Biography
Interests
Güntuğ Batıhan
Department of Thoracic Surgey, University of Health Sciences Turkey, Dr Suat Seren Chest Diseases and Surgery Medical Practice and Research Center, Turkey
*Correspondence to: Dr. Güntuğ Batıhan, Department of Thoracic Surgey, University of Health Sciences Turkey, Dr Suat Seren Chest Diseases and Surgery Medical Practice and Research Center, Turkey.
Copyright © 2020 Dr. Güntuğ Batıhan. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Minimally invasive techniques in thoracic surgery have made great progress over the past 20 years and are still evolving. In this process, of course, different applications and methods have been described and the most successful and feasible technique has been tried to be presented. In this article, current minimally invasive techniques in thoracic surgery are discussed and important points are emphasized in the light of the current literature.
Introduction
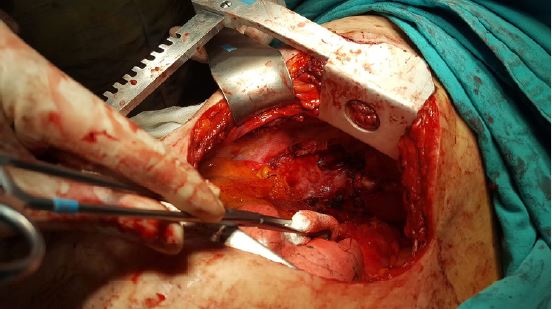
Minimally invasive surgical approaches have become widely used in thoracic surgery as they are applied
in every area of medicine. With the use of smaller incisions and modern instruments, patient comfort has
increased, and hospital stays have been shortened (Figure 1) [1-3].
Due to the rigid structure of the thorax, ventilation of the lung, and the presence of large vascular structures in the mediastinum, it has not been easy to adapt minimally invasive methods to thoracic surgery. While initially limited to simple biopsy procedures and wedge resections, nowadays, extended lung resections can be performed with minimally invasive surgery [3-5].
Advantages of thoracoscopic lobectomy compared to thoracotomy include less postoperative pain, better pulmonary function, early recovery, shorter hospitalization have shown by many studies, and Video-assisted thoracic surgery (VATS) has become established as a gold standard treatment method for patients with early‐stage lung cancer [2,3].
Surgical Technique
Although “tubeless” or “awake” VATS has been described and performed successfully by several authors,
single-lung ventilation, which may be accomplished with either double-lumen endobronchial tubes or with
single-lumen tubes and bronchial blockers, is often required for thoracoscopic lobectomy [6,7].
The patient is positioned in full lateral decubitus position with slight flexion of the table at the level of the mid-chest, which allows slight splaying of the ribs to improve exposure in the absence of rib spreading.
The instruments and surgical technique used vary according to the number, location, and width of the port incisions. Although the number of port incisions and locations are the surgeon’s preference, different applications and techniques have emerged over time.
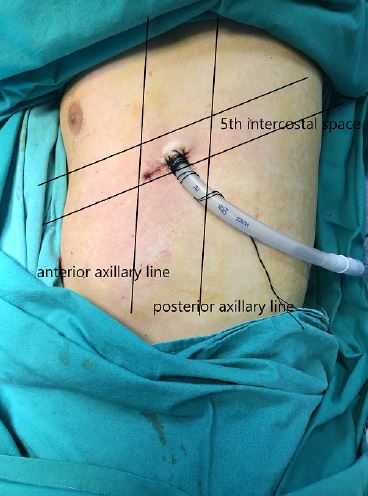
3-port VATS
In this technique, the camera port-anterior port is located in the 7th or 8th intercostal space in the anterior
axillary line, and the posterior port is located in the posterior axillary line in the same intercostal space. The
utility port was usually placed in the anterior axillary line 4th intercostal space for an upper lobectomy or 5th
intercostal space for a lower lobectomy (Figure 2). While the posterior port was previously placed from the
upper and rear levels, it was modified over time, and the localization we described became more frequently
applied [8].

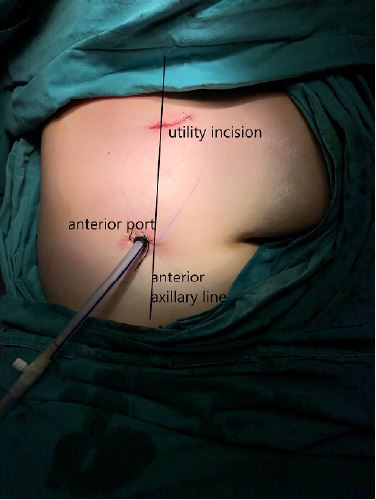
2-port VATS
Since the additional contribution of the posterior port is not essential, VATS has become applied with two
ports in some centers. The need for surgical retraction and manipulation can be provided by using another
instrument via the utility port (Figure 3). However, apart from providing retraction, another feature of the
posterior port that makes it useful is the introduction of the endoscopic stapling devices. Therefore, the
absence of the posterior port should be compensated by appropriate maneuver and retraction of the lung.
Uniportal VATS
Uniportal VATS is firstly described by Dr. Gaetano Rocco for minor thoracic procedures include lung
biopsies and pneumothorax operations [9]. Dr. Diego Gonzalez Rivas shared his single port VATS lobectomy
experience and became a pioneer in this regard [10,11]. It has become preferred by many surgeons due to its
advantages, such as causing less tissue damage and providing direct vision.
3-5cm uniport incision is placed in the 5th intercostal in the anterior axillary line. A 5mm diameter 30° video-thoracoscope is inserted through the same incision (Figure 4). Thus, the assistant and the surgeon share the same vision of direction. Although this is beneficial in terms of team cooperation, the working environment of the surgeon is somewhat limited.
Moreover, Gonzales Rivas successfully performed extended lung resections include bronchial, arterial, and double sleeve resections, and raised the bar in uniportal VATS lobectomy [12]. Despite favorable surgical results, whether uniportal VATS has an additional benefit over traditional VATS is still controversial.
Needlescopic VATS
The main goal of this technique is to reduce the size of the incisions rather than the number of ports. It was
aimed to minimize intercostal nerve damage and achieve better cosmetic results with the use of instruments
and ports with a diameter of 3-5mm instead of 10mm ones used in conventional VATS [13].
The placement of the ports and the direction of the vision are the same as the 3-port VATS technique, and the utility port has to remain at 3-5cm to extract the resection material. Surgeons who have appropriate instruments include 3 mm trocar, 3mm 30° video-thoracoscope, and needlescopic grasper and do not prefer the uniportal VATS may prefer this technique.
Robot-Assisted Thoracic Surgery
Advances in technology have enabled robots to be used in surgical procedures, and some authors started to
share their first experiences in robotic thoracic surgery in the early 2000s [14].
It is thought that robotic surgery, which provides 3-dimensional vision and has articulated modern instruments, may allow the surgeon a safer dissection. With increasing experience, many thoracic surgery procedures have been shown to be successfully performed with robotic surgery [15].
However, its use has not become widespread worldwide due to the system’s higher cost, the time-consuming installation, and the lack of tactile feedback during surgery. It is possible to achieve similar surgical results with much less expense without sacrificing minimal invasiveness.
Conclusions
Minimally invasive surgical methods are in a continuous cycle of change and development. Each technique
discussed in this article has its weaknesses and strengths, and surgical teams should choose the most
appropriate approach in line with their capabilities and experience. Robotic surgery may not be applicable
for every center due to its high cost, but even conventional instruments are sufficient to apply traditional
VATS with adequate effort and practice.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!