Biography
Interests
Seydou Bakayoko, Rodrigue Romuald Elien, G. Y.*, Mahamat Adam Dicko, Aly Sylla, Innocent Adubango Mananu & Tembely Marcel Lamine Traore
Hospital and University Center of the Institute of Tropical Ophthalmology of Africa (CHU-IOTA) of the University of Sciences, Techniques and Technologies of Bamako (USTTB), Bamako, Mali
*Correspondence to: Dr. Rodrigue Romuald Elien, G. Y., Hospital and University Center of the Institute of Tropical Ophthalmology of Africa (CHU-IOTA) of the University of Sciences, Techniques and Technologies of Bamako (USTTB), Bamako, Mali.
Copyright © 2020 Dr. Rodrigue Romuald Elien, G. Y., et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
To describe the clinical, therapeutic and evolutionary profiles of oculomotor paralysis during
diabetes at IOTA-Teaching Hospital.
We describe the case of a patient who was diagnosed with oculomotor paralysis.
Our patient is 80 years old, with type 2 diabetes antecedent for 10 years under hypoglycemic
sulfamides, poorly balanced, and uncomplicated, who presented 03 days before his admission of
headaches, left periorbital pain with progressive eye ptosis, After ophthalmological examination, neurological and orbital-computed tomography encephalopathy was diagnosed as a secondary
common oculomotor paralysis of diabetic neuropathy. The evolution after 3 months was marked by
the progressive regression of ptosis after glycemic balance.
Oculomotrice paralysis is common during diabetes, one should think about it before headaches
with unexplained visual disorders in any diabetic, Its evolution is favorable within a few weeks, but
enamelled with the possibility of homo or contralateral recurrence.
Introduction
Anatomically, the common oculomotor nerve at the entrance to the sphenoid cleft is divided into 02 branches
[1].
The upper branch will innervate the upper eyelid lift muscle and the upper rectus muscle [1,2].
The lower branch will innervate the medial rectus muscle, the inferior rectus muscle and the inferior oblique muscle [1,2].
These 02 branches constitute the extrinsic motor system of the common oculomotor nerve [1,2].
The pupil and the ciliary muscles receive the sympathetic fibres that constitute the intrinsic component of the common oculomotor nerve [3].
In diabetics, paralysis of the oculomotor common nerve involves either the upper or lower limb, or the entire extrinsic motor system [1-3].
Its prevalence in diabetics varies from 01 to 04% depending on the authors [4].
Observation
Our patient is 80 years old and male, he has been known type 2 diabetic for 10 years under oral antidiabetic
drugs, poorly balanced, and uncomplicated, who presented 03 days before his admission headache, left
periorbital pain, insomnia and rebellious to the usual analgesics (Paracetamol, Ibuprofen and Trialgic®)
with the fall of the upper eyelid of the left eye of progressive installation. In whom the ophthalmological
examination found:
- Distant visual acuity = 5/10 Snellen line
- External review a note:
• Drop of the upper eyelid of the right eye
• 3mm distance between the upper edge of the upper eyelid and the corneal reflex
• Function of the upper eyelid lift muscle was poor with 3mm stroke.
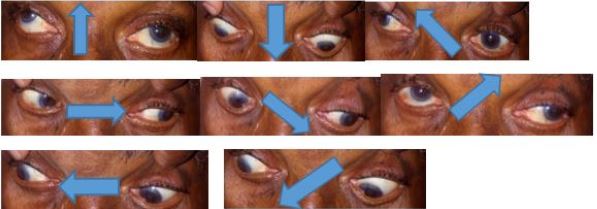
• Ophthalmoparesis of the upper gaze, in adduction, and slightly downward (Figure 1).
- The rest of the clinical examination was unremarkable.

- Distant visual acuity = 6/10 Snellen line
- The clinical examination was normal.
In front of this picture we concluded to extrinsic paralysis of the common oculomotor nerve.
The paraclinical check-ups carried out revealed: hyperglycemia with poorly controlled diabetes.
• Blood glucose = 193mg/dl (Normal = 70 - 110mg/dl)
• HbA1c = 10.4% (Normal < 7%)
• LDL = 1.5g/L (Normal = 1.10 -1.60g/L)
• Total cholesterol = 2.4g/L (Normal < 2.60g/L)
• Creatinine = 1.1mg/dl (Normal = 0.7 - 1.4mg/dl)
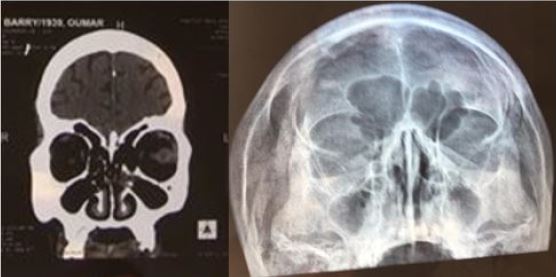
Orbitocerebral CT scan and Blondeau’s sinus incidence X-ray were unremarkable (Figure 2).
Therapeutic Protocol (antiplatelet agents)
- ASPEGIC® sachet 100mg (acetylsalicylic acid): 01 sachet per day for 02 weeks.
- CLOPI-DENK® tablet 75mg (Clopidogrel): 01 tablet per day for 01 months
The evolution was marked by the sedation of pain 48 hours after the start of anti-platelet agents; resolution of ptosis and ophthalmoparesis occurred 3 months later (Figure 3).
Discussion
The literature notes that isolated paralysis of the extrinsic motor system of the III is the prerogative of
poorly balanced diabetics [5,6] and often co-morbid with other degenerative complications [7]. Oculomotor
paralysis usually occurs after the age of 50 [7,8], as in our patient, but some authors have observed it in young
subjects [9]. No significant association between oculomotor paralysis and either the type of diabetes or the
sex of the patient has been reported in the literature [9]. Pupillary reactivity facilitates differential diagnosis
with aneurysmal compression III paralysis in which the photomotor reflex is abolished [3].
The normality of the lipid, renal, infectious, neurological, radiological and CT scans in our patient indicates that our patient’s common oculomotor paralysis was secondary to diabetic neuropathy.
The literature has highlighted the superiority of MRI over CT scans in the diagnosis of paralysis of the common oculomotor nerve, highlighting the different nuclei affected [10,11].
The first physiopathological description comes from Pierre M. DREYFUS who, in 1957, following the autopsy of a 62 year old deceased type 2 diabetic patient, evoked the hypothesis of a vascular mechanism, notably ischemic, by observing arteriosclerosis lesions of the vasa nervorum which led to partial ischemia of the common oculomotor nerve [12].
The regression of pain under anti-platelet aggregation in our patient confirms the ischemic origin of the paralysis of the common oculomotor nerve.
The therapeutic management of oculomotor paralysis requires good glycemic control, requiring the involvement of the endocrino-diabetologist, and the treatment of other risk factors for vascular ischemia such as arteriosclerosis, arterial hypertension, dyslipidemia, etc. [11].
Moreover, according to the literature, its evolution is spontaneously favourable after an average of 3 months [13]. But recurrences on But recurrences on the homo or contralateral eye are possible, without omitting the possibility of paralysis of the other cranial nerves. Hence the need for regular ophthalmological surveillance after any episode of oculomotor paralysis.
Conclusion
Oculomotor paralysis, like any other peripheral neuropathy, is a serious complication of diabetes.
The characteristics of pain during oculomotor paralysis have a negative impact on the diabetic’s quality of life.
Multidisciplinary cooperation is necessary for its proper management.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!