Biography
Interests
Dr. Egbe-Nwiyi, T. N.1, Dr. Kumbongsi, N. S.1 & Dr. Shamaki, B. U.2*
1Department of Veterinary Pathology, Faculty of Veterinary Medicine, University of Maiduguri, Nigeria
2Department of Veterinary Physiology, Pharmacology and Biochemistry, Faculty of Veterinary Medicine, University of Maiduguri, Nigeria
*Correspondence to: Dr. Shamaki, B. U., Department of Veterinary Physiology, Pharmacology and Biochemistry, Faculty of Veterinary Medicine, University of Maiduguri, Nigeria.
Copyright © 2018 Dr. Shamaki, B. U., et al., This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Seventy-two healthy adult albino rats of both sexes weighing 180-200 g were used for investigate
the therapeutic efficacy of double doses of fansidar® (25mg perimethamine and 500mg/
sulfadoxine), chloroquine, berenil® (Diminazine aceturate) and a combination of the drugs in
the treatment of experimental Federe strain of Trypanosome brucei brucei infection. The rats were
separated into nine groups (A-I) of eight rats each. Rats in groups B-1 were each infected with
T. b. brucei (1x106 trypanosomes as group A served as uninfected untreated control. Group B
rats served as infected untreated control, while rats in groups C, D, and E were treated with 3.5
mg/kg of berenil®, 1.0ml/5kg of fansidar® and 0.5ml/10kg of chloroquine respectively. Group
F, G and H animals were treated with 7.0mg/kg of berenil®, 2.0ml/5kg of fansidar® and 1.0ml/10kg of chloroquine respectively while rats in group I were administered with (double doses)
a combination of 7.0mg/kg of berenil®, 2.0 ml/5kg of fansidar® and 1.0ml/10kg of chloroquine.
Parasitaemia developed within 4-6 days’ post-infection (PI) and treatment was instituted on day 8
PI. Pre-patent period was comparable (P>0.05) in all the infected groups while survival time was
shorter (P<0.05) in groups B, D and E. Splenomegaly and hepatomegally were higher in groups
B, D and E. anaemia observed was more severe (P<0.05) in groups B, D and E. there was relapse
of infection in 2 rats each in groups C and F while one in group I. Showing 75 % diminazene
aceturate (berenil®) treatment success. In conclusion double doses of Fansidar® or chloroquine or
in combination with berenil® appeared not to be efficacious while single or double dose of berenil®
achieved remarkable success.
Introduction
Trypanosomosis in animals is mainly caused by T. vivax, T. congolense, T. brucei and T. equiperdum. Human
beings are not left out as T. brucei rhadesiense and T. Brucei gambeinse cause sleeping sickness in man
(Radostits et al., 1994). Trypanosomosis is one of the major constraints to livestock production in Nigeria
and Africa [1]. Affected animals show poor milk production, weight loss, orchitis in males, infertility in
females, anaemia, emaciation and even death if untreated [1].
Trypanosomosis have antigenic variations which enable them invade host immune response (Halliwell and Gorman, 1989). Much work has been done on the chemotherapeutic management of trypanosomosis in various animal species [2]. Diminazane aceturate is one of the oldest trypanocides and remains the drug of choice and it is only effective where the parasites have not crossed the blood brain barrier (BBB) [3]. Presently, few available trypanocides are very expensive and out of the reach of the local farmers [2,4].
It has been reported that trypanosomosis due to T. brucei brucei was resistant to single doses of chloroquine®, Metakalfin, Camoquine®, Artesunate and Fansidar® [4,5]. These drugs are very remarkably efficacious in the treatment of malaria parasite in man caused by Plasmodium falciparum. Both Trypanosomosis and Plasmodiosis are caused by protozoan organisms [1,6].
This study was therefore designed to ascertain the level of efficacy of double doses of Fansidar®, chloroquine® berenil® and a combination of these drugs in the treatment of T. brucei brucei infection of rats.
Materials and Methods
Seventy-two (72) healthy adult albino rats of both sexes weighing 180-200g obtained from the Nigerian
Institute of Trypanosomosis Research (NITR), VOM, Plateau State, Nigeria were used. They were allowed
to acclimatize for two weeks in the Veterinary Pathology Laboratory of the University of Maiduguri. The
rats were maintained on a standard laboratory diet (Vital Feeds Ltd, Jos) and housed in clean plastic cages
at ambient temperature (30-35oC). Water was provided ad libitum. Before the commencement of the study,
the rats were screened for the presence of haemoparasites (Jain, 1986).
Trypanosoma brucei brucei (Federe strain) were obtained from NITR, VOM, Nigeria. The parasites were
maintained by serial passages in mice and each rat was inoculated intra-peritoneally with 0.5ml of cold
glucose saline (pH 7.4) diluted with blood containing approximately 1x106 trypanosomes.
The rats were divided into nine groups (A-I) of 8 rats each. The rat’s inn group B-I were each infected with
Federe strain of T. b. Brucei. Groups A and B rats served as uninfected untreated and infected untreated
controls respectively. Rats in groups C, D and E were treated with 3.5mg/kg of berenil®, 1.0ml/5kg of
Fansidar® and 0.5ml/10kg of Chloroquine respectively. Groups F, G, and H animals were treated with 7.0mg/kg of berenil®, 2.0ml/5kg of Fansidar® and 1.0ml/5kg of Chloroquine® respectively while rats in group
I were treated with (double doses) a combination of 7.0mg/kg of berenil®, 2.0ml/5kg of Fansidar® and 1.0ml/10kg of Chloroquine®.
Fansidar® (25ml) perimethanine 500 mg Sulfadoxine, (SWIPHA, Nigeria) and 7% dimanazene aceturate
(Berenil®, KEPRO, B. V. Holland) and Chloroquine phosphate were prepared for administration following
the Manufacturers’ specifications. The drugs were given intramuscularly. On day 8 post-infection when
parasitaemia was well established, the infected rats were treated. Tail vein blood samples were collected
from the rats before and after trypanosome inoculations in order to assess the likely trypanocidal effects of
the drugs. The parameters used in the assessment of the drugs included the presence of the parasites in the
blood, Packed Cell Volume (PCV%) and rate and frequency of death. The parasitaemia was determined
every 2 days by haemocytometry while the PCV determined every 4 days by micro-haemocrit method (Jain,
1986) was used to assess haematological response.
When the rats died, post-mortem (PM) was carried out on each rat using conventional procedure (Igbokwe,
1989). The liver and spleen were harvested, grossly examined and weighed.
Data obtained were summarized as means ± Standard Deviations (SD) and were compared by Analysis of
Variance (ANOVA) and Students T-test [7].
Results
The infected rats developed parasitaemia within 4-6 days’ post-infection (pi). The mean pre-patent periods and survival time (ST) in groups B-1 are presented in table 1.
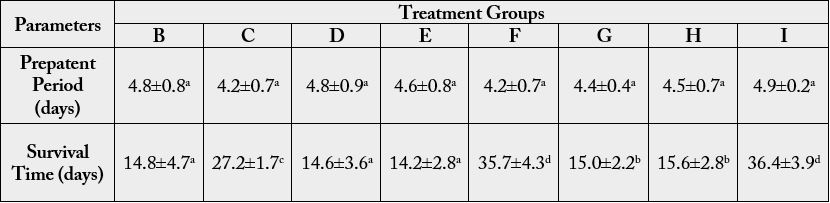
a, b, c, d values in rows with different superscript differ significantly (p<0.05)
There was no significant difference (P>0.05) in the pre-patent periods among the infected groups. Parasitaemia reached peak on day 8 Post--infection (Pi). The infected and treated rats in groups C, F and I became aparasitaemic for 20 days’ post-treatment (PT) and became parasitaemic again from day 30 Pi (22 days’ post-treatment) (Fig 1). The level of parasitaemia decreased slightly in groups D, E and H after treatment.
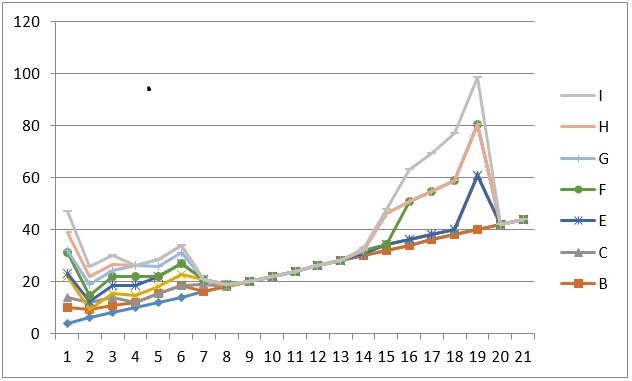
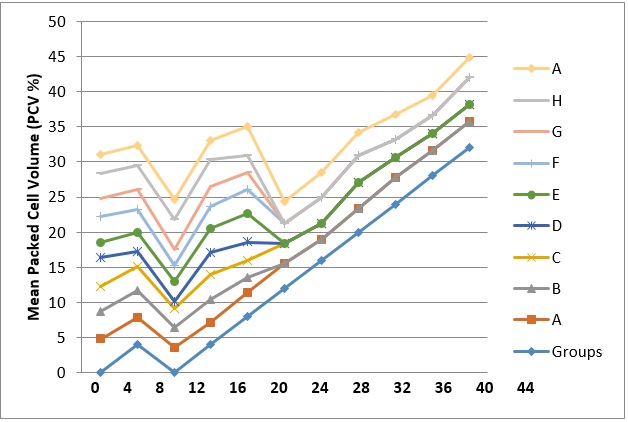
The Packed Cell Volume (PCV) decreased remarkably in all the infected groups (Fig. 2) and after treatment, the PCV of the rats in groups C, F and I increased for some days but later decreased (Fig. 2). There was relapse of infection in 2 rats each in groups C, and F while in group I, it was in one rat.
The clinical signs that were prominent were rapid weight loss, intermittent pyrexid, weakness, dullness and pale mucus membranes. Splenomegaly and hepatomegaly were observed in all infected rats and the levels were higher (P<0.05) in groups B, D, E, G, and H when compared with those of groups C (infected and treated with 3.5mg/kg of Berenil®), F (infected and treated with 7.0mg/kg of Berenil® and I (infected and treated with combinations of 2.0mg/5kg of fansidar®, 1.0ml/10kg of chloroquine® and 7.0mg/kg of berenil®).
The survival time (ST) was shorter (P<0.05) in groups B, D and E than in groups C, F, G, H and I (table 1). The ST was comparable (P>0.05) in groups B, D, and E (Table 1) and longer (P>0.05) in groups G and H when compared with groups B, D and E and shorter (P<0.05) when compared with groups C, F and I. The group C rats exhibited longer (P<0.05) ST when compared with those observed in groups B, D, E, G and H but shorter (P<0.05) when compared with the values recorded in groups F and I.
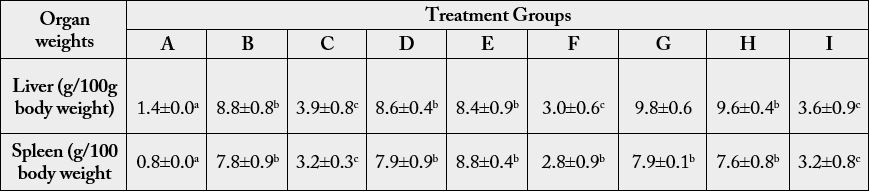
a, b, c, d values in rows with different superscript differ significantly (p<0.05)
Discussion
The parasitaemia which appeared in the infected groups within 4-6 days PI was slightly longer than the one
(2-4 days Pi) observed earlier in (Egbe-Nwiyi and Yakubu, 2014) in rats infected with the same strain of T.
b. brucei. The study has demonstrated that Fansidar® or Chloroquine irrespective of dose or in combination
with other conventional trypanocides have no anti-trypanosomal properties. The drugs insignificantly
reduced the level of parasitaemia.
The survival time (ST) was slightly prolonged in the rats infected and treated with double doses of Fansidar® or Chloroquine® but the ST could not be compared with the ones observed in infected and treated with 3.5mg/kg of Berenil® or 7.0 mg/kg of Berenil® with or without the combinations of Fansidar® and chloroquine®. The ST in the infected rats and treated with single doses of Fansidar® or chloroquine® was comparable with the ST observed in infected untreated rats and this agrees with the findings of Egbe-Nwiyi and Igawe (2013), but disagrees with the reports of previous workers (Egbe-Nwiyi et al., 2005; 2011) where the ST in rats infected with T. b. brucei and treated with Metakelfin® alone and Camoquine® alone was longer than that of infected untreated.
There were aparasiteamic and parasitaemic stages in groups C, F and I as there was relapse of infection in 2 rats each in groups C (infected and treated with 3.5mg/kg of Berenil® and F (infected and treated with 7.0mg/kg of Beneril® alone) and one rat in group I, and this is in consonance with earlier reports (Onyeyili and Onwualu, 1991; Egbe-Nwiyi and Igwe, 2013). Relapse of infection in rats treated with higher doses of Berenil® (10-21mg/kg) has earlier been reported (Onyeyil and Onwualu, 1991; Egbe-Nwiyi et al., 2003). The relapse observed in some rats could not be attributed to under dosage or drug resistance as higher percentage of the rats in groups C, F and I were cured of the infection as no trypanosomeswere seen in peripheral blood 3.6 days after treatment [8].
It is possible some of the trypanosomes entered into drug inaccessible sites such as the brain, microcirculation, heart, spleen and bone marrow (Jennings et al., 1979; Onyeyili and Anika, Mamman et al., 1994) or the time interval between infection and treatment on day 8 PI was long. Because rats infected with the same strain (Federe strain) of T. b. brucei and treated with 7.0 mg/kg of berenil® on day 6 pi did not show relapse. But there was relapse in rats infected with T. b. Brucei and treated on day 12 post infection (Egbe- Nwiyi and Yakubu, 2014). Diminazene aceturate is effictive in the treatment of acute animal trypanosomosis and becomes less effective as the time interval increases (Jennings et al., 1977, Onyeyili, 1984).
The drug also becomes ineffective once the central nervous system (CNS) is involved and brain was reported to be the main source of relapse in T. Brucei infection (Jennings et al., 1977a; Chukwu et al., 1990). Conventional trypanocides like berenil® are not usually in sufficient quantity to cross the blood-brain barrier (BBB), (Aliu, 2007) [3].
The Fansidar® and chloroquine irrespective of dose have demonstrated that they do not possess antitrypanosoma properties. Trypanosomosis and plasmodosis are both protozoan diseases and drug like Fansidar® considering its composition (pyrimethamine and sulfadoxine) is used in treating plasmodosis Toxoplasmosis which are protozoan diseases (Webmed, 2015).
The inability of the Fansidar® or chloroquinbe at double doses to clear the trypanosomes from the peripheral blood of the infected rats suggest they lack basic anti-trypanosomal properties which berenil® has. The two druigs are commonly used for the treatment of human plasmodosis. (Plasmodium falciparum). Plasmodosis and trypanosomosis are both protozoal infectioons. Fansidar® and chloroquine are active against the asexual erythrocytic stages of plasmodium falciparum (Webmed, 2015; NIS, 2015).
Fansidar® is composed of sulfadoxine and pyrimethamine which are folic acid antagonists. Sulfadoxine inhibits the activity of dihydropteroate synthase while pyrimethamine inhibits dihydrofolate reductase (Webmed, 2015). Chloroquine is a synthetic aminoquinoline that acts by binding to the protozoal or parasitic DNA and preventing DNA and RNA production and subsequent protein synthesis (NIS, 2015).
Diminazine aceturate (Berenil®) on the other hand, is one of the aromatic diamidines which are active against protozoal infections and are thought to combine with nucleic acids producing partial uncoiling and denaturation of the DNA double helix. They selectively block kinetoplast DNA and subsequently produce dyskinetoplastic trypanosomes [3]. The drug can also prevent oxygen uptake, phospholipid synthesis and basic amino acid transport in the trypanosomes (Hill and Hunter, 1986; Gutteridge, 1966; 1969). The release of the trypanosomes from the micro-circulation into the general pool or circulation reported [9].
The anaemia recorded in all the infected groups based on low PCV was more severe in groups B, D, E, G and H. anaemia is a common finding in African animal trypanosomosis but the severity of anaemia differs from one species of trypanosome to another [10,11]. It also depends on the virulence of the trypanosomes species and host factors such as age, breed, nutritional status and host of others [11,12]. The splenomegaly and hepatomegaly observed in all the infected groups, and these findings agreed with earlier reports in T. brucei infection [1]. Splenomegaly and hepatomegaly were both associated with erythrophagocytosis [13]. And the latter might have contributed to the more severe anaemia seen in groups B, D, E, G and H.
The gradual recovery of PCV in those rats amenable to berenil® treatment in groups C (6 rats), F (6 rats) and I (7 rats) demonstrated among other things that the drug (berenil®) was in sufficient concentration to have cleared the trypanosomes from the peripheral blood. There was high percentage of treatment success in groups C, F and I and the PCV of the rats with relapse infection decreased gradually until they died and this observation did not differ from earlier reports (Egbe-Nwiyi et al., 2014).
Conclusion
Based on the above findings, and the differences in their (drugs) mode of actions, it was therefore concluded
that chloroquine and fansidar®, single or in combination, are not effective in the treatment of T. b. brucei
infection in animals, double doses of Fansidar® and Chloroquine appeared not to be effective in the treatment
of T. b. Brucei infection even when combined with berenil® at 3.5mg/kg or 7.0mg/kg. But berenil® at 3.5mg/kg or 7.0mg/kg achieved 75% success. Relapse infection occurred in 2 rats each in group C (infected
and treated with 3.5mg/kg of berenil® and F (infected and treated with 7.0mg/kg of berenil®) and 1 rat in
group I (infected and treated with 2.0 mg/5kg of Fansidar®, 1.0mg/10kg of chloroquine and 7.0mg/kg of
berenil®). There is need to evaluate the pathogenicity of the relapsed strain of the T. b. Brucei.
Recommendation
Diaminazene aceturate (berenil) can be used as a single dose, and within the range of 3.5mg/kg - 7.0mg/kg for the effective treatment of T. b. brucei infections in animals. Further work should be carried out on the
relapsed strain to evaluate its pathogenicity.
Acknowledgement
The authors wish to acknowledge and appreciate the technical assistance of Laboratory staff at NITR,
Vom and Veterinary Pathology Laboratory in the Faculty of Veterinary Medicine, University of Maiduguri, Nigeria.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!