] with respectively 11% and 95%. This probe reinforces the safety of the patient undergoing digestive surgery.
The postoperative care protocol was not established in 6.6% of the patients before they left the operating room. This was due to forgetfulness or fatigue related to the workload or laziness. Anesthesiologists are very often alone on call when faced with the management of several emergencies. It is important to reinforce this paramedical anesthesia staff.
In 80.9% of the patients operated on, the daily treatment protocol was poorly respected. There was only one nurse for 37 to 49 beds in the hospital wards, which limited surveillance and care to the strict minimum, and the schedule of care was not respected or was done at the request of patients. The number of nurses needs to be increased to ensure adequate postoperative follow-up.
None of the patients operated on had received a postoperative pain assessment and the analgesia schedule was not respected in 82.7% of cases. Postoperative pain assessment was not prescribed by the anaesthetists and the nurses in the hospital wards had not been trained to assess postoperative pain. Here it is essential to strengthen the capacity of paramedical anesthetists and nurses on pain assessment and management.
Non-compliance with the analgesia schedule mainly concerned patients admitted to the hospital ward, where analgesia was often administered at the patient’s request. It is important to strengthen the capacity of nurses.
Multimodal analgesia was respected except in neonates. The fear of overdosing still remains.
Thirty-three patients had received postoperative ventilatory assistance in the intensive care unit. The use of ventilatory assistance in the postoperative period was related to the terrain, the surgery, the anesthesia and above all the intraoperative complications. It is always important to have a resuscitation in the management of surgical digestive pathologies.
Hydroelectrolytic support was systematically provided to all patients operated on and 11% transfused.
The vascular sector was always highlighted by digestive loss and/or third sector.
12.7% of the patients had received postoperative anticoagulants to prevent high thromboembolic risk. These were patients transferred to the intensive care unit in whom early mobilization was not possible due to their clinical condition.
The most frequently monitored parameters were temperature and BP. The taking of these constants was limited to twice a day in the hospital wards. This was due to the lack of a monitoring chart and insufficient staffing. BP was not monitored in all patients because there was no suitable cuff for children. The monitoring of vital parameters in the operating room was very inadequate.
The patients admitted to the intensive care unit for monitoring or postoperative care remained there until
their clinical condition stabilized or, if necessary, until death, as was the case in our study.
All the operated patients had resumed digestive motricity in the form of gas or stool emission between Jo and D4. The majority of patients had resumed transit on the day of the operation or the following day. These were simple procedures. According to Mariette [15], the duration of postoperative ileus is normally less than or equal to four days. The recovery of gastrointestinal tract motility after surgery differs according to the segments: a few hours for the small intestine, 24-48 hours for the stomach and 96 hours for the colon. In our context, the resumption of transit allowed the resumption of oral feeding depending on the surgery of the stomach, the small intestine, the colon or the adnexal glands.
Almost half of the patients had resumed oral feeding postoperatively between D0 and D1. Oral feeding had followed the resumption of transit. Postoperative oral feeding was undertaken mostly between D0 and D1. Scott and Mariette [8, 15] found respectively 51.6% and 81% of oral feeding resumed between D0 and D1.
According to Mariette [15], early and progressive oral re-feeding from the day after the operation, provided that it is tolerated, would allow rapid postoperative rehabilitation.
The earlier the oral resumption, the more it would promote peristalsis and reduce the delay in intestinal transit.
At the first dressing, the majority of surgical wounds (94.1%) were clean, 4.9% dirty and 2.3% suppurated. Most dressings (75.5%) were done once every two days. The infectious process that very often accompanies digestive emergencies would explain the dirty and suppurated state of the wounds at the first dressing. In our context, the dressing was done with sterile material but several factors favored secondary superinfection, namely: the work environment; the financial difficulties of the patients to honor the prescriptions for the dressing; the unavailability of the personnel for the care.
218 patients presented 502 postoperative complications of a neurological, digestive, infectious, anesthetic, cardiovascular, and respiratory nature, with a perioperative mortality of 5.9% (Table V). The failure to respect the schedule of care, insufficient monitoring of patients, the patient’s condition, the anaesthesia, the surgery and the often septic environment of the hospitalization rooms could explain the occurrence of these complications. Assouto [3] found 158 patients who presented 163 complications. Bernard [17] found an overall complication rate of 51%. In our series, the main postoperative neurological complication was pain (93.6%) while Attipou [7] had 89.3%. According to Rhoel [18], pain is one of the factors of the postoperative discomfort, the level 1 analgesics are administered at a fixed time without waiting for the patient’s request and the loading dose must be administered in the operating room one hour before the end of the operation. This practice was little respected in our context. This requires capacity building of the actors.
The surgical site infection rate was 17.7%. The prevalence of emergencies, the state of the operating rooms and the conditions of hospitalization could explain this high rate of surgical site infection. Chadli and Pesseaux [19, 20] reported respectively 5.20% and 4.05% of surgical site infection rates. This significant difference was related to the working conditions with reduced asepsis, and it is important to reinforce the capacities of the actors.
Perioperative mortality was 5.9%. Insufficient surveillance would explain the cases of death in the hospital ward. This mortality rate was significantly higher than those reported by Mariette and Regenbogen [15, 21] with 2% and 0.1% respectively. Several factors could explain this difference: the pathology, the emergency, the terrain, the delay in care, the health system characterized by antiquated equipment, insufficient qualified personnel, limited health coverage and health insurance. The challenge for safe and good quality care must be met.
The digestive complications were nausea, vomiting, hematemesis and non-resumption of transit with 3.6% of resumption for postoperative peritonitis. Anastomotic disunion was the main cause of these postoperative peritonitis that required a revision. Chaldi, Pessaux and Proske [19, 20, 22] found respectively 1.6%, 2.2% and 3% of postoperative peritonitis. This difference could be related to the delay in diagnosis and treatment, the long admission time and the infection of the surgical environment.
The mean duration of the procedures was: 1h52mn ± 49mn (table III and IX). The rate of infectious complications tripled with the duration of the operation and increased from 8.9% to 31.3% respectively for operations of one to two hours and three to four hours. Infectious complications were high with increasing procedure duration and were significant. The prevalence of complex procedures would explain the long duration of the procedures. The risk of infection was greater the longer the operative time. According to Cruse [23], if the duration of the operation is longer than sixty minutes, the rate of infectious complications is significantly higher, and beyond two hours the risk of infection increases. It is necessary to ensure the hygiene of the working environment and to reinforce the intraoperative antibiotic therapy.
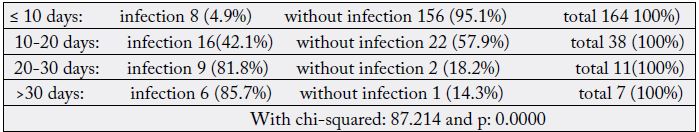
The average postoperative hospital stay was 8.7 days. The duration of postoperative hospitalization was related to the surgery, the terrain and the intra- and postoperative complications. This mean duration was lower than that found by Mehinto and Tchalla [24, 25] respectively 13 and 15 days. However, all these durations are much longer than that of Proske [22] with 4 days. Patients with less than 10, 20, 30 and more days of hospitalization had respectively 4.9%, 42.1%, 81.8% and 85.7% of infectious complications. Infectious complications were significantly correlated with the length of hospitalization (Table VII). A long stay increases the risk of postoperative infection by a hospital environment conducive to the grafting of an infection, by the circulation of germs therein and by the lifestyle that the patients led according to Touré [26]. They favored long hospital stays. This long hospitalization period favored the exhaustion of the parents’ resources, malnutrition, delayed healing and a vicious circle of infection.
Thirteen patients died (5.9%). The ASA3 class was the one for which mortality was highest, 9.1%, compared with 7.7% and 4.1% respectively in the ASA2 and 1 classes. The higher the ASA, the higher the mortality, but this correlation was not significant. On the other hand, according to Pignaton [27], the ASA physical status was a predictive factor of mortality. Mortality was rather related to complex and neonatal lesions. Catre [28] found a higher mortality in neonates with ASA greater than or equal to 3. It is important to evaluate ASA and to take preventive measures before, during and after surgery to reduce mortality.
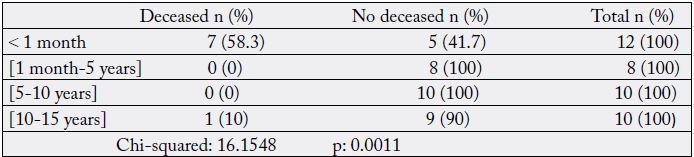
Malformative conditions were the most lethal: duodenal atresia, anorectal malformations. The mortality according to the operative indications was significant (Table VIII). There was the problem of early diagnosis of these malformations at birth and urgent measures to be implemented rapidly to avoid the occurrence of occlusive complications for duodenal atresia and anorectal malformations. This finding is similar to that of Livingstone [29] for whom congenital anomalies complicated by acquired septic conditions constitute a significant burden with high mortality in developing countries. According to the same author, the absence of neonatal resuscitation was another determining factor in the increase of neonatal mortality for malformative conditions. This was indeed the case in our context without a true neonatal resuscitation directed by an adapted specialist. The hospital and even the country need a real structure of this kind with proven competence.
Eight patients were recalled for postoperative peritonitis with three deaths. The mortality from postoperative peritonitis was very high. Yadav [30] had noted that postoperative sepsis was the main cause of mortality in emergency neonatal surgery.
Postoperative peritonitis, which is characteristic of digestive procedures, should make us think absolutely of setting up a resuscitation unit equipped with a sufficient number of resuscitators.
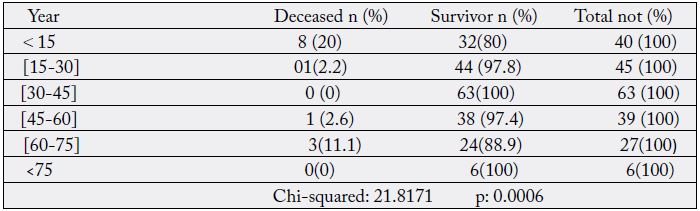
The delay in diagnosis, the financial difficulties of the patients to pay for the drugs and the insufficiency of qualified personnel were also factors that contributed to increase the mortality; as well as the emergencies and the very young age of the patients (newborns). GA drugs create postoperative cardiocirculatory and respiratory depression accentuated by surgical laparotomy incisions, explaining GA mortality. 20% of patients under 15 years of age and 11.1% of patients aged 60 to 75 years had died (TableX). Mortality by age was significant. Age was therefore an important factor in death in pediatric and elderly surgery. Neonatal surgery was particularly lethal (Table XI). The same was true for Pignaton [27] with children and adults. In the pediatric age groups, perioperative mortality is higher in neonates and infants than in others according to De Bruin [31]. Ademola [32] had made the same observation. The vulnerability of newborns is explained by the immaturity of most vital functions according to Chabernaud [33] and that of elderly subjects by the senescence of the organs. In our context, newborns and elderly people were fragile subjects. Great care and efficiency would be required in their management.
Conclusion
At the end of the study, the postoperative care in digestive surgery had made it possible to determine the
frequency of activity for 235 patients, 220 of whom were included in the study.
Postoperative care involved all ages with a predominance of males and young people.
Digestive emergencies predominated.
Dirty surgeries, contaminated surgeries and contaminated clean surgeries were predominant.
General anesthesia was predominant. It was performed almost entirely by paramedical anesthetists.
More than half of the surgery was performed by seniors and the rest by juniors.
There were few intraoperative complications.
Postoperative pain prevention was partially performed.
The postoperative care included mainly: filling, glucose intake, antibiotic therapy, postoperative analgesia, mechanical ventilation and simple oxygenation, monitoring of vital parameters, monitoring of the resumption of intestinal transit, paraclinical monitoring, postoperative pain, transfusion, monitoring of the abdominal wound, urinary catheters, nasogastric tubes and drains.
They were performed in the post-interventional surveillance room (SSPI), in the hospitalization room and in the intensive care unit.
There was an insufficiency in the postoperative care: the absence of evaluation of postoperative pain, the insufficiency of postoperative analgesia, the limited surveillance, the non-respect of the schedules of care in the hospitalization room, the insufficiency of the number of nurses, the unavailability of a pediatric blood pressure monitor and the none functioning of the SSPI.
What is Already Known about this Subject?
- Digestive emergencies are more frequent in the African environment
- The asepsis of the surgical environment is not well respected (favoring postoperative infection)
- Perioperative mortality is higher in settings with few management resources.
What this Study Adds:
- Insufficient technical facilities and human resources specialized in anesthesia.
- Insufficient paramedical nursing staff and their inability to administer appropriate postoperative care;
- Multidisciplinary postoperative care (surgeons, nurses, intensive care anesthetists, neonatologists, blood
bank, biology laboratory, medical imaging).
Thanks
To Isabelle Mouzou who did the secretarial work and Afi Hégbor who translated the text into English.
Ethical Approval
We have the agreement of the ethics committee of the CHU Sylvanus Olympio and the protection of
patients.
Duplicate Release
We have not undertaken any work to publish our study elsewhere.
Conformity
We have made every effort to follow all of your journal’s publishing procedures. We will submit to any
correction procedures to comply with the publication standard.
Conflict of Interest: The authors declare that they have no competing interests
Author Contributions and Agreement
They actively contributed to the study, data collection, analysis and writing of the manuscript.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!