Biography
Interests
Senay Cetinkaya1* & Esra Bulmus2
1Faculty of Health Sciences, Department of Nursing, Child Health and Nursing, Çukurova University, Adana,
Turkey
2Çukurova University, Health Sciences Institute, Nursing Care Main Branch of Science, Msc Student, Adana,
Turkey
*Correspondence to: Dr. Senay Cetinkaya, Faculty of Health Sciences, Department of Nursing, Child Health and Nursing, Çukurova University, Adana, Turkey.
Copyright © 2021 Dr. Senay Cetinkaya, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
According to the Occupational Health and Safety (OHS) Law, Nurses who take care of patients
with suspected COVID-19 and a definite diagnosis in a hospital environment, which is classified
as very dangerous, is extremely important not only for themselves but also for the patients they care
for, their families and society. The health care services provided by nurses who work in a healthy
and safe environment can affect the health and quality of life of people who receive this service.
Correspondingly, it is inevitable to increase the awareness of nurses on this issue by ensuring their
occupational health and safety. COVID-19 affects both the physical and psychological states of
healthcare professionals. Healthcare professionals continue to work, exposed to fear, stress, limited
resources, and infection. In these situations, managing mental health is as important as managing
physical health. A nurse who has been working in the COVID-19 intensive care unit since the
beginning of the pandemic and caught the disease; her experience during the illness process, psychological condition, and coping methods were written as a case report. Written and verbal
consent was obtained from the nurse in writing about her experiences during the illness process.
How did this nurse deal with the illness, was she able to cope in the long term?
Introduction
Healthcare professionals continue to work, exposed to fear, stress, limited resources, and infection. In these
situations, managing mental health is as important as managing physical health. Healthcare professionals
managing with COVID-19 experience physical fatigue, fear, emotional disturbances, and sleep deprivation
[1]. In a study conducted in China; there is 68.1% of nurse fatigue in Chinese nurses and this fatigue is
more common in women than in men and is highest in those who are married [2]. While some nurses are
more anxious because of the changing events and situations, some are more active and able to control the
situation [3].
I had a burning and itching in my throat, I graduated from university six years ago and began my career and
now I’m 28 years old. At the moment, I’m doing my master’s degree and worked in the COVID-19 intensive
care unit throughout the pandemic. Being aware of the fact that one of the main and most important
duties of the nursing profession is to provide service and benefit to society, I carefully took care of my
patients. While meticulously applying equipment such as full face masks and surgical aprons in the hospital
environment, I am caught by the virus because of my friend. My illness, which did not cause any symptoms
in the first week, became noticeable 7 days later as symptoms of cough, weakness, and vision problems. My
test result conducted on 22.11.2020 was positive. I was living with my mother and little brother at home. On
the same date, my mother also had the same symptoms. I had difficult times when I was trying to get over
this illness at home. The table below contains my information and data during my illness. We stayed in the
same room at home because my mother had the same symptoms and she refused to leave me. On the other
hand, my brother protected himself in his room and he did not get sick.
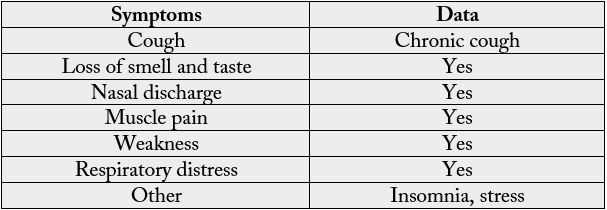
For treatment, I used 2 * 1600 milligrams of Favipiravir on the first day and 2 * 300 milligrams on the other days. Before favipiravir, I used 1 * 40 milligrams of Nexium to prevent nausea and vomiting and to protect my stomach. I took vitamins A, D, and iron and ate more tangerines than I have ever eaten in my life. My result was negative in the test I had done on 03.12.2020 and I started working on 05.12.2020 (Table 1).

The day before, I had a burning and itching in my throat, I waited for it to pass but it did not. When I woke
up in the morning I was sluggish and tired, and my eyes were also red. Assuming that this was due to my
long shift, I took my precaution and went to work. I wanted to go to work because the number of patients in
the intensive care unit, which was normally 10, became 14 during the pandemic process, and we were going
to work 4 nurses that day. When I went to work, my friends noticed immediately, they said “you are sick,
you should give a test immediately.” I told them; go, you will be too tired to take care of the patients.” But I
had to go and give my test, and I didn’t want to leave until the results came out. Both my patients and my
friends needed me. While I was preparing treatment I noticed that my eyes saw the patient’s vitals blurry.
Our meals came at noon. During the pandemic period, our meals arrived at the clinic in plastic containers
with our snacks. In case I infect my friends, I didn’t eat anything. I also hadn’t done breakfast in the morning.
Seeing that I was getting very sluggish at that moment, my co-workers sent me home. Since I believe that
the main treatment is always nutrition, I wanted to feed my patient and go, but I became too weak that I was
struggling to see. My co-worker fed my patient instead of me. While I was leaving, my mind was filled not
with being sick, but with my friends, who had to take care of 3 of the 14 patients in the clinic. Later, I came
home. I felt like I had let my friends down because we were working too hard and my permission would be
a burden to them. Anyway, one or both of us were getting this disease every day. I saw my mother at home
and she was tiredly lying just like me. My mother told me that she was weak and I replied to her the same
way by saying “me either.’’ I was scared. I was worried about my mother because she was over 50 years old. I
told her that we had COVİD-19. My mother persistently wanted to believe she had the flu. My friend called
from the hospital and I found out that my test was positive. I ordered Adana kebab from outside and ate it
together. Afterward, my mother and I had a long sleep until the morning.
When I woke up in the morning, I couldn’t move my head. My cough was so bad that it was like going to
destroy my lungs. My mother made us oregano tea. I noticed that it relaxed and stopped my cough. Looking
at the computer or phone was increasing my cough severely. In the evening, my mother made soup and we drank it. Four hours after dinner my fever had risen to 38.8. Because my mother was afraid when I started to
tremble, she put a cold cloth with vinegar on my head and neck areas. When my fever dropped, an hour and
a half had passed. While I should have looked after my mother as a healthcare worker, my mother’s effort
to look after me both made me emotional and feel sorry for my despair. In the evening, I called a friend
of mine who is a doctor and said to him “my cough does not stop and it is very tiring for me”. There was a
definition of asthma due to allergic rhinitis, and when I coughed, I said that I was taking Geraldine Plus and
before and I asked if there was any problem in taking it again. He told me not to drink anything other than
favipiravir and to consume plenty of water. I felt a little relief in my throat when I drank water.
We woke up in the morning with my mother. I was willing to sleep as if I hadn’t slept for a thousand years.
The filiation teams called and brought my medication. When I explained my mother’s situation, they told
her to go to the hospital. My mother went to the hospital by taxi but returned home without having a test
due to the queue and fatigue. I started the Favipravin drug. I wanted my mother to start but my mom didn’t
want to use it by saying she was fine. I drank 1 * 1600 milligrams of favipiravir in the evening. I fell asleep
after drank it. While I was sleeping, I woke up at night with a cough. My mother woke up because of my
voice. I said, “Mom, I can’t breathe.” My dyspnea has started. I was also afraid to upset my mother, but my
mother was like a shoulder I lean on. They couldn’t breathe like me. “How was I treating my patients?” I said.
I said, “Mom, I need steam.” My mother ran and immediately brought the teapot. I turned my face to the hot
steam of the teapot. I said to my mother “will you hit my back”. I was very bad at that moment, I experienced
the feeling of suffocation. I both lived and remembered my patients. I tried to do a coughing and breathing
exercise and lastly inhaled the steam in the prone position and kept coughing that way. It seemed like it was
never gonna pass. Then thyme tea came to my rescue again. Now I started drinking at least 3 cups of thyme
tea a day. I had never had thyme tea before I had COVID. I said from the bottom of my heart, “I’m glad that
I’m not alone at home” and I remembered once again that mother is a remedy for every problem.
I believed it would be good to take a shower in the morning. I went in and out of the shower. This is the first
time my hair fell out that much in my life when I was combing. I thought that cancer patients are faced with
this feeling and how bad it can feel to keep it happening all the time. My toothache started. Realizing that
I have been sick for 4 days, our cat came and looked at me. My brother was staying in a separate room from
us. I did not take the cat with me because I would have infected them. Sometimes my cat looked at me as
if she was puzzled and saying “this girl wasn’t like this, what happened to her?” People who have grown up
with loved animals can know this feeling better. My brother stayed away from us in his own room for days.
He is not infected. He also took care of the house’s grocery business. We were often airing the house. When
I was dealing with my cough, my mother made the soup again. My mother constantly does it with broth,
when I’m sick. The soup has always been good for us. Maybe this is why I tell patients, “Let them eat, it is
the strongest treatment”. I was relieved after the shower and meal, but my symptoms started again at night.
It reminded itself very well every now and then. It stuck to my throat at night, it was like someone came and
put glue on my throat. I was struggling to breathe. I wanted someone to aspirate me to get rid of the glue in my throat. I drank something hot again. My mother said, “be calm, you will be okay.” As I was dealing
with the disease in my bed, I was telling my mother, “If I start work, I will give patients something warm all
the time, I will do tapotement more often, and check their aspiration needs more often. I was already doing
these things, but when I experienced this, I started thinking about how to be more useful. Then again, steam,
thyme tea, tapotement, I somehow relaxed. My friends called on the phone.
It was difficult to talk. Each of them called and asked one by one. We were so afraid that something happened to one of us and we had to take care of her… I knew if I were bad; They would have taken care of me as best as they could as taking care of every patient until their feet hurt and I was going to be fine. Even if I was bad, I thought my colleagues would have kept me alive. All of these thoughts made me have affective disorders and reduced my ability to cope with stress. I fell asleep with my headache and these emotional thoughts.
I woke up with a cough again, I had enough energy to go to the kitchen and I opened the fridge. I saw that
my mother made yogurt, I said it was probiotic and I ate it immediately. What a cough it was that it didn’t
go away. There were eggs for breakfast. My mother said, “Eggs smell so good.” I brought the egg closer to
myself and said “it doesn’t smell at all”. I noticed my loss of taste and smell. I had breakfast and started the
day again with my thyme tea. While I was sleeping today, I felt a pain in my feet. The ache turned into bone
pain. My foot was too painful to make me sleep. I drank parol when the pain was unbearable. With the pain,
my leg started to make movements like in restless leg syndrome. I noticed something in the sink today. My
tongue had the strawberry tongue appearance seen in children, like a wound. I thought it was because of
fever and lack of vitamins and that’s why I immediately took vitamin D, A, iron supplements. My mother
gave me something with broth again. I was 28 years old, my mother was 55 years old. My mom’s faster than
me, his recovery surprised and delighted me. I have a mother who walks daily, exercises and eats healthily. I
gave the vitamins to my mother as well, she recovered even faster.
My night mixed with my day and my day with my night. I could not sleep at night, I could not wake up in
the morning. My report was lasting 10 days. I didn’t want to be sick again since I had too much debt, and
I was worried about the salary cut. Our neighbors gave us a drink called boiling prepared with a mixture of
seven kinds of spices and walnuts known as puerperal sherbet “kaynar”. It was hot and good too, but it tasted
bad to me. Now I could wake up to the day and feel alive, my belief that I was going to be healthy increased.
I knew how to cope when symptoms of COVİD occurred. My limb pains kept me awake all night, but it
wasn’t worse than not being able to breathe. I watched movies and listened to music to distract myself. I tried
to have fun with myself. I also looked at my photos from my old social days with my friends. I said to myself
“This process will end, it will pass.” I talked to myself about the way I support my patients, how I talk and
empathize with them. I managed to motivate myself.
I was fine now and enjoyed having coffee with my mother. What a joy it was… I was getting better. My
mother was fine, I was fine, my brother and cat were fine too. I had loved ones who were constantly seeking, asking, and wondering. There was a disease, yes, but there was life too. Breathing was worth everything. I was
trying to eat more food to gain energy. During this period, the responsible doctor who was worried about me,
my colleagues, my counselor who did not spare me my homework and humanity, and my graduate friends
were with me at times when I was mentally bad. I knew that it was worth loving, being loved, lovingly caring
for the sick, living strong, and keeping health alive for humanity. This job was worth everything...
Discussion
In this study, the physical emotional state of a nurse who became ill while working in the COVİD-19
intensive care unit (ICU) was presented as a case report. This study is presented to support individuals who
try to treat themselves at home in the COVİD-19 process.
My brother, who lived in the same house, did not get sick. By the way, I would like to express that physical distance is extremely important in order not to get sick. We have observed this by living with my brother who lives in the same house. The increasing number of patients, mutated virus, patients who had the disease, getting sick again, etc. Do not ignore the fact that we continue to pay attention to physical distance, the use of masks, and hygiene. If you have a chance to be vaccinated, of course, you should. I have to say this as a person who has had the disease. Unfortunately, we could not save a doctor in our hospital during the absence of vaccines. And again, unfortunately, there were patients that we lost a lot in this process and they continue to be. Sadly, some of our nurse colleagues who were vaccinated fell ill with COVİD-19. However, these friends at least overcome the illness process as a home treatment. In our society, the vaccination rate is not yet at the expected level, and the age of the patients who die is now in their 40s. In addition to developed countries that stock more vaccines for their own country’s citizens, underdeveloped and poor countries cannot access vaccines. In poor countries, people cannot access vaccines and personal protective equipment. Unfortunately, there are societies that do not have access to healthy and clean water and cannot provide personal hygiene comfortably.
The nurse in this case report is still not vaccinated. No information was given to her on this matter. One of the questions that individuals with the disease are curious about is when it will be their turn to vaccinate. In those with COVİD-19 disease; What complications will be seen or that can be seen in the near or distant time and how to treat them are also issues that need to be investigated.
Our nurse colleague who presented the case, said, “As a nurse, I was in fear, anxiety, and anxiety during the illness and while working in the hospital. “Everything started to look dirty to me, and I felt like I have to constantly wash my face shield,” she said. Ou., et al. (2020) found a significant relationship between obsessive-compulsive disorder and anxiety and depression states of nurses in their study with 92 nurses in China. In this study, these situations in nurses are lower than the national averages [4]. Of course, this can be explained by individual and social differences. Dönmez et al., In their presentations titled clinical characteristics and experience of a midwife with COVİD-19 in 2020, stated that the symptoms were mild [5], but in this case, respiratory distress and cough were observed. Like every nurse, the nurse in this case report also stated that she experienced midwife-like feelings of fear, anxiety.
Doğan et al. (2020) stated that the patient with COVİD-19 and nursing care case reports had joint pains. In this case, the nurse, who had similar pain conditions to the inpatient, stated that he used medication. Doğan et al. In his case report, it was stated that the nurse taught the cough and breathing exercises to the patient [6]. The nurse in the case report also tried to breathe comfortably with coughing and breathing exercises when she felt respiratory distress.
Yüncü et al. (2020) examined the impact of the pandemic on healthcare workers and found that it had psychological effects [7] In this case presentation, the nurse who had the disease stated that she also questioned her. Similar effects are observed in the case who stated that he could not cope with stress from time to time like the nurse in this situation analysis. Social support of family and relatives is extremely important in this disease process. An important question that comes to mind here is how individuals who live alone or who have to live alone are affected or will be affected in this process.
Nurses play a prominent role during the pandemic. Politicians and managers should practice solving the increasing problems of healthcare professionals [8]. Health workers should be supported both financially and morally in this process. In our country, the necessary steps in this regard should be taken as soon as possible.
Results
In this study, the experiences and observations of a nurse who had the disease were tried to be explained
objectively. The nurse said, “I hope that respiratory distress and cough can help individuals who try to
treat themselves at home in terms of coping with COVİD-19 because respiratory distress and cough were
the most severe and anxious conditions for me.” We wanted to indicate what a healthcare worker can
experience both physically and mentally after he/she becomes ill. All healthcare professionals must comply
with protective measures both inside and outside the hospital. It affects the emotional state of healthcare
professionals who witness the respiratory distress of their patients.
At the same time, we experienced a lot of losses as healthcare professionals in this process, and we continue to live. The most natural right of every human being is the right to life. During this pandemic process, we healthcare professionals have to continue both to live and to help people to survive by working hard in numbers. If the patient cases increase, even more, we do not want to deal with ethical problems such as the selection of patients for treatment and we do not want to bear the emotional burden of this.
Finding a vaccine is a good chance, but unfortunately, the desired result is not good in our society at the rate of vaccination. Unfortunately, it is not going well. The percentage of vaccines being made will of course increase in relation to the vaccine supply. Necessary things should be done in this regard. It is observed that death rates have decreased with measures such as closing shops, economic support, and immunization in developed countries. I hope our country will not be late in taking measures to reduce these mortality rates. Having a healthy and safe working environment for nurses who deal with patients with suspected COVID-19 and with a definite diagnosis in a hospital setting is extremely important not only for themselves, but also for the patients they care for, their families, and society.
Having a healthy and safe working environment for nurses who deal with patients with suspected COVID-19 and with a definite diagnosis in a hospital setting is extremely important not only for themselves, but also for the patients they care for, their families, and society. As a nurse, we have to “be hopeful” and continue “staying healthy” as we always say. In this way, we nurses realize that we can help other people to maintain their health. It is true that this pandemic is a trauma for everyone. However, healthcare professionals experience this every day. It should not be forgotten that healthcare professionals are also human beings.
Conflict of Interest Section
The authors have no conflicts of interest relevant to this article.
Funding Section
No financial or nonfinancial benefits have been received or will be received from any party related directly
or indirectly to the subject of this article.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!