Biography
Interests
Imtiyaz Ali Mir1*, Jia Qi Phang1 & Mohammed Abdulrazzaq Jabbar2
1Department of Physiotherapy, Faculty of Medicine and Health Sciences, Universiti Tunku Abdul Rahman, Jalan
Sungai Long, 43000 Kajang Selangor, Malaysia
2Department of Population Medicine, Faculty of Medicine and Health Sciences, Universiti Tunku Abdul Rahman, Jalan Sungai Long, 43000 Kajang Selangor, Malaysia
*Correspondence to: Dr. Imtiyaz Ali Mir, Department of Physiotherapy, Faculty of Medicine and Health Sciences, Universiti Tunku Abdul Rahman, Jalan Sungai Long, 43000 Kajang Selangor, Malaysia.
Copyright © 2022 Dr. Imtiyaz Ali Mir, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Sarcopenic obesity (SO) is characterized by age-related decline in muscle mass and function with
increased body fat, and is found to be associated with higher risk of physical disability, hospitalization,
metabolic syndrome, cardiovascular disorders and mortality. To date, no study has been carried out
on prevalence of SO in community-dwelling elderly in Malaysia. Objective of this study was to
determine the prevalence of sarcopenia and SO among community-dwelling elderly.
Using the convenient sampling technique, a total of 65 participants of either gender aged 60 years
and above were recruited for this study. Physical performance, muscle strength, and muscle mass and percent body fat were measured by usual gait speed, handgrip strength, and bioelectrical
impedance analysis respectively. European Working Group on Sarcopenia in Older People 2
diagnostic algorithm was used to determine the SO, based on the cutoff points from American
Society of Bariatric Physicians and Asian Working Group for Sarcopenia.
Out of 65 participants, 27 were males (41.5%) and 38 females (58.5%). The overall prevalence of
sarcopenia was 7.7% (n=5) and this was reported only in female (13.2%) participants, similarly SO
was only prevalent in female (5.3%), with overall prevalence of 3.1%. Age and gender were found
to be associated with sarcopenia (p=0.000; p=0.005 respectively), but SO was not associated with
gender (p=0.226) and age (p=0.814).
Prevalence of sarcopenia and SO is relatively low in Malaysian Chinese living in community. The
prevalence was only exhibited by female population. More studies shall be advocated as there is
dearth in current literature regarding SO in Asian population.
List of Abbreviations
SO - Sarcopenic obesity
EWGSOP2 - European Working Group on Sarcopenia in Older People 2
PBF - Percent body fat
HS - Handgrip strength
GS - Gait speed
ASM- Appendicular skeletal muscle mass
Background
Obesity is considered as a worldwide public health problem as more than one third of the world’s population
is expected to be affected by obesity [1]. The risk of being obese is increased by sarcopenia, which reduces the
physical activity, resulting in reduced energy expenditure [2]. Sarcopenia is known as age-related decrease
in skeletal muscle mass, as well as diminished muscle strength and/or physical performance [3,4] which
develops secondary to inflammation induced by visceral fat [5]. In 2018, European Working Group on
Sarcopenia in Older People 2 (EWGSOP2) used low muscle strength as the principal determinant of
sarcopenia, instead of low muscle mass [6]. The interaction between sarcopenia and obesity give rise to
sarcopenic obesity (SO). SO is a geriatric syndrome, described by reduced muscle mass and function, and
increase in body fat, with certain underlying elements [5,7].
Based on the 2016 population data, 10% of the Malaysians are 60 years old or above. With such a high percentage of elderly population, SO can adversely affect the health-related outcomes, such as risk of falls and fracture [8], can lead to reduced activities of daily living [9], and increase the risk of physical disability [10], eventually, decreasing the quality of life. Financially, SO may significantly increase the healthcare cost, including both hospitalization and cost of care during hospitalization. Hence, early detection of SO may be able prevent the worsening of health-related outcomes, thereby, reducing the risk of hospitalization.
Few studies have reported on the prevalence of SO in recent years [11-13], however, the majority of the studies undertaken in Malaysia have only focused on prevalence of either sarcopenia or obesity [14-16]. To our knowledge, there is no research evidence at all on the prevalence of SO among elderly in Malaysia, therefore, the objective of study was to determine the prevalence of SO among community-dwelling elderly.
Methods
Pilot study design with convenient sampling was employed. The sample size was calculated using the equation
developed by Viechtbauer et al. [17] with confidence interval of 95% and margin of error 5%. 65 participants
of both gender, aged 60 years and above were recruited. Participants who were wheelchair bound, with
metal implants, skin lesions around ankle and fingers that restrict the use of bioelectrical impedance analysis
electrodes, those with hearing impairment and not using hearing aid, visual impairment and not using
spectacles and fear of fall were excluded from the study. This study was approved (U/SERC/134/20) by the
scientific and ethical review committee (SERC) of Universiti Tunku Abdul Rahman and was carried out
according to the declaration of Helsinki, with all the recruited participants providing their written informed
consent.
All the outcome measures were assessed in the morning. Participants were clearly instructed to fast overnight and not to drink or eat anything during the morning time of assessment day and not to engage in any kind of physical activity [18,19]. This was to ensure that accurate measurement of the percent body fat (PBF) was taken during testing and to avoid any erroneous interpretation. Body weight and height were measured without shoes to the nearest 0.1kg and 0.01m respectively using SECA stadiometer and electronic weighing scale. To diagnose SO, body composition, handgrip strength (HS) and usual gait speed (GS) were evaluated. Bioelectrical impedance analysis device (Inbody S10 Body Composition Analyzer) was used to measure the muscle mass and PBF. Participants were positioned in seated posture and touch type electrodes were fixed on their four limbs. They were asked to rest their forearms on the arm rest of chair and keep their legs apart with feet flat on the floor. For electrode placements, hand electrodes were placed over the index (black) and middle (red) fingers for both hands, whereas foot electrodes were placed over the ankles (red for medial side; black for lateral side) for both feet. Once the analysis began, the participants were instructed to avoid any body movement and not to fall asleep throughout the process. Low muscle mass was height-adjusted appendicular skeletal muscle mass (ASM) of <7.00kg/m2 for male and <5.70kg/m2 for female [4]. The participants were identified as obese if PBF was ≥25% for male and ≥30% for female [20].
HS of the dominant hand was measured by Jamar® Hydraulic Hand Dynamometer. The participants were required to keep their arms rested on a supported surface. Standardized positioning recommended by the American Society of Hand Therapies was employed - participants were in sitting position with back supported, shoulders adducted, elbow flexed at 90°, forearm and wrist in neutral position [21]. The participants were required to grab the dynamometer forcefully for 3 seconds. The measurements were done for 3 times to get the average readings. 1-minute rest interval was given to prevent muscle fatigue. Low muscle strength was defined as HS of <26.00kg for male and <18.00kg for female.
For assessing physical performance, a 6-meter of level walkway with additional 2-meter of acceleration and 2-meter of deceleration phases was used. The participants were instructed to walk at their usual and comfortable pace. The timing was being started when the toes of leading foot crossed 2-meter mark, and stopped once 8-meter mark was crossed. Test was repeated for 3 times to obtain average readings. The participants were allowed to use assistive device, if any, during the gait test. Usual GS of >0.8m/s was considered as low.
All data was computed in excel sheet and statistical analyses was performed using IBM SPSS Statistics for Windows (Version 24.0). All statistical analysis was done in 95% of confidence interval (CI). The result was considered statistically significant if p < 0.05.
Results
Descriptive statistics was used to analyze the demographic data and measurement data, as well as prevalence
of sarcopenia and SO. Table 1 shows the demographic characteristics of participants.
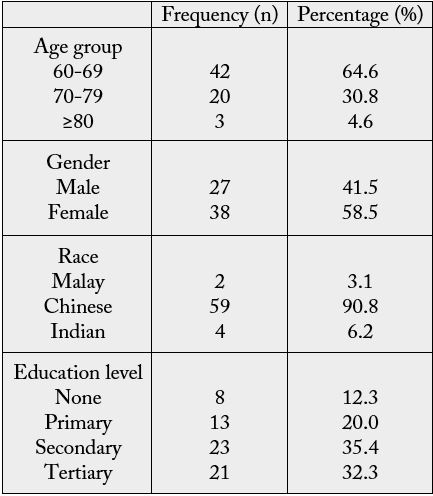
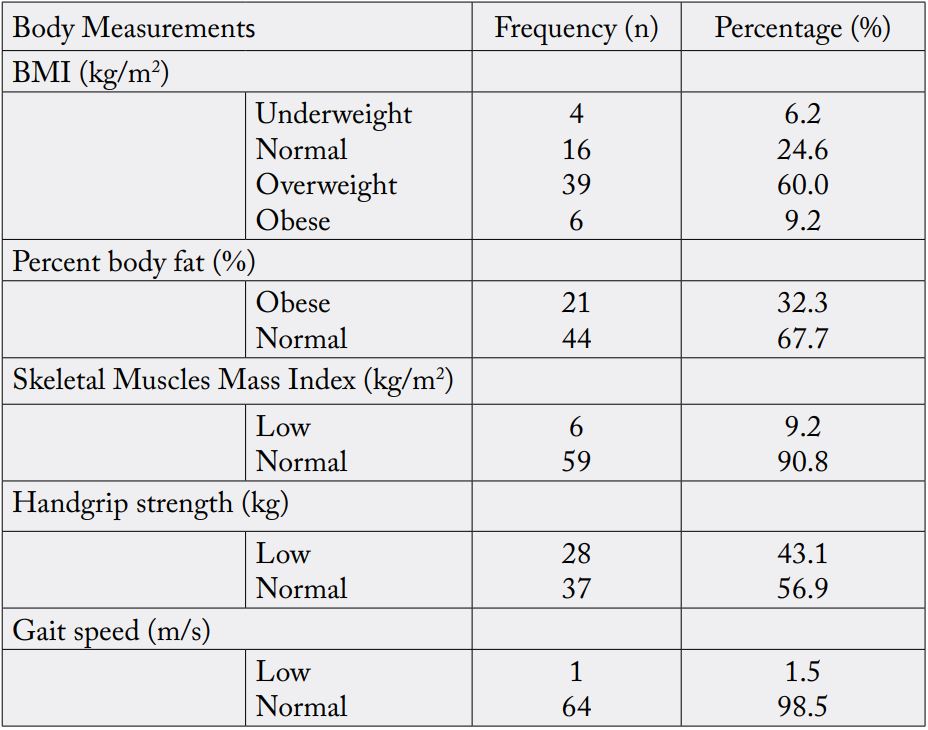
Out of 65 participants, 27 were males (41.5%) and 38 females (58.5%). The participants were categorized into 3 age groups, which were 60-69 (n=42, 64.6%), 70-79 (n=20, 30.8%) and ≥80 (n=3, 4.6%). Skeletal muscle mass index (SMI), HS and usual GS were used to diagnose presence of sarcopenia. Table 2 shows the measurement characteristics for diagnosing the SO. 6 participants were diagnosed with low muscle mass (9.2%), 28 participants were having low muscle strength (43.1%) and only one out of 65 participants was having low physical performance (1.5%) (table 2).
The overall prevalence of sarcopenia was 7.7% (n=5) and this was only reported in female (13.2%) gender. This prevalence was found in all age groups, which are 60-69 (n=1, 2.4%), 70-79 (n=2, 10.0%) and ≥80 (n=2, 66.7%). Age group was found to be associated with sarcopenia (p<0.000), but association was not found with gender (p=0.05) after performing Pearson’s chi-square test.
The overall prevalence of obesity was 32.3% (n=21). The prevalence of obesity was found mostly in female (n=20, 52.6%) with only one male (n=1, 3.7%) being obese. The prevalence was found in age groups of 60- 69 (n=14, 33.3%) and 70-79 (n=7, 35.0%). Gender was found to be associated with obesity (p<0.035), but association was not found with age groups (p=0.468) based on Pearson’s chi-square test, as indicated in table 3.
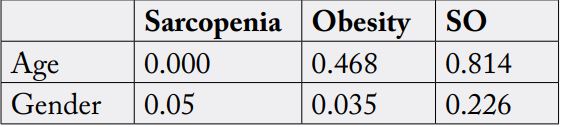
*Pearson’s Chi-square test was performed, Level of significant at p<0.05.
The overall prevalence of SO was 3.1% (n=2). The prevalence of SO was only shown by female (5.3%). Besides, the prevalence of SO was only observed in age groups of 60-69 (n=1, 2.4%) and 70-79 (n=1, 5.0%). Insignificant association of SO with genders (p=0.226) and age groups (p=0.814) was found after performing Pearson’s chi-square test.
Discussion
The study on prevalence of SO in Asian population is still lacking compared to number of studies being
conducted on sarcopenia and obesity alone. This indicates more studies in relation to SO should be conducted
in Asia and Asian population. This observational study demonstrated that community-dwelling elderly have
very low prevalence of sarcopenia and SO. Our findings were similar to study conducted by Kim et al. [22]
who reported the prevalence of SO was nearly zero for both gender, which was very close to the findings
in the current study. As compared to another study by Lim et al. [23], prevalence of SO was 16.7% in male
and 5.7% in female. The higher prevalence rate in their study was probably explainable by increased age of
participants (≥65 years) and use of muscle mass as the only outcome measure that did not meet the criteria
suggested by EWGSOP2, which could have resulted in overestimation of sarcopenia. For the current study,
the participants needed to meet at least two EWGSOP2 criteria to be diagnosed with sarcopenia. Besides,
they estimated the visceral fat in their study instead of body fat percentage, which possibly could have also
led to differences in the findings. Study by Cheng et al. [24] found the prevalence of SO of 4.7% and 1.4%
in male and female respectively, the recruited participants were physically active (at home or outdoors) and
free from chronic diseases. The current study also required the participants not to have any kind of chronic
disorders and most of them were physically active as well. The approximate similar findings may be due to
the characteristics of the participants assessed.
SO is classified as a geriatric syndrome, but whether it is gender specific or not is still questionable to researchers worldwide. Prevalence of SO was reported to be higher in men compared to women in Chinese population [24]. To the contrary, Kim et al. [22] reported SO was more prevalent in female , using weight adjusted ASM. For sarcopenia alone, Hao et al. [25] reported female had higher prevalence rate than male.
In the current study, the prevalence of SO and sarcopenia was only found in female participants. Generally, the gender differences on prevalence of SO and sarcopenia was insignificant, the differences in prevalence of SO (χ2 =1.466, p=0.226) and sarcopenia (χ2 =3.849, p=0.05) between gender was found to be statistically not significant. Therefore, sarcopenia and SO may be non-gender-specific disorder. Male and female could have equal risk of getting sarcopenia and SO. In terms of obesity, current study reported a profoundly higher prevalence in female compared to male. The differences in prevalence of obesity between gender was statistically significant (OR=0.035. 95%CI= 0.004-0.082). Similar finding was supported by another study, with higher prevalence of obesity in female (p<0.05) [26]. The possible explanation could be the greater fat deposition in female’s body due to sex steroids and genetic determinants. The sociocultural factors could have accounted for this phenomenon as well. In old age, male and female may have same dietary intake, but the physical activity level of female is comparatively lower to male, which makes them more prone to become obese [27].
Previous studies reported the eldest age group (≥80) has higher prevalence of SO [26,28], which was in contrast with current study as there was no prevalence found in this age group. However, prevalence of SO is supposed to increase with advancing age based on its pathophysiology. The difference in results could possibly be due to very low number [3] of participants from the oldest group due to higher mortality rate, as a result of the synergist effect of SO. Physical disability, as a consequence of SO could also be the reason as to why the number of participants above 80 were very few in our study.
EWGSOP2, International Working Group on Sarcopenia and specialists from Asia and America collaborate to form the International Sarcopenia Initiative. According to the report, the relationship of prevalence of sarcopenia and age could not be investigated systematically [29]. This could be due to the differences in manner used to report the participants’ age, such as mean age and age group in different reports. Majority of the studies demonstrated that prevalence of sarcopenia increases with age; this explains why sarcopenia is defined as age-related disorder. From the result of current study, the increase in prevalence of sarcopenia can be noticed from age group of 60-69 (2.4%) to 70-79 (10.0%) and finally ≥80 (66.7%). In addition, the difference in median age between participants with sarcopenia (77 years) and participants without sarcopenia (66 years) was statistically significant after performing Mann-Whitney test (p<0.05) indicating that advancing age can have higher risk of developing sarcopenia. In contrast, an inverse trend was shown between prevalence of obesity and advancing age. This statement was supported by several researchers, which reported a lower prevalence in age group of ≥80 compared to other age group [26,30,31]. In the current study, no prevalence of obesity was found in the eldest age group and the differences were statistically not significant (χ2=1.518, p=0.468).
We acknowledge that there were few limitations in this research study. First of all, the sample size in this study was too small. Consequently, the results generated in this study cannot be generalized to the public. Disproportionate distribution in ethnicity made this study unable to represent three races in Malaysia as most of the participants in the current study were Chinese. Lastly, the complete reliance on the cut-off values recommended by Asian Working Group for Sarcopenia and American Society of Bariatric Physicians may not represent the population in Malaysia completely.
Conclusions
In conclusion, prevalence of sarcopenia and SO was found to be very low among community-dwelling
elderly and this prevalence was only exhibited by female population. Additional research with larger sample
size and proportionate number of individuals from different ethnicity would be necessary to validate the
current findings. In completion of this research, noteworthy lack of relevant research evidence addressing
current knowledge of SO is noticed in Malaysia. Therefore, more studies should be advocated in different
aspects in order to enhance knowledge regarding SO.
Declarations
Written informed consent was obtained from all the participants to participate in this study. Ethical approval
(U/SERC/134/20) for this study was obtained from the Scientific and Ethical Review Committee (SERC)
of Universiti Tunku Abdul Rahman (UTAR), Sungai Long campus Malaysia, and complied with the
Declaration of Helsinki. All the participants were clearly informed with regards to their right to withdraw
from this study at any point of the time.
Not applicable.
IAM designed the study protocol, JQP and IAM implemented the protocol and
assessed the outcome measures, MAJ carried out the statistical analysis, and IAM, MAJ, and SH prepared
the manuscript. All the authors were involved in writing the paper and had final approval of the submitted
version.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!