Biography
Interests
Envuladu, E. A.1*, Osagie, I. A.2 & Sodipo, O. Y.3
1Department of Community Medicine, College of Health Sciences, University of Jos, Nigeria
2Department of Community Medicine and Primary Healthcare, College of Medicine, Bingham University, Jos Campus, Nigeria
3Department of Community Medicine, Jos University Teaching Hospital, Nigeria
*Correspondence to: Dr. Envuladu, E. A., Department of Community Medicine, College of Health Sciences, University of Jos, Nigeria.
Copyright © 2020 Dr. Envuladu, E. A., et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Poor Infection prevention and control measures at health care facilities have been linked to puerperal and neonatal sepsis in Nigeria against the backdrop of socio-cultural factors. The aim of this study was to assess infection control equipment and practices in labour and delivery suites by healthcare workers at selected PHCs in Plateau State, Nigeria.
The study was a descriptive cross-sectional study conducted in Plateau State Nigeria. A cluster of 43 PHC facilities in the Jos Metropolis were included in the study. Questionnaires and a walk-through check list were used to collect data. Data was coded and analysed using SPSS version 23. Results were presented using the infection prevention and control domains as counts and percentages.
Hand washing amenities such as water were readily available in most of the facilities, but this was a challenge in about 20% of the facilities. Availability of complete personal protective equipment was low in majority of the facilities though disposable and surgical gloves being more readily available (100% and 97%). Only 6 of the 43 facilities (14%) had disposable bedding and disinfection of equipment was low across board: autoclave(44%), chemical (25%), boiler (30%). A little above half cleaned beds before and after delivery (58%).
The poor infection, prevention and control measures in PHC facilities revealed in this study could contribute to both puerperal and neonatal sepsis. The provision of effective equipment for disinfection and personal protective equipment as well as regular training and retraining of healthcare workers is recommended.
Introduction
One of the components of the 3rd United Nation Sustainable Developmental Goals is to reduce maternal
mortality to 75 per 100,000 globally [1]. However, in sub-Saharan Africa, there are still records of 830
women of reproductive age dying from pregnancy or childbirth-related complications everyday [2]. Nigeria
has a maternal mortality ratio of 512/100,000 live births making attainment of the SDG unlikely by 2030
[3]. Maternal mortality is associated with many factors one of which is puerperal sepsis.
Puerperal sepsis defined as: ‘Fever maintained over a twenty-four-hour period between the end of the first day to the end of the tenth day after childbirth or abortion’ is the third leading cause of maternal death [2,4]. When infections are not recognised and treated early, progress to sepsis may lead to morbidity or mortality for both mother and child, this has not received adequate research attention and accounts for at least 75,000 maternal deaths every year in Low and Middle-Income Countries(LMICs) [2]. Neonates birthed in health care facilities in LMICs are 3-20 times at a greater risk of contracting Healthcare Associated Infection (HAIs) compared to High Income Countries [5]. A neonatal mortality rate of 37 per 1000 live births in Nigeria is significantly high and puerperal sepsis has been implicated in up to 12% of maternal deaths [3].
Several reasons have been suggested for the increased risk for puerperal sepsis including the increasing age of mother, hospital overcrowding, early release of new mothers from wards, and rising rates of Caesarean sections [5]. In sub Saharan Africa, this has been closely linked to sociocultural factors (transportation, low socioeconomic status) and individual factors such as low immunity, malnutrition and anaemia). Albeit, health services factors have been linked to puerperal sepsis and include - poor birthing amenities/facilities, poor aseptic techniques and limitation in birth attendant skill against the backdrop of socio-cultural factors [5,6].
In Nigeria, 36% of deliveries occur within health care facilities and with an increasing drive in awareness and for the increase in facility delivery, it is essential that efforts are put into infection control at labour and delivery units to reduce the risk for HAIs [7]. Primary healthcare (PHC) facilities are the first level of care within communities with utilization in Nigeria ranging from 45-60% [8,9]. They are required to provide essential maternal and child health services including basic emergency obstetric care such as taking uncomplicated childbirths and assisted vaginal delivery. It also includes basic neonatal care and post-partum care [10]. However, there is paucity of data regarding infection control in the labour and delivery units in PHC facilities as a risk factor for neonatal and maternal morbidity or mortality.
This study was aimed at assessing infection control practices in labour and delivery suites by healthcare workers and to determine the availability and functionality of delivery equipment to maintain asepsis for women and neonates at selected PHCs in Plateau State, Nigeria.
Methods
The study was a descriptive cross-sectional study conducted between November 2019 and February 2020. It
was carried out in Plateau State, one of the 36 states of Nigeria, located in North Central geo-political zones.
The study location was Jos metropolis which is made up of Jos North and Jos South LGAs. Jos North LGA
has a total of thirty-three (33) PHC facilities, twenty-six (25) of which are public and eight (8) are private.
Jos South LGA has a total of forty-four (44) primary health care facilities, thirty-four (34) are public and
ten (10) are private.
A cluster of the PHCs offering labour and delivery services in Jos North and South LGAs were selected giving a total of 43 facilities. Data collection was carried out using a semi-structured pre-tested questionnaire, extraction of data from clinical records and using a walk-through check list. The questionnaire covered: Type of PHC facility, methods of infection control and the availability of equipment and amenities for infection control. It also collected information on infection control practices and procedures (such as: handwashing, availability of gloves, equipment and supplies, disinfection, autoclaving, drapes, gowns and shoe covers etc.) The walk-through checklist was used to collect information on labour and delivery units, environmental cleanliness and availability of necessary equipment for infection control.
Purpose of the study was explained to respondents and after reassurance of anonymity and confidentiality, information was collected by a team of trained resident doctors who do not work in the selected PHCs.
Data was coded and analysed using SPSS version 23. Results were presented in tables and figures and categorical variables using the infection prevention and control (IPC) domains were presented as counts and percentages.
Informed consent was gotten from all respondents prior to collection of data and confidentiality assured. Ethical clearance was given by the JUTH ethical review board while permission was given by the Plateau State Ministry of Health.
Results
The figures below shows the different domains of IPC which was assessed at the selected PHCs. These
include: Hand hygiene, availability and use of Personal Protective Equipment, Equipment for disinfection
practice, and the practice of disinfection.
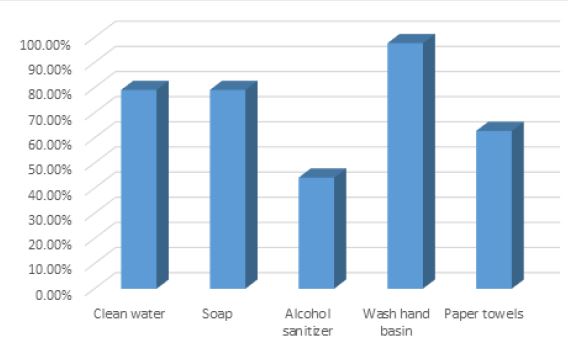
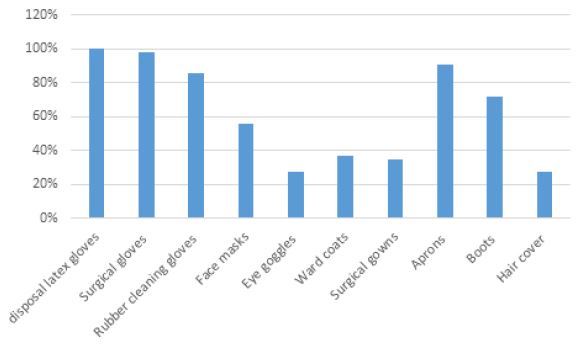
Water and soap as well as wash hand basins were available for hand washing in most of the facilities (79% and 97% respectively). However, this was less so for sanitizers (44%) and paper towels (62%). The availability of PPE varied depending on the types with disposable and surgical gloves being more readily available (100% and 97%) while hair covers, eye googles, ward coats and face masks were scarce.
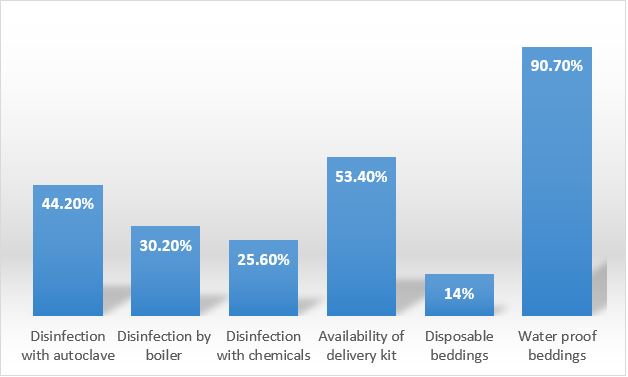
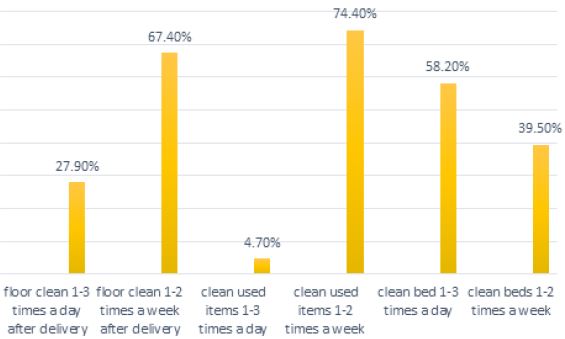
About half (53%) of the healthcare workers had delivery kits available for use during childbirth and waterproof beddings were readily available in nearly of the facilities (90%) compared to disposal bedding which was only observed in 6 facilities (14%). Disinfection of equipment varied depending on type - by autoclave(44%), chemical (25%), boiler (30%). In the domain of the practice of disinfection, the labour and delivery units were cleaned 1-2 times a week in two-thirds of facilities assessed (67%) and a little above half cleaned delivery beds before and after delivery (58%).
Discussion
An important aspect of infection disease control that is globally proven to be effective is hand washing. This
practice is encouraged especially in health facilities and in critical places like childbirth rooms. We must
also acknowledge that the practice of hand washing requires the availability of essential resources such as
clean running water and soap. Clean water and soap was available in majority of the delivery rooms but it
is not acceptable and right for about 20% of the health facilities receiving child birth to not have regular
water and soap and more than half without alcohol-based hand sanitizers in this period of COVID-19 and
considering the risk of puerperal sepsis, one of the leading causes of maternal mortality.
This situation is worse in other parts of the country as evidenced in a study conducted in Southern Nigeria; other studies in the country also reported availability of some and absence of other hand hygiene materials in the delivery rooms of health facilities [11-13]. This is not peculiar to Nigeria as finding from a study in India also reported non-availability of some hand hygiene equipment and commodities even though most of the maternity units had running water while barely half of the maternity units in Zanzibar met all the infrastructure conditions for hand washing in maternity units [14-16]. It raises the concern of a high risk of infection for both women and health care providers especially with the current outbreak of COVID-19, who in addition, are exposed to other existing nosocomial infections.
No delivery room should be without personal protective equipment (PPE) and incomplete PPE poses a risk to infection. What was observed in this study was that disposable gloves and surgical gloves were available in most of the delivery rooms, however, about half had no face masks and more than two thirds had no eye goggles, hair covers, ward coats and surgical gowns. India and Iran also had similar situation documented in studies conducted in their countries [12,15,17]. This implies poor infection control practice when faced with any potential high-risk patient.
Childbirth is associated with production of body fluid which can be highly infectious requiring consistent and effective disinfection. It is therefore, standard practice that materials and the entire delivery room be regularly disinfected [18-20]. It is unfortunate that most delivery rooms were not disinfected according to standard criteria and practice in this study. One will expect that all health facilities and sensitive units like the theatre and delivery rooms should have standard autoclaves but alternative disinfection methods such as boiling was not available and essential instrument like delivery kits were not available in some of the facilities. How do we then encourage hospital delivery and how does hospital delivery be perceived as better than home delivery if safety practices are absent in health facilities? In Bangalore, autoclave/hot air oven/boiling water and formalin were used for sterilization but not all health facilities had the equipment for sterilization [15].
The standard of cleanliness of the delivery rooms was also suboptimal, barely a quarter of the delivery rooms in the health facilities reported cleaning before and after childbirth and less than five percent clean the delivery rooms twice a day. With evidence that poor hygiene practices contribute to life threatening sepsis resulting in maternal and new-born mortality, the importance of hygiene and infection prevention control in health facilities cannot be over emphasized [18,20].
The study would have been more revealing if health workers were also interviewed and data captured on sepsis among women and newborns in the facilities. A much larger study about the IPC in the country involving microbiological components to assess the actual presence of pathogens and sepsis especially during the period the whole world is taking steps to fight COVID-19 is highly recommended.
Conclusion and Recommendation
This study revealed that IPC in primary health care facilities is low in the labour and delivery units.
Considering that PHCs are the first point of care for majority of Nigerians, this could be a major contributor
to both puerperal and neonatal sepsis thereby impacting on maternal and neonatal morbidity and mortality.
Further studies exploring health worker’s perspectives for factors responsible for the low IPC will be beneficial to inform policy makers. Albeit, the State Government and heads of the facilities have the responsibility to improve maternal and neonatal health services through the provision of effective equipment for disinfection, appropriate PPE and in organising regular training and retraining of healthcare workers within these units.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!