Biography
Interests
Shon Shmushkevich1,2#, Massimo Baudo3#, Mahmoud Morsi4, Mariam Khobsa5, Mohamed Ismael6, Ayah Hassan, A.7, Mostafa Rahouma8 & Mohamed Rahouma9*#
1Zanvyl Krieger School of Arts & Sciences, Johns Hopkins University, Baltimore, Maryland, USA
2Department of Cardiothoracic Surgery, Weill Cornell Medicine/New York Presbyterian Hospital, New York, NY, USA
3Department of Cardiac Surgery, Spedali Civili di Brescia, Brescia, Italy
4Department of General Surgery, Montefiore Health System, New York, NY, USA
5Department of Cardiology Overlake Medical Center, Bellevue, WA, US
6Department of Microbiology, High Institute of Public Health, Alexandria University, Egypt
7Department of Pharmacognosy, Faculty of Pharmacy, Cairo University, Egypt
8Department of Information Technology, National Cancer Institute, Cairo University, Egypt
9Department of Surgical Oncology, National Cancer Institute, Cairo University, Cairo, Egypt
#Equal contribution
*Correspondence to: Dr. Mohamed Rahouma, Department of Surgical Oncology, National Cancer Institute, Cairo University, Cairo, Egypt.
Copyright © 2020 Dr. Mohamed Rahouma, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
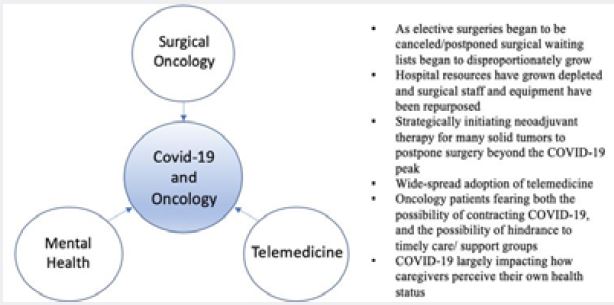
Surgical Oncology
Due to the spread of COVID-19, many medical institutions began to cancel/postpone elective procedures
out of concerns for safety. The American College of Surgeons (ACS) and the Centers for Disease Control
and Prevention (CDC) recommended cancelling or postponing non-emergent surgeries beginning in March
2020 [1]. This directly affected a wide range of oncological institutions, which had to adapt swiftly. With
these policies in place, surgical waiting lists began to disproportionately grow [1,2]. Throughout this period,
and leading up to today, many hospital resources have grown depleted and surgical staff and equipment have
been repurposed [1].
Through implementing telemedicine (touched upon in the next section), patient office visits continued virtually. The far-reaching acceptance of this new virtual based medicine allows for patients to be evaluated, assessed, and counseled without having to leave their homes [1]. This has large upsides since when nonemergent procedures resume, patients will already have fulfilled their preoperative requirements [1]. However, this new era of widespread telemedicine has its downsides. For one, vital signs can no longer be acceptably recorded since the patient is not physically present during the office visit - this creates a potential for a misdiagnosis and poor follow-up.
As more operating rooms open for non-emergency procedures, many new considerations must be made. Some important considerations include availability of the medical staff and hospital resources, the transmission risk of COVID-19 to health-care workers and non-infected patients, and perioperative outcomes when triaging surgeries [1,3]. The adoption of outpatient surgical procedures must be considered whenever safe through utilizing risk predictors [1,4-6].
The Department of Surgical Oncology at MD Anderson Cancer Center is one example of an effective center, which clinically adapted to meet the demands of cancer patients throughout the current pandemic. Since the department mostly favored neoadjuvant therapy for many solid tumors, they strategically initiated or continued this treatment sequencing when possible to postpone surgery to beyond the COVID-19 peak in their respective hometown of Houston, Texas [7]. Throughout this time, they were also able to have each disease site group continue to formally review new patients to reach consensus regarding treatment plans (even before patients set out to travel to the institution) [7].
At this institution, patients will receive a prompt operation if they are affected by a localized disease with potential for cure and don’t have indication for chemotherapy [7]. On the other hand, patients who needs extensive gastrointestinal surgery, such as Whipple procedure for pancreatic adenocarcinoma, major hepatectomy for colorectal liver metastases, and retroperitoneal sarcomas, are carefully reviewed to balance the risks of delaying surgery versus excessive chemotherapy causing organ damage or performance status decline [7]. Thanks to the clinic’s extensive experience with neoadjuvant therapy, they are able to selectively extend neoadjuvant chemotherapy or chemoradiation, which pushes the surgery out another 2 months for many patients with gastrointestinal cancers [7].
It is important to note that with the reopening of operating theaters for non-emergency procedures, minimally invasive robotic surgical systems may be of tremendous importance to minimize COVID-19 spread. Different reviews suggest that robotic surgery is associated with improved clinical outcomes for patients [1,8,9]. This type of surgery is associated with lower rates of conversion to laparotomy and decreased complication rates compared to abdominal and conventional laparoscopy [1,9]. With better clinical outcomes there is a lower likelihood of overnight admission when compared to conventional laparoscopy [1]. A robotic surgical route more effectively safeguards COVID-19-negative individuals from prolonged hospital stay, which at the current stage of the pandemic is crucial [1]. Medical professionals must take every precaution to minimize patient time spent inside the hospital, since it will always be a potential source of transmission [1].
Telemedicine
Many drastic changes in clinical medicine were implemented in the era of COVID-19. One significant
change was the wide-spread adoption of telemedicine. As previous reviews have noted, it is vital to maintain
the same level of safety and quality of care [10]. Prior to the COVID-19 pandemic many care delivery
regulations (e.g., supervision requirements) were in place to not only safeguard patients but also health care
professionals [10,11].
At the onset of the pandemic, many health clinics opted for solely remote service. However, as regulations eased, healthcare institutions began to deliver care not only for emergency cases. Therefore, it is crucial for health care professionals to create an appropriate balance for in-person visits/procedures vs a telemedicine approach [10]. The appropriate balance will have to come directly from the regulations put forth by policy makers of the respective city or country.
In addition to online chat and telephone-based peer support, we believe there should be a larger push to video based face-to-face support. One institution, for example, in order to reduce loneliness and isolation created 120 face-to-face virtual support groups when it became clear that it was unsafe to meet in person [12-14].
Important considerations in COVID-19 era telemedicine encapsulate how to appropriately perform objective patient assessments (e.g., patient-reported outcomes, physical examinations, laboratory tests, imaging, and endoscopy), monitor for any fraud or abuse, and maintain patient and physician satisfaction [10]. Through monitoring quality metrics, we will be able to determine the effect of telehealth on quality of care, which will guide our implementation of telemedicine for years to come. Examples of quality metrics include rates of emergency department visits, hospitalizations, and adverse events; delays in treatment initiation; and rates of adjuvant therapy receipt [10].
Of important note, telemedicine may provide greater and more flexible access to care, yet the technical requirements risk perpetuating disparities [10]. Certainly , there are patients who are not keen with the use of the internet and new communication technologies, particularly in older populations, which results in technology barriers to overcome [12-15]. One healthcare center developed a ‘tech tips’ guide in collaboration with support group leaders in order to make the transition to telemedicine communication much more bearable [12].
As per future considerations, telemedicine pattern research will provide insight into the extent and rapidity of telehealth adoption and regional variations in service [10]. Furthermore, there is a long-term potential in determining subspecialties and patient encounters for which telemedicine is most effective [10]. At the current stage of the pandemic, however, it is of utmost importance to protect our most vulnerable communities from contracting COVID-19, particularly patients with a history of cancer [10].
While more wide-spread telemedicine introduces new possibilities for research, it is important to remember that COVID-19 also severely affected clinical trials. Clinical trials tend to require frequent in-person visits, which are usually conducted in healthcare settings that are now more Coronavirus-19 exposed [10]. Early survey results show that the COVID-19 pandemic has significantly disrupted the conduct of clinical trials (e.g., enrollment; protocol adherence; and patient, physician, and supportive staff and services engagement) [10,16]. Telemedicine, in addition to dramatically changing clinical medicine, has fortunately kept many clinical trials operational, with many visits being carried out virtually [10].
Mental Health
Cancer patients are at a greater risk of severe events as a result of a COVID-19 infection, including higher
likelihood of being admitted to the intensive care unit, greater chance of requiring invasive ventilation, and
greater probability of death [17]. Due to this, many institutions began adapting their standards of care for
oncology patients [18]. With the newly proposed changes, much burden has been placed on the mental
wellbeing of both the oncology patients and the medical teams.
It is important to note that oncology patients do not only fear the possibility of contracting COVID-19, but possibility of hindrance to timely care and the ability to access sources of social and professional support [18]. Cancer patients have been more seriously affected with social isolation precautions and restricted with regard to their ability to access informal and formal sources of support [18]. The current changes coupled with the patients’ cancer diagnosis creates a troubling mental state. The field of psycho-oncology must seek alternative ways in which to identify patients in need and to whom there needs to be special attention granted throughout this difficult time [18].
With mental health of cancer patients being vitally important, it is just as important to prioritize mental health for medical professionals and employees of medical/cancer organizations. COVID-19 largely impacts how caregivers perceive their own health status; increased their feelings of fear, panic, vulnerability and loss of control; and isolated them from family, friends, and health care providers [18]. Social relations play a critical role in mental health and emotional well-being [18] Furthermore, loneliness is a known risk factor for all causes of morbidity and mortality [18-20].
A recent study showed that every aspect of the work done by cancer organizations has been affected to varying degrees by the pandemic [21]. Eighty-nine percent of organizations reported that they had to change their services for patients with cancer while they were experiencing an increase in calls and requests for assistance from patients with cancer [21]. Fifty-seven percent of organizations have had an increase in the number of calls and emails that they have received, with a mean increase of 44% [21].
However, while the need for cancer patient support dramatically rose, the organizations were forced to cut back on their activities, advocacy, and research, with half of the organizations involved in raising awareness reported having to change their activities by cancelling or postponing events [21]. Furthermore, many of the organizations are struggling financially and only 5% felt that they were “confident of their financial position” during this time [21].
As most organizations raise money through fundraising events, the majority of which being cancelled, and donors also facing financial uncertainty, leading to a decrease in donations - the situation for many oncological clinics being dire [21]. It is absolutely necessary to make political institutions aware of this tremendous burden and seek for governmental financial assistance to these clinics. The frontline healthcare personnel who treat and support cancer patients must feel confident in treating their respective patients. We are certainly going to see many long-term effects of this critical time period, but it is our duty to care for the mental wellbeing of our fellow medics and our patients [22].
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!