Biography
Interests
Sara Rahama1, Mustafa Hussein2*, Salma Mohamed3 & Rayan Mohamed4
1Faculty of Medicine, University of Gezira, Wad Madani, Sudan
2Faculty of Medicine, University of Medical Sciences and Technology (UMST), Khartoum, Suda
3Department of Microbiology, Faculty of Medical Laboratory Sciences, University of Science and Technology, Omdurman, Sudan
4Faculty of Medicine, University of Science and Technology, Omdurman, Sudan
*Correspondence to: Dr. Mustafa Hussein, Faculty of Medicine, University of Medical Sciences and Technology (UMST), Khartoum, Sudan.
Copyright © 2021 Sara Rahama, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Coronavirus disease 2019 (COVID-19) has tested the readiness and preparedness of healthcare systems to respond to a global pandemic of such magnitude. Low and middle-income countries seem to be struggling more in meeting the high healthcare needs.
In this case-report from Sudan, we present an elderly lady who had been successfully treated and recovered from COVID-19 at home-level. She was managed at home due to the unavailability of hospital beds. However, various factors contributed to the favourable outcome.
Background
On March 11th 2020, the WHO declared coronavirus disease 2019 (COVID-19) a global pandemic. The
first case of the disease in Sudan had been reported on March 13th 2020 [1]. As of January 20th 2021, there
were 27,494 confirmed cases of the disease in the East African state with 1,657 fatalities [2].
In a country where significant challenges and gaps in the provision of healthcare services exist, facing the high tide of the global pandemic imposed a huge burden on both the community and healthcare system. This has been reflected in the insufficiency of personal protective equipment, shortage of healthcare professionals, preparation of isolation centres, disease surveillance and contact tracing. As a result, many healthcare facilities dropped out of service.
In this case report, we present an 87 years old lady who had been successfully treated and recovered in home isolation. The decision of managing her at home was based on the fact that there had been no available bed in the isolation centres in Khartoum state, where she resides.
Case Presentation
An 87 years old lady, with no background history of chronic medical disorder; complained of fever, diffuse
headaches and myalgia which were relieved by paracetamol. She is independent in carrying daily life activities
and manages her home duties perfectly without help. Three days later, she developed a dry cough, generalized
weakness and lethargy. Therefore, COVID-19 was suspected. Initial investigations were consistent with the
suspicion of COVID-19, as it showed white cell count (WCC) of 3.6 x 103/mm3, lymphopenia (lymphocytes
9%), mild thrombocytopenia (platelets 128 x 103/mm3), a mild degree of renal impairment (serum creatinine
1.4mg/dl) and c-reactive protein (CRP) of 96. She was started on Azithromycin 500mg daily for 3 days.
Besides, vitamin and mineral supplements to enhance her immune system. These supplements included
Vitamin C 1 gram twice daily, Vitamin D 3000 iu daily and Zinc Sulphate 200mg twice daily
The local health department was informed, and nasopharyngeal swabs were taken. The result of the swabs came back to confirm the diagnosis of COVID-19. Transferring her to an isolation centre was not possible, due to the shortage in beds in all isolation centres in Khartoum, capital state, where she lives. Hence, the decision was to manage her in-home isolation. All the household members abided by social distancing, wearing face masks and other health authority measures during the quarantine period. Besides, they were all swabbed and the results came back negative.
On day 7, she had an episode of diarrhoea and her appetite decreased significantly. On examination, her temperature was 39°C, pulse rate 65 beats per minute, respiratory rate 26 per minute and blood pressure 145/70. Chest auscultation revealed rales and crepitus bilaterally. Hence, she was started on salbutamol and ipratropium nebulization. In addition, intravenous antibiotics (Ceftriaxone 1 gram twicedaily and Metronidazole 500mg thrice daily) were commenced. Paracetamol infusion of 1 gram was scheduled every 6 hours and Clexane 40mg was started for venous thromboembolism (VTE) prophylaxis.
Two days later, when being assessed by the local health team, she was found to be irritated with severe bouts of dry cough and dyspnoea. Her blood pressure was 150/65, pulse rate 68 beats per minute, respiratory rate 32 per minute and oxygen saturation on room air was dropping to 87%. Besides, her temperature was 38.7°C. The local health department again decided to shift her to an isolation centre. Unfortunately, still, there were no available beds. Therefore, home management continued. She was commenced on oxygen therapy 5 litres per minute (L/m) via nasal cannula targeting oxygen saturation not less than 92%. Chest physiotherapy was done regularly. She felt more comfortable on her right side rather than on the prone position. Altered taste sensation was also noted.
Though the condition was seemingly improving, it had a sudden shift on day 15; she woke up with highgrade fever 38.8°C and was confused. Although her oxygen therapy was modified to 15L/m using a facemask, oxygen saturation was barely maintained above 90%. Meanwhile, she continued on salbutamol and ipratropium nebulization. One hour later, her status stabilized and her oxygen requirements by the end of the day settled on 8L/m matching saturation of 92%. Over the next few days, there was an obvious pattern of ups and downs associated with spikes of fever in the early morning and late at night. Besides, she had a continuous thirst sensation and sore throat.
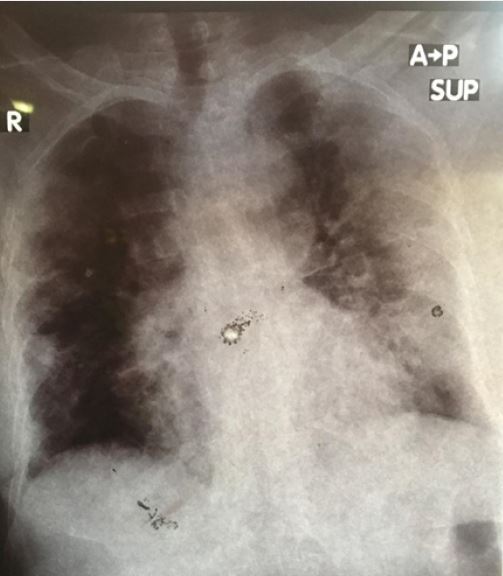
On day 18, a chest x-ray was done. It showed bilateral opacities mainly on the left side (Figure. 1). Also, her routine follow-up investigation revealed an increase in WCC10.5 with an apparent neutrophilia (9.4, 87.1%) and persistence of lymphopenia 8% serum creatinine 1.0 and urea 64mg/dl) together with increased inflammatory markers (CRP 96, ESR 87). On the light of her clinical assessment and lab results, antibiotics treatment was shifted to meropenem 500mg intravenous injection three times daily; along with the nebulization. Throughout this period, minerals and vitamins supplements were maintained.
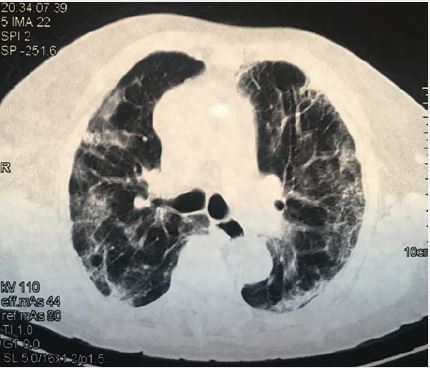
On day 23, her condition started to improve gradually. The fever subsided with normalization of the CRP and renal function tests. However, she was experiencing significant exertion dyspnoea, fatigue, and myalgias. She was started on dexamethasone injections 4mg daily based on the evidence provided by RECOVERY Collaborative Group [3]. Three days later, she showed overt progress with decreased oxygen demands despite the persistence of tachypnea. A CT Pulmonary Angiography (CTPA) was arranged and she was able to go for it without oxygen supplements. It showed no evidence of pulmonary embolism and described bilateral confluent ground-glass opacification with coarse reticulation which represented sequelae of COVID-19 infection. Moreover, early lung fibrotic changes were detected (Figure. 2). She was continued on dexamethasone injections for ten days.

On day 29 she was completely weaned-off oxygen. A second nasopharyngeal swab was taken the next day, and the result turned out to be negative.
One month later, she started ambulating using walking aids. She was feeling numbness in both of her legs with increasing forgetfulness; otherwise, her physical examination was unremarkable.
Discussion
Advanced age, presence of co-morbidities and immune-suppression have been associated with mortality among COVID-19 infected patients. There has also been a discrepancy in mortality rates based on the severity of infection and intensive care unit (ICU) admission [4]. It could also vary between patients managed at a hospital or home level.
Data on mortality from COVID-19 in Sudan varies widely. Salameh reports the fatality rate in Sudan to be 0.1121 [5] while Altayeb estimates it as 6.23% [1]. In a cross-sectional survey among hospitalized patients in Gadarif Hospital, East Sudan, mortality was found to be 37.5% with the majority of fatalities occurring within the first 24 hours of admission. It was also found to increase with advanced age [6]. However, upon reviewing the literature we found a paucity in the information stratifying mortality from COVID-19 in Sudan based on the location of management, whether it’s hospital-based or home isolation.
We believe that several factors played a role in the recovery of the patient presented here. These include the absence of co-morbidities, being not obese reflected by a body mass index (BMI) of 23.2, early initiation of pharmacological and non-pharmacological interventions and awareness of the household members who were taking care of her.
Bergquist et al. suggest that the clinical and socio-demographic characteristics between non-hospitalized and hospitalized patients infected with COVID-19 vary considerably. They noted that most of the symptoms among non-hospitalized patients resolved within one week. Besides, most of them (91.4%) lived with one or more household member [7].
A number of clinical trials are investigating the role of vitamins and minerals supplementation in the management of COVID-19 patients. It is thought that it has anti-antioxidant and anti-inflammatory effects. Although being used in higher doses than the recommended daily allowance, it is considered to be safe [8].
The psychological impact of the global pandemic continues to impose a negative effect on many patients. This can be as a result of confinement, loss of social contact and loneliness. The presence of family members providing social and emotional support can help in reducing psychological distress significantly. Hence, we believe this has been the case with our lady here.
Conclusion
This case report highlights the serious challenges faced by patients in Sudan seeking healthcare service
amidst the COVID-19 pandemic. However, management should not be delayed and started as soon as the diagnosis is suspected. It also sheds light on the importance of family members in providing support for
patients in home isolation.
Statement of Ethics
An informed consent has been obtained from the patient before writing the case report. The patient’s name
has not been mentioned and there are no identifiers to link the patient to the report.
Disclosure Statement
The authors have no conflicts of interest to declare
Author Contributions
SR conceived the idea, wrote the case presentation and discussion. MH wrote the introduction, discussion
and conclusion. SM and RM wrote the case presentation. All authors read and approved the final manuscript.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!