Biography
Interests
Dr. Manoela Vilarinho1*, Dr. Emília Martinez2, Dr. Hélio Nichioka3 & Dr. Thomas Pesavento3
1Physiotherapist, B. S. in Physical Therapy, Faculdades Metropolitanas Unidas, São Paulo, Brazil
2Physiotherapist, M. Sc in Health Science, Faculdade de Ciências Médicas da Santa Casa de São Paulo, São Paulo, Brazil
3Physiotherapist, Center at Oswaldo Cruz Hospital, São Paulo, Brazil
4Physiotherapist, M. Sc in Evidence-Based Health, Obesity Center at Oswaldo Cruz Hospital, São Paulo, Brazil
*Correspondence to: Dr. Manoela Vilarinho, Physiotherapist, B. S. in Physical Therapy, Faculdades Metropolitanas Unidas, São Paulo, Brazil.
Copyright © 2018 Dr. Manoela Vilarinho, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
To identify injury risks, biomechanical demands and develop a prevention program for climbers.
An electronic literature search was performed using Pubmed, Embase, Lilacs, The Cochrane
Library, PEDro for the development of this narrative. The outcomes analyzed were muscle strength,
mobility, range of motion, injuries and physical performance in climbers.
No studies on climber’s prevention treatment were found in the search. The literature provides
studies of other sports modalities that developed therapeutic exercises as means of shoulder injury
prevention. Based on this finding we elaborated a prevention program for climbers that approaches
scapular muscles and aims for specificity of the sport.
Based on the studies available, the exercise program for climbers encourages new researches aiming
prevention on upper extremities injuries.
Introduction
Climbing is a sport of high physical and psychological demand. Most of the time only parts of the hand and feet of the climber are in contact with the surface being climbed independently of its angle. The angle of the surface can have less then 90° (slabs), be vertical at 90° or inclined more than 90° (overhang). The climber’s hand and feet are used as tools to ascend a climbing route. Large part of the body weight and external support strength are applied to the climber’s hand being distributed to wrist, elbows and shoulders [1,2].
There are a few climbing modalities, and to make it more comprehensive between the differences of the ones most practiced, and their relations with mechanism of injury, we will focus in bouldering.
Bouldering the athlete climbs boulders that can vary on height, in average 16ft, sometimes more [3]. These blocks can be found in nature or can be artificially build, inside gyms for example. Bouldering does not require wearing any protection equipment, like rope and harness. The athlete will only need crash pads, a type of portable mattress used to brake the fall and landing, which also help to level the ground preventing ankle sprains. This form of rock-climbing can be done solo or in a group, the latter being the most advised since the partner can serve as spotters and in case of a fall can help to orient the falling climber’s body. Thus, minimizing more serious traumatic injuries, such as, trauma of the spine and head with the ground. The climber’s goal in any sub-modality is to “send” the route or problem, referred to as when they get to the top of the climbing route. Sending is successfully accomplished when the climber gets to the top without falling or in case of sport climbing, without resting on the rope. Sometimes a few or many attempts might be needed, which can take a toll on the body and lead to overuse injury [3].
Bouldering, lead climbing and speed climbing will be the sub-modalities of the first Olympic climbing competition scheduled to happen in the 2020 Summer Olympic Games in Tokio [4]. National climbing federations worldwide are supposed to figure out how to change training programs so they can prepare athletes to become potential Olympic gold medalists [4]. We can wait and see if there will be a change in injury pattern now that the athletes will have to practice all three sub-modalities or we can experiment adding prevention programs before damage is done.
Purpose
The present study aims to develop a shoulder injury prevention program for climbers based on the risks and
biomechanical demands related to the sport.
Methods
This is a narrative review. The search was performed thru the data base platforms: Pubmed, Embase, Lilacs,
The Cochrane Library and PEDro. We have included studies that use exercise as shoulder injury prevention,
as well as studies that analyzed the biomechanics of climbing. The selected studies were randomized clinical
trials, systematic reviews, longitudinal studies, and clinical guidelines.
We selected studies that showed muscle strengthening for the upper extremity, joint mobilization, stretching, functional demand and injuries in climbers.
Results
Climbing in general, combines movements that resemble those of Olympic gymnastics with a lot of explosive
movements, resistance and intense isometric gripping function [5]. It demands intermittent isometric
contraction of the forearm and hand’s muscles alternating with complex movements of the whole body [6].
With that we can start to understand some of the results of the research on epidemiology, where it is pointed
that most climbing related injuries occur on fingers, wrists, elbows and shoulders [7-10]. Nonetheless, knees
and ankle injuries are not uncommon due to potential falls to the ground or forceful impact of the body
against the surface being climbed, which in some cases is inevitable [8].
There are so many demanding and repetitive movements using only hands and feet on small holds that, over time especially ligaments and tendons of the upper limbs begin to undergo some adaptations. Studies performed through medical imaging, report an increase in the thickness of the cortical layer of the bones of the hands as well as increased tendon thickness and hypertrophy of the A2 and A4 pulleys of the fingers. These adaptations are probably induced by high mechanical stress during years of climbing, becoming thicker and more resistant to rupture [11]. This leads us to believe that in climbing, especially high-performance climbing, it is not enough to only increase the muscular strength of the upper limbs, it is also necessary to stimulate these adaptations to occur in the tendons and pulleys of the fingers [12]. The correct dose of this stimulus is not something discussed in the literature, and climbers do so by indication and instruction of more experienced climbers.
For the muscular system, two specific muscle functions were identified in climbing: Support muscles - mainly composed by the wrist and finger flexors, both of which are essential to allow gripping, and that is extremely important for the athlete’s performance in the sports and, also involves the tendinous structures mentioned above; Execution muscles - composed of the muscles of the shoulder girdle, latissimus dorsi and elbow flexors with forearm in pronation [12].
The climbing sub-modality directly influences the risk and types of injuries. Indoor climbing is safer and
more controlled than outdoor climbing. However, overuse injuries stand out [13]. The level of difficulty can
also be risk determinant. Elite climbers are most often affected by overuse injuries and for excessive exposure
levels (very small holds, strenuous movements and falls). While less experienced climbers are injured by
judgmental failure or lack of technique and suffer milder injuries such as abrasions [14]. Interestingly,
climbers are injured while climbing at their comfort level route graduation or below it [13]. The higher risk
is found within male climbers with more than ten years of climbing experience and that guide more complex
routes [14].
Amateur and professional climbing athletes have specific injuries, related to anatomical regions and movements unique to the sport [13]. About 60% of injuries affect fingers and wrist, the other 40% are divided between elbow and shoulder [15].
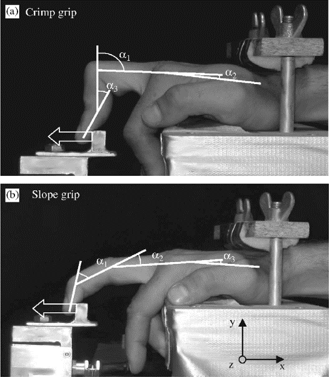
The finger flexor tendons and pulleys are the most affected area in the sport. This is true specially in bouldering, where the climber exerts extreme amount of force on small holds added to their body weight and explosive movementsp [16]. Besides that, if the foot slips from the hold or fall while one or more fingers are locked on a hold (called finger pockets), generate a sudden overload on the tendons, collateral ligaments and pulleys leading to injury [15]. The term "climber’s finger" has been used to describe lesions affecting the annular pulley system, especially A2, A3 and A4 from II to V finger. The injury and may vary in degrees of strain or rupture. The ruptures are usually accompanied by a “pop”, swelling and pain. In case of chronic injuries, the pain and feeling of weakness will be persistent [13]. Swelling and reproducible pain may be found at physical examination as well as the visualization of the tendon bowstringing beneath the skin. The recommendations found in the literature for the prevention of such injuries are: give preference to the "extended" or "slope" grip (Figure 1-b), which exerts less stress on the pulleys than the crimp grip (figure 1-a); and the suspension training on the fingers on the hangboard (figure 2), strengthening board with different holds, gradual increase of time and weight. Thus, providing the gradual stress on the mentioned structures as a stimulus making the tendons thicker and more resistant [12,1].

Different grips and specific climbing movements affect the biomechanics of the wrist, forearm and elbow. Which when combined with repetitive micro injuries and the fact that the tendon takes a long time to regenerate can be a disastrous recipe and cause some issues. An example of injury due to the concomitance of inappropriate biomechanics and overuse is the "climber's elbow". Where there is a rupture, of variable size, in the musculotendinous junction of the brachialis muscle.
Traverse climbing where there are intense movements of elbow flexion with forearm pronation, and insufficient activation of the biceps brachii in the position of flexion and pronation can lead to a compensatory activation of the brachial muscle and eventually acute or chronic overload [13]. In this case it is common to observe climbers complaining of pain during elbow flexion with pronation and is often presented after a long or difficult climb, or after raising the difficulty level of the climb without sufficient rest intervals between training sessions. The physical examination commonly accuses pain in the anterior region of the elbow near the distal portion of the brachial muscle leading to the common, but mistaken, diagnosis of tendinopathy of the biceps brachii. Pain presents worsening during elbow flexion with forearm in pronation and relief in flexion with forearm in supination [7].
Other soft tissue lesions affecting the elbow include medial and lateral epicondylitis, and triceps tendinopathy. Medial epicondylitis can arise from overload and micro trauma of the superficial flexor muscles of the fingers, flexors of the wrist, and pronator teres muscles. Which all have insertion in the medial epicondyle and all but pronator teres are involved in maintaining the grip of the hand. Lateral epicondylitis may appear with overloading of the extensor fingers and wrist and supinator muscle, which are inserted into the lateral epicondyle of the humerus. In climbing the overload of the extensor muscles, which tend to be less trained, can be due to the fact that the greater strength potential of the flexor muscles of the fingers and wrist is optimized when the wrist is in extension and ulnar deviation [15].
The tendinopathies affecting the triceps brachii muscle can be the result of repetitive shoulder and elbow extension movements to sustain body weight when the climber raises his body to a higher surface than himself, for example, on a plateau or when he reaches the end of the route and tops off the rock. Or simply by the continuous shoulder flexion with elbow extension during some of the climb, especially when resting on the wall [15].
In similarity to overhead athletes or other that lifting weight overhead, climbers can be affected by impingement syndrome. And according to orthopedist Patrick Peters, can be divided into two categories. The primary impingement syndrome is due to imbalance and lesions of the rotator cuff muscles, caused by ineffective and non-specific training. Possibly leading to classic signs of impact syndrome such as painful arch, positive Hawkins test and positive abduction test [15]. The secondary impingement syndrome may result from dysfunctions such as labral injury (SLAP) with superior instability, since the position of the arm over the head can lead to greater shear and overload of the biceps tendon. However, the clinical presentations of SLAP lesions can vary greatly. The isolated injury of the tendon of the long head of the biceps can also occur and is most often associated with hangboard training. Where most climbers hang without activating the scapular muscles and are likely to lead to superiority of the humeral head and greater compression of the sub-acromial structures. Other common lesions are muscle lesions of the latissimus dorsi, rhomboid, and lower trapezius muscles. Glenohumeral dislocation is rare, representing about 4% of upper limb injuries in sports [15].
Climbing is a relatively new sport, it appeared in Brazil in the early 1980s as an alternative of physical and technical training for mountaineers [18]. Since then, climbing has become an increasingly popular sport and according to the International Federation of Sport Climbing (IFSC) the approximate number of sports fans in the world reached 25 million in 2015 [19]. The number of climbers and climbing gyms increased in 50% from 2001 to 2010 [19]. Besides that, with climbing becoming an Olympic sport for the 2020 Summer Olympic Games, the trend is that the sport will win even more fans. With this is expected an increase in the number of injuries related to climbing [19,20]. According to a study done with British climbers, the main sources of treatment or advice for climbers were firstly physical therapists (18%), secondly other climbers (14%) and thirdly doctors (11%) [9]. Therefore, reinforcing Physical Therapist’s acquaintance and knowledge of injury prevention and rehabilitation in climbing.
Scapular muscles strengthening is used to treat dysfunction of the shoulder. It is a challenge for physiotherapists
to reestablish the control and balanced co-activation of the scapular muscles [21].
Although the literature shows a lack on preventive exercises for climbers, recent evidence describes therapeutic exercises on shoulder injury management in many other sports modalities as well as biomechanical analyzes of muscle contraction on the shoulder [22,23].
A randomized clinical trial aimed to evaluate the effect of an injury prevention program in 45 handball teams (660 players). The intervention group performed the exercises in the program three times per week during seven months as part of the warm-up routine before the games. The intent of the exercise was to gain muscle strength for internal and external rotation of the glenohumeral joint, and strengthen the scapular muscles. The program also added exercises to enhance kinetic chain and provide thoracic spine mobility. The intervention group showed 17% (IC95% 16% a 19%) of shoulder alterations throughout the season, the control group presented 23% (IC95% 21% a 26%) of shoulder problems. Thus, resulting in a mean difference of 6% between groups. This program offers a great clinical strategy to reduce the risk of injury to handball players [24].
Some muscles are key in stabilizing the shoulder girdle. Strengthening the lower trapezius muscles, medial trapezius, anterior serratus can minimize intermuscular imbalances and thus prevent physical aches and pains. Evidence-based exercises seek concepts to stabilize the muscles of the shoulder girdle. One of the concepts are in the 3D movements of the shoulder, exercises with upward rotation, external rotation and posterior tilt are important joint [25,26].
Based on electromyography findings on muscle activation around the scapula, push-up exercises cause large amounts of activation of the serratus anterior and produce minimal activation of the upper trapezius [27].
Individuals with scapular dyskinesia often demonstrate upper trapezius hyperactivity and medial and inferior trapezius muscle weakness. Strengthening the lower trapezius, medial trapezius, and serratus anterior may decrease scapular muscles imbalances and thus prevent physical aches and pains [28].
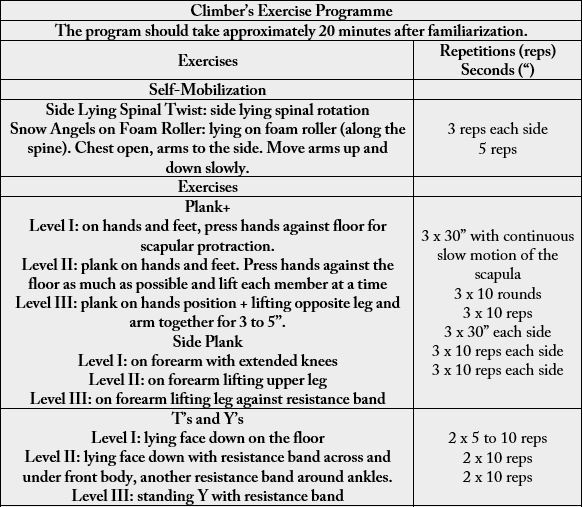
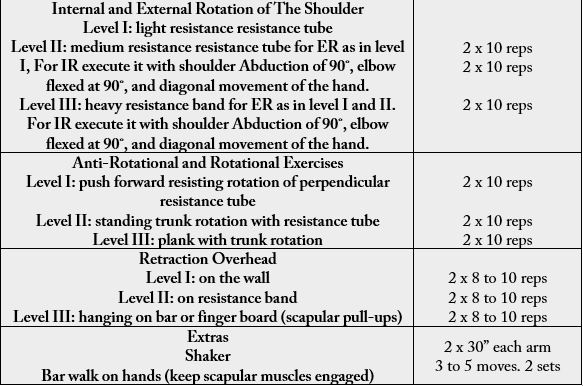
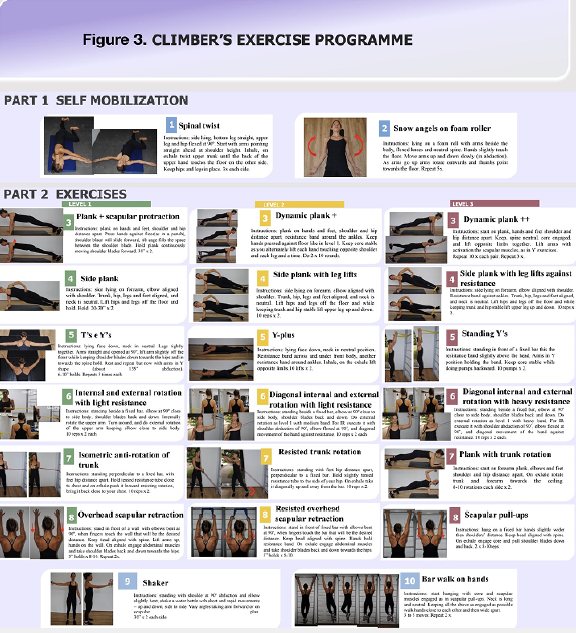
Based on the findings, we developed a program of therapeutic exercises for climbers. This program is divided in three levels, going from easiest (level one) to more complex (level three) exercises. Each exercise is followed by a progressive version on the subsequent levels. The number of series of repetitions, or holds in seconds were kept low to avoid muscle fatigue. Before performing the exercise program as part of a warm up, it is advised that the athlete practices the same exercises under proper supervision in a regular training routine, thus avoiding compensations.
All levels start with mobility exercises – part 1 in the exercise program attachment. In part 2 of the attachment there are three different levels: The level one exercises are done in a mostly isometric fashion and lighter resistance is used – bodyweight or a lighter resistance elastic band; The level two exercises are done more dynamically and medium resistance is used – medium resistance elastic bands; Level three exercises are composed of more complex movements and heavier resistance is used – heavy resistance elastic band and full body hanging weight. As well as part 1, part 3 of the exercise program is supposed to be done at the end of all exercises’ levels. It is composed of two exercises with focus on proprioception, during shaking of a water bottle and scapular muscle activation awareness while hanging and walking the hands on a bar. Each level should be practiced at least twice a week for three weeks before moving on to the next level. (Table 1 and Figure 3)
Discussion
Currently, studies have shown that many of the muscular and articular structures of our body are connected
hence influence each other. As an example, a study made with healthy overhead athletes reported that the
fatigue of the stabilizing muscles of the scapula can lead to a kinematic alteration of the elbow joint [29].
Another study reports how the strengthening of the proximal hip muscles (gluteus maximal and medius) can
promote functional gain and in the two joints below (knee and ankle). And in analogy to this, a second study
proposed that the scapular muscles, as well as the hip, can serve as a stabilizing structure for the elbow, wrist
and finger joints thus promoting functional gain of these joints [30,31]. This hypothesis has been proven
through other studies that show that the lack of strength or the simple activation of the scapular muscles
can lead to an overload of the wrist extensor muscles and consequently lead to an elbow injury such as lateral
epicondylitis [32]. In addition, some articles suggest the relation between activation of the scapular muscles
and the increase of grip strength [31] or even the contraction of the abdominal muscles as an optimizer for
the activation of the scapular muscles in dynamic exercises for the shoulder [33].
We must consider that motor learning can have a beneficial effect not only on gaining strength, but also on integrating neuromuscular activation in the climbing movements related to the scapula. An athlete can learn to activate the scapular muscles in more static movements and gradually evolve to activate those muscles during more complex and dynamic movements. Hence, the neuromuscular recruitment will be integrated into the routine of movements, optimizing the scapular function and preventing [34].
Regardless of the sub-modality of climbing, it is hypothesized that this prevention program can collaborate to optimize the function of the upper limbs and to reduce the number of injuries due to the climbing biomechanics. That would be possible through the neuromuscular activation and strengthening of the scapular muscles, the muscles of the forearms and hands. We should state that although the program is focused on upper limbs due to the result of epidemiological research, the program includes some lower limb exercises that are also extremely important for climbing. In addition, self-mobilizations are included to maintain or restore tissue mobility and nutrition.
A prevention program proposal is not new. Since 2004 FIFA has focused on soccer injury prevention strategies and recently a systematic review has reported that the use of the prevention program FIFA11 + has resulted in the reduction of soccer related injuries by 39% [35]. In resume, a 20-minute program, which serves as a warm-up, can avoid expenses with surgeries, months of rehabilitation and time off the field. Regardless of whether climbing is still not a large-scale sport as soccer, athletes, professional or amateur, enjoy climbing and usually want to do it for as many years of their lives as possible. Climbers start early, 38% of them are under the age of 18, and continue to climb above 60 years of age (IFSC-climbing.org). This is a unique group of individuals, and many of them believe that most physicians and physiotherapists do not understand their sport and cannot help them heal or rehabilitate from their injuries.
We hope this is just the beginning of a larger project along with the scientific community, whether they are climbers themselves or not. And that we can achieve a common good always aiming to keep our patients healthy. This study has a few limitations. The prevention program was based on epidemiological findings available in the literature. Thus, it may be interesting to carry out a more current and local epidemiological survey. In addition, it has not been tested on athletes to assess its effectiveness. As a suggestion for future research besides taking the prevention program into practice, we can think of performing functional tests on groups of athletes to analyze their biomechanical deficits and then adjust the prevention program based on the results. We can also look for effects of the exercise program on climber’s performance [36].
Clinical Implications
Climbing is gaining popularity. Healthcare providers, especially Physical Therapists, will need to acquire
familiarity with climbing injuries in order to recognize and manage these injuries effectively. Also, the
knowledge around mechanisms of injury will lead to development of more preventive measures which
healthcare providers can start to implement in their practice.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!