Biography
Interests
Dr. Carlo Lazzari
Centre for Healthcare and Medical Education, United Kingdom
*Correspondence to: Dr. Carlo Lazzari, 19 Castlemoat Place, Corporation Street, Taunton, TA1 4BB, United Kingdom.
Copyright © 2018 Dr. Carlo Lazzari. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Short Communication
Partnership in dementia care is becoming one of the primary goals of the actual healthcare system in the
United Kingdom. Besides, as multidisciplinary teams are constantly involved in the care plans, it becomes vital
to ensure that all people occupied in the care of patients with dementia (PwD) understand the requirements
for collaboration and care planning. The current study will also serve as policy paper to implement a patientcentred
approach to dementia care. Several constraints exist for a coordinated care planning and the sharing
of expertise and skills within interprofessional teams. The primary limitations are linked to the nature of
care of PwD which is complicated and long-term. Also, there are different interfaces of teams that might
have some difficulty in communicating data, plans, notes, as these teams are geographically unconnected,
have a different philosophy of patient care, operate in an asynchronous matter, and work according to silos
management strategies. For instance, the communication within wards when a patient with dementia is
transferred often sees delay in getting the notes about the new admission. The discharge letters from the
previous admissions might not be ready when a patient arrives at a new unit. The medication cards are not
always updated or communicated within interlocking teams. The original team might be late in generating
all the information needed in the new ward when the patient was already transferred. Chronic medical
conditions might be recorded in the family doctors notes but are not in the file accompanying a patient
during admissions. Occasionally, in order to facilitate the allocation of a patient to another destination, some
negative behavioural or clinical aspects are emphasized or omitted to increase the likelihood to appeal the new team. Interprofessional teams in the care of PwD involve many healthcare workers regulated by
specific professional bodies: nurses, doctors, clinical psychologists, occupational therapists, physiotherapists,
clinical managers, support workers, etc. Hence, due to the complexity of clinical cases of dementia and to
disparities in professional figures, collaboration, coordination, and mutual trust are not always automatic.
In fact, divided staff need specific training in order to grow and to operate in partnership in the care of
PwD. The first goal in partnership responds to the theory of social systems. Teams can avoid becoming
chaotic (hence impairing patient care) as long as the barriers within systems are permeable to exchanges
of information via interprofessional communication. This action will avoid the risk of that PwD remain
unattended in one of their basic needs because two systems (wards, teams, hospitals) did not communicate
some essential information in patient care (e.g., an allergy to medication). Another interprofessional barrier
to the partnership is the conflict within different professions. For instance, PwD might have a reduced
quality of care because a hospital manager does not accept that PwD’s agitation is treated with medication
as instead suggested by the medical team. Another barrier to a partnership is found when teams operate
asynchronously, during different times of the day, of the week or from different regions. For instance, PwD
might receive limited night sedation because the night team did not hand over to the day team about
increased confusion and agitation during night time and insomnia of ward patients. Another problem found
is that when patients are transferred from one geographical region to another, the whole team changes, and,
consequently, the care plans promoted in the former hospital or ward cannot be replicated in the new ward
or unit. In this case, the entire care plan needs to be regenerated. Another barrier to a partnership is found
in the models adopted by the professionals to describe and treat a symptom or presentation, and when the
interprofessional team cannot see coordination of the different care models. For instance, a consultant in
dementia believes that patient’s confusion should be treated ‘mainly’ pharmacologically while the clinical
psychologist believes that it should be treated ‘mainly’ with cognitive behavioural therapy. In this case, the
two professionals could have implemented a coordinated plan in the partnership where the patient is treated
pharmacologically ‘and’ with cognitive behavioural therapy. However, the divide has not been filled. In
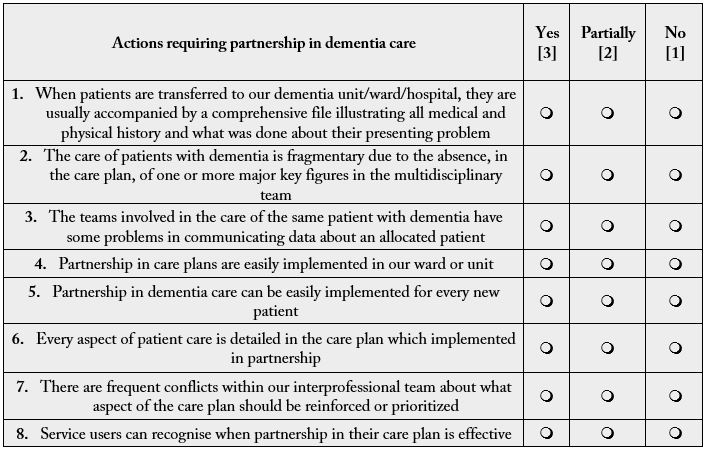
auditing partnership and coordination in PwD care the author of the current article has created a checklist
for assessing interprofessional care plans, the Partnership in Dementia Care Scale (PDCS). In the scale,
answers indicate that the patient has or not a robust care plan and that partnership in care is implemented.
There are several advantages of partnership in dementia care [1]:
1. ‘Added value’ as the global care plan cannot be accomplished if healthcare professionals work as separate entities.
2. ‘Reciprocity’ as the cooperation benefits each member of the multidisciplinary team.
3. ‘Formal and ongoing relationship’, a partnership is progressively achieved by working together.
4. ‘People who use services’, a partnership is effective only if it is recognized by the service users.
5. ‘Partnership is voluntary’ based on confidence, fairness and acknowledgement of the alliance.
Moreover, a patient centred care is achievable by sharing accountability and leadership within the interprofessional team [2]. Besides, being able to ask for help and to provide support to other members of the interprofessional team is one of the strategies of active collaboration [3].
Partnership in dementia care and interprofessional teamwork covers all areas of PwD treatment [4]:
1. Conclusive diagnosis is reached by consensus of different team members of what is the underpinning
problem.
2. Conclusive treatment requires coordination of each member of the team to assess the effect, side effects, and
allergies to the treatment provided.
3. Conclusive placement requires coordination of home treatment teams, families, care coordinator, support
workers, commissioners, and hospital team that agree what the best regarding therapy and placement for a
patient.
4. End of life care requires knowledge of hospital assets, wishes of the family, limitations linked to patient’s
physical health, and the legal aspects of DoLS (Deprivation of Liberty Safeguarding) and DNR (Do Not
Resuscitate).
The current project respects the guidelines for policy papers in the following dimensions [5]:
1. ‘Effectiveness’. The proposed paper examines the major steps in promoting partnership in dementia
care as matured during practical observations and auditing of dementia wards operating according to
multidisciplinary models.
2. ‘Efficiency’. The social impact is significant as it includes the whole care of a person with dementia.
3. ‘Equity’. The aim is to reduce the social divide in the health provision and provide PwD with the best care
plans operated by multidisciplinary teams.
4. ‘Feasibility’. Partnership in dementia care is already implemented in some regions and frequently applied
in the wards and community treating patients with dementia.
5. ‘Flexibility’. Care plans implemented by a partnership in dementia care should be open to the expertise
and creativity of each member of the multidisciplinary team.
In conclusion, the present article also stands as a policy paper for the management of patients with dementia in terms of desired actions in partnership care and eexpected goals in quality of patient-centred care.
Conflict of Interest
The author of the current article expresses no conflict of interests in the disclosed contents.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!