Mohamed Magdy2, Ihab Eldessouki1, Ola Gaber1, Mohamed Kamel3*, Mohamed Rahouma3, Nagla
Abdelkarim1 & John Morris1
1College of Medicine, Division of Hematology-Oncology, University of Cincinnati, Cincinnati, USA
2Pediatric Oncology Senior Registrar, Children Cancer Hospital, Egypt
3National Cancer Institute, Surgical Oncology Department, Cairo University, Egypt
*Correspondence to: Dr. Mohamed Kamel, National Cancer Institute, Surgical Oncology
Department, Cairo University, Egypt.
Copyright © 2018 Mohamed Kamel, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 11 October 2018
Published: 14 November 2018
Keywords: Infantile; Hemangioendothelioma; Cardiovascular Complications
Abstract
Despite its rarity, Infantile hepatic hemangioendothelioma (IHHE) is the most common hepatic
vascular tumor in children [1]. According to the International Society for the Study of Vascular
Anomalies (ISSVA) classification, lesions can be classified into focal, multifocal and diffuse
[2]. While hepatomegaly is the most common presenting feature, IHHE may be accompanied
by cardiovascular complications, coagulopathies, hypothyroidism, and angiomatous and nonangiomatous
lesions [3-8]. Depending on the presentation and associated morbidities, treatment
options include observation, medical treatment and/or surgical resection. In rare occasions, liver
transplantation might be considered [2,9-13].
Introduction
Infantile hepatic hemangioendothelioma (IHHE) is the most common vascular tumor in the liver in
pediatric age group [1]. Most cases are diagnosed in the first 2 months of age (85%) and it is rare after the
age of 3 years [14].
While IHHE is benign in nature, it is frequently associated with several morbidities (i.e. visual, respiratory
and gastrointestinal) that might necessitate medical intervention. Moreover, life threatening conditions such
as congestive heart failure was reported with this disease [15].
Treatment options for IHHE vary widely depending on patients’ presentation and any associated morbidities.
Spontaneous regression within a year is almost always the natural course for asymptomatic lesions. While
oral steroid is the most widely used treatment, interferon alpha and propranolol are other available treatment
options [13,16,17]. Other more invasive treatment modalities include hepatic artery embolization, hepatic
artery ligation, resectional surgery and liver transplantation might also be considered in symptomatic cases
or those with associated complications [18].
Epidemiology, and Demographics
IHHE accounts for around 12% of all pediatric hepatic tumors [19-21]. IHHE has a female predominance
with a male to female ratio of 1:1.3-2. It has a higher incidence in preterm infants, and Caucasian population
[22-26].
Classification & Clinical Presentation
The International Society for the Study of Vascular Anomalies (ISSVA) classification is the most commonly
used classification. IHHE is classified into focal, multifocal and diffuse lesions based on the extent of
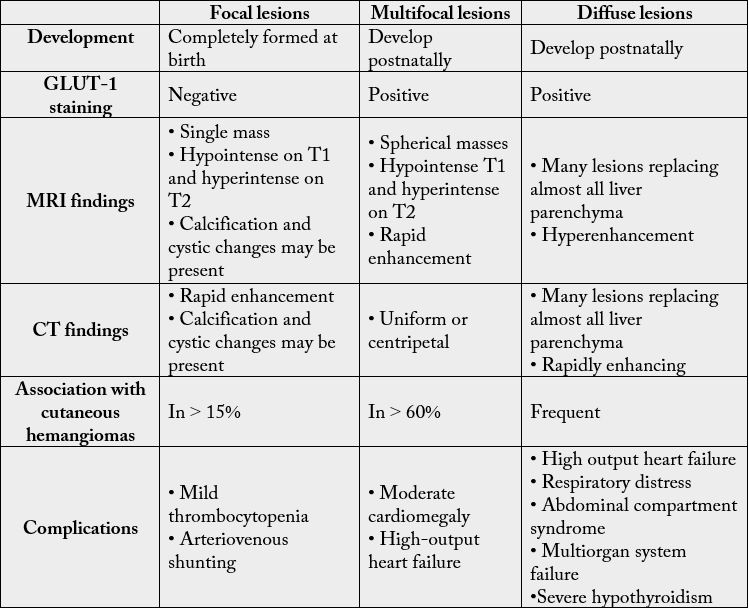
unaffected liver parenchyma [2,26]. (Table 1)
Table 1: Comparison of different types of IHHE
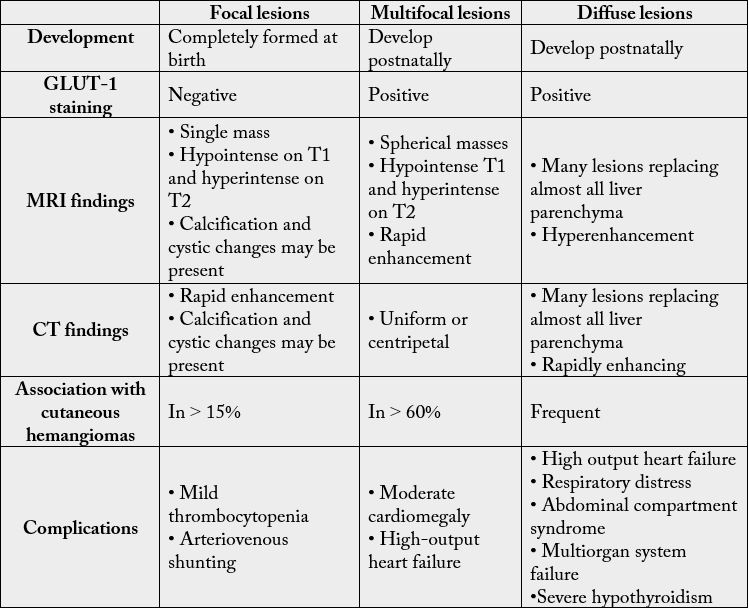
Most of the focal IHHE are asymptomatic, while multifocal and diffuse types are often symptomatic [2].
Clinical features of solitary lesions depends on the tumor size and the volume of shunted blood [27]. While,
patients with multifocal IHHE frequently present with hepatomegaly (83%), upper abdominal mass (66%),
cardiovascular failure, coagulopathy and/or jaundice [3,28]. Less common manifestations include vomiting,
splenomegaly, ascites, gastrointestinal bleeding, anemia, feeding difficulties and hepatic bruits [3,29].
Cardiovascular Complications
Due to arteriovenous shunting, IHHE can cause high output congestive heart failure particularly with
multifocal tumor. Cardiac failure may be the initial presentation which may misleadingly be attributed
to congenital heart disease [3,30-33]. As arteriovenous shunts are perfused from the hepatic artery, those
patients can be treated with hepatic artery ligation [34].
Coagulopathy
Coagulopathy that complicates IHHE is seen more frequently with multifocal IHHE [3]. It can be
secondary to activation and consumption of coagulation factors in a similar manner as with highly vascular
tumor (Kasabach-Merritt syndrome) [35-40].
Hypothyroidism
IHHE associated consumptive hypothyroidism was first reported by Huang et al. in 2000 [4]. Type
3 iodothyronine deiodinases produced by the tumor converts T4 and T3 to inactive metabolites. There
is a direct relationship between the incidence of hypothyroidism and the growth pattern of the tumor.
It is more common with diffuse IHHE and to a lesser extent with multifocal IHHE. Interestingly, this
complication regresses with regression of the tumor size or with liver transplant [6,41-43]. Since undetected
hypothyroidism can cause a permanent neurologic damage, defective hemostasis and cardiac symptoms, it is
crucial to monitor thyroid hormone levels when diffuse IHHE is diagnosed [26,44].
Cutaneous Angiomas
Cutaneous angiomas are commonly associated with IHHE (50% of patients) [5,45]. Kulungowski et al.
reported an incidence of 77.4% with multifocal IHHE, 53.3% with diffuse type and 15.3% with focal type
[6].
Non-Angiomatous Tumors
IHHE associated hepatic mesenchymal hamartomas may cause elevation in serum alpha-fetoprotein. In
addition, large brain hemangiomas that may be associated with multicentric IHHE have been reported
[7,8,46,47].
Diagnosis of IHHE
Imaging Studies
Multiple imaging modalities may be used for diagnosis and surveillance of IHHE including sonography,
CT, monitoring tumor’s growth and MRI.
Sonography
Sonography is useful in detecting fetal hepatic hemangioendothelioma as well as monitoring tumor’s growth
pattern and treatment response [48-52]. Characteristic features include complex heterogenous hypoechoic
masses, with occasional calcifications that can be attributed to central hemorrhage, necrosis, or fibrosis of the
lesion. The solitary lesions appear as round nodules consisting of tortuous markedly perfused cavities while
multifocal lesions may present as a solid tumor.
Computed Tomography (CT)
On non-contrast CT, IHHE appears as multiple hypo-attenuated well-demarcated nodules or masses, more
frequently in the periphery. Dynamic scans that use intravenous contrast material may show peripherally
enhanced lesions with no central enhancement. On delayed scans, a washout of the peripheral enhancement
and filling in of the center of the lesion can be seen. This is because of the slower blood flow within the lesion
compared to the rest of the liver [53]. Small lesions may show central enhancement initially which may
be considered equivalent to peripheral enhancements in large lesions [54]. Three Criteria were suggested
for diagnosis of hemangioma by Freeny and Marks which are diminished attenuation in non-contrast CT,
peripheral enhancement in dynamic CT and complete iso-attenuating filling of the lesion in delayed scans
[55].
Magnetic Resonance Imaging (MRI)
Hemangiomas appear as hypointense lesions in T1 weighted images and markedly hyperintense in T2
weighted images [56]. If fibrosis is present within the lesion, it appears as areas of hypointensity in a hyperintense lesion [57]. While if there are cystic changes or hemorrhage, it appears as areas of increased
signal intensity compared to the already hyperintense lesion in T2 weighted images [56]. MR imaging has
some limitations even with contrast administration as they cannot consistently differentiate hemangiomas
from some other lesions especially hypervascular malignancies [58].
Differential Diagnosis
On diagnosis of IHHE, there are other rare tumors that need to be excluded. One example is Kaposiform
hemangioendothelioma which has a more infiltrative nature and usually accompanied by Kasabach Merritt
syndrome. Although it presents in older children, undifferentiated embryonal sarcoma should also be
included in the differential diagnosis. Angiosarcoma is another rare diagnosis in infants that should be
included in the differential diagnosis as it can mimic IHHE on imaging.
IHHE should be differentiated from hepatoblastoma that may occur in the same age group. Imaging can
be helpful in differentiating it from IHHE as hepatoblastoma appears heterogenous in T2 weighted MRI
sequence. Other benign lesions that may resemble IHHE include cysts, arteriovenous malformations and
biliary hamartomas [3,26].
Management of IHHE
The treatment of IHHE depends on the clinical presentation and the asociated complications [9]. Since
focal IHHE mostly involutes spontaneously, no treatment is usually needed. In rare cases that are associated
with arteriovenous shunting, embolization may be considered.
Multifocal and diffuse IHHE types are usually symptomatic and often require medical, interventional,
or surgical management. Historically, oral corticosteroids have been the main medical treatment for
problematic multifocal and diffuse IHHE [10]. The efficacy of corticosteroids in terms of stabilization or
reducing tumor size were as high as 75%. The used doses ranged from 2-3 mg/kg/day. Despite all published
reports, there is no standard regimen regarding the optimal dose and tapering regimen for corticosteroids
[10,59]. Treatment with corticosteroids carried many side effects including hyperglycemia, hypertension,
growth retardation, Cushing syndrome and immunosuppression [60]. Even after 2008, when propranolol
was proved highly effective in inducing involution of infantile hemangiomas, many published studies still
used interferon 2 alpha and corticosteroids for treatment of IHHE. Interferon 2 alpha is estimated to
cause spastic diplegia in around 2.5% of infantile hemangioma patients and was also associated with motor
developmental disturbance in another 4.1% [61].
Propranolol, a nonselective beta blocker, dramatically changed the treatment approach since the discovery of
its efficacy in treating infantile hemangiomas. While the exact mode of action of propranolol in IHHE is not
totally clear, multiple hypotheses have been discussed including vasoconstriction, inhibition of angiogenesis,
decreased renin production and stimulation of apoptosis [62-64]. Compared to corticosteroids, propranolol
carried a more rapid and greater response. Several reports demonstrated the efficacy of propranolol (in a
dose of 2-3mg/kg/day) in controlling the proliferation of IHHE [65-67]. Few studies demonstrated the
efficacy of propranolol in combination with corticosteroids in treating IHHE [13,68,69].
The use of propranolol in patients with IHHE has its side effects. These include bradycardia, hypotension,
hypoglycemia, and exacerbation of bronchospasm [67].
Other medical treatments including vincristine and cyclophosphamide have shown various degrees of
success [2,11,69].
Surgical resection and hepatic artery embolization were the main treatment options for IHHE before the
efficacy of medical treatment was proven [12]. Currently, surgery is rarely performed for IHHE and is usually
reserved as a last resort in problematic cases that are refractory to medical treatment. With the refractory
cases specially presenting with abdominal compartment syndrome, a liver transplant may be indicated [13].
Conclusion
Despite the benign nature of IHHE, some cases may require aggressive treatment, especially in multifocal
and diffuse types. Propranolol is considered the golden treatment for IHHE, considering the fewer side
effects it carries compared to the long-term use of corticosteroids. While the treatment of IHHE has much
evolved in the last decade, understanding the nature of IHHE may lead to a revolution in the currently used
treatment modalities. Considering the rarity of the disease, prospective multicentric trials should be the
ultimate goal to reach consensus on the management algorithm of IHHE including imaging techniques,
treatment regimens and doses, the period of follow up and treatment options in recurrence.
Bibliography
- Sari, N., Yalçin, B., Akyüz, C., Haliloglu, M. & Büyükpamukçu, M. (2006). Infantile hepatic hemangioendothelioma with elevated serum alpha-fetoprotein. Pediatr Hematol Oncol., 23(8), 639-647.
- Christison-Lagay, E. R., Burrows, P. E., Alomari, A., et al. (2007). Hepatic hemangiomas: subtype classification and development of a clinical practice algorithm and registry. J Pediatr Surg., 42(1), 62-68.
- Zimmermann, A. (2017). Infantile Hepatic Hemangioma/Hemangioendothelioma. In: Tumors and Tumor-Like Lesions of the Hepatobiliary Tract. Cham: Springer International Publishing, (pp. 937-957).
- Huang, S. A., Tu, H. M., Harney, J. W., et al. (2000). Severe Hypothyroidism Caused by Type 3 Iodothyronine Deiodinase in Infantile Hemangiomas. N Engl J Med., 343(3), 185-189.
- Dickie, B., Dasgupta, R., Nair, R., et al. (2009). Spectrum of hepatic hemangiomas: management and outcome. J Pediatr Surg., 44(1), 125-133.
- Kulungowski, A. M., Alomari, A. I., Chawla, A., Christison-Lagay, E. R. & Fishman, S. J. (2012). Lessons from a liver hemangioma registry: Subtype classification. J Pediatr Surg., 47(1), 165-170.
- Hsiao, K. H., Lin, L. H., Chen, D. F. & Huang, S. H. (2007). Hepatic Mesenchymal Hamartoma Combined with Infantile Hepatic Hemangioendothelioma in an Infant. J Formos Med Assoc., 106(3 Suppl), S1-S4.
- Bejarano, P. A., Serrano, M. F., Casillas, J., et al. (2003). Concurrent Infantile Hemangioendothelioma and Mesenchymal Hamartoma in a Developmentally Arrested Liver of an Infant Requiring Hepatic Transplantation. Pediatr Dev Pathol., 6(6) 552-557.
- Canan Özdemir, Z., Kar, Y. D., Şöhret, N. C., Kebapçı, M. & Bör, Ö. (2017). Beta blocker and steroid therapy in the treatment of infantile hepatic hemangioendothelioma. Drug Discov Ther., 11(3), 161-164.
- Bertrand, J., McCuaig, C., Dubois, J., Hatami, A., Ondrejchak, S. & Powell, J. (2011). Propranolol versus prednisone in the treatment of infantile hemangiomas: A retrospective comparative study. Pediatr Dermatol., 28(6), 649-654.
- Meyers, R. L. & Scaife, E. R. (2000). Benign liver and biliary tract masses in infants and toddlers. Semin Pediatr Surg., 9(3), 146-155.
- Markiewicz-Kijewska, M., Kasprzyk, W., Broniszczak, D., et al. (2009). Hemodynamic failure as an indication to urgent liver transplantation in infants with giant hepatic hemangiomas or vascular malformations - Report of four cases. Pediatr Transplant., 13(7), 906-912.
- Sarıalioğlu, F., Yazıcı, N., Erbay, A., et al. (2017). A new perspective for infantile hepatic hemangioma in the age of propranolol: Experience at Baskent university. Exp Clin Transplant., 15(Suppl 2), 74-78.
- Park, E. A., Seo, J. W., Lee, S. W., Choi, H. Y. & Lee, S. J. (2001). Infantile hemangioendothelioma treated with high dose methylprednisolone pulse therapy. J Korean Med Sci., 16(1), 127-129.
- Drolet, B. A., Swanson, E. A. & Frieden, I. J. (2008). Infantile hemangiomas: an emerging health issue linked to an increased rate of low birth weight infants. J Pediatr., 153(5), 712-715, 715.e1.
- Selby, D. M., Stocker, J. T., Waclawiw, M. A., Hitchcock, C. L. & Ishak, K. G. (1994). Infantile hemangioendothelioma of the liver. Hepatology, 20(1 Pt 1), 39-45.
- Chang, E., Boyd, A., Nelson, C. C., et al. (1997). Successful treatment of infantile hemangiomas with interferon-alpha-2b. J Pediatr Hematol Oncol., 19(3), 237-244.
- Stehr, W. & Guzzetta, P. C. (2012). Nonmalignant Tumors of the Liver. In: Pediatric Surgery, 459-462.
- Jha, P., Chawla, S. C., Tavri, S., Patel, C., Gooding, C. & Daldrup-Link, H. (2009). Pediatric liver tumors--a pictorial review. Eur Radiol., 19(1), 209-219.
- Isaacs, H. (2007). Fetal and neonatal hepatic tumors. J Pediatr Surg., 42(11), 1797-1803.
- Kochin, I. N., Miloh, T. A., Arnon, R., Iyer, K. R., Suchy, F. J. & Kerkar, N. (2011). Benign liver masses and lesions in children: 53 cases over 12 years. Isr Med Assoc J., 13(9), 542-547.
- Emre, S. & McKenna, G. J. (2004). Liver tumors in children. In: Pediatric Transplantation., 8(6), 632-638.
- Daller, J. A., Bueno, J., Gutierrez, J., et al. (1999). Hepatic hemangioendothelioma: clinical experience and management strategy. J Pediatr Surg., 34(1), 98-105, discussion 105-106.
- Moon, S. B., Kwon, H. J., Park, K. W., Yun, W. J. & Jung, S. E. (2009). Clinical experience with infantile hepatic hemangioendothelioma. World J Surg., 33(3), 597-602.
- Kim, E. H., Koh, K. N., Park, M., Kim, B. E., Im, H. J. & Seo, J. J. (2011). Clinical features of infantile hepatic hemangioendothelioma. Korean J Pediatr., 54(6), 260-266.
- Gnarra, M., Behr, G., Kitajewski, A., et al. (2016). History of the infantile hepatic hemangioma: From imaging to generating a differential diagnosis. World J Clin Pediatr., 5(3), 273-280.
- Mortelé, K. J., Vanzieleghem, B., Mortelé, B., Benoit, Y. & Ros, P. R. (2002). Solitary hepatic infantile hemangioendothelioma: Dynamic gadolinium-enhanced MR imaging findings. Eur Radiol., 12(4), 862-865.
- De Paoli, A. G., Williams, M., Parsons, S. J., Long, E., Brothers, L. & Dargaville, P. A. (2007). Massive hepatic congenital haemangioma: clinical dilemmas. J Paediatr Child Health., 43(4), 312-314.
- Bay, A., Öner, A. F., Etlik, Ö., Koseoglu, B. & Kaya, A. (2005). Unusual presentation of infantile hemangioendothelioma. Pediatr Blood Cancer., 44(3), 267-269.
- Davenport, M., Hansen, L., Heaton, N. D. & Howard, E. R. (1995). Hemangioendothelioma of the liver in infants. J Pediatr Surg., 30(1), 44-48.
- Lu, C. C., Ko, S. F., Liang, C. D., Kuo, H. W. & Tiao, M. M. (2002). Infantile hepatic hemangioendothelioma presenting as early heart failure: report of two cases. Chang Gung Med J., 25(6), 405-410.
- Sidwell, R. U., Daubeney, P. E. F., Porter, W. M. & Roberts, N. M. (2004). Neonatal Hemangiomatosis and Atrial Septal Defect: A Rate Cause of Right Heart Failure in Infancy. Pediatr Dermatol., 21(1), 66-69.
- Jothilakshmi, K., Matthai, J., Paul, S. & Singal, A. K. (2006). Symptomatic hepatic hemangioendothelioma in a newborn. Indian Pediatr., 43(10), 908-910.
- Dempers, J., Wadee, S. A., Boyd, T., et al. (2011). Hepatic hemangioendothelioma presenting as sudden unexpected death in infancy: a case report. Pediatr Dev Pathol., 14(1), 71-74.
- Hase, T., Kodama, M., Kishida, A., et al. (1995). Successful management of infantile hepatic hilar hemangioendothelioma with obstructive jaundice and consumption coagulopathy. J Pediatr Surg., 30(10), 1485-1487.
- Jayanthi, V., Shankar, T. R., Ravindran, C., Sudalaimuthu, S. & Chandrasekar, T. S. (2000). Diffuse hepatic hemangiomatosis: case report. Trop Gastroenterol., 21(4), 188-189.
- Gembruch, U., Baschat, A. A., Gloeckner-Hoffmann, K., Gortner, L. & Germer, U. (2002). Prenatal diagnosis and management of fetuses with liver hemangiomata. Ultrasound Obstet Gynecol., 19(5), 454-460.
- Sevinir, B. & Özkan, T. B. (2007). Infantile hepatic hemangioendothelioma: Clinical presentation and treatment. Turkish J Gastroenterol., 18(3), 182-187.
- Naik, A., Rahouma, M., Eldesoki, I., et al. (2018). Anticoagulation in Surgery. 1.
- Hassan, R., Gulati, S., Mahender, Y., et al. (2017). Impact of Low Molecular Weight Heparin on Overall Survival in Patients with Advanced Lung Cancer: A Retrospective Study. Am J Clin Exp Med., 5(5), 173-175.
- Konrad, D., Ellis, G. & Perlman, K. (2003). Spontaneous regression of severe acquired infantile hypothyroidism associated with multiple liver hemangiomas. Pediatrics, 112(6 Pt 1), 1424-1426.
- Balazs, A. E., Athanassaki, I., Gunn, S. K., et al. (2007). Rapid resolution of consumptive hypothyroidism in a child with hepatic hemangioendothelioma following liver transplantation. Ann Clin Lab Sci., 37(3), 280-284.
- Lee, T. C., Barshes, N. R., Agee, E. E., et al. (2006). Resolution of medically resistant hypothyroidism after liver transplantation for hepatic hemangioendothelioma. J Pediatr Surg., 41(10), 1783-1785.
- Smith, A. A. H. & Nelson, M. (2016). High-Output Heart Failure from a Hepatic Hemangioma with Exertion-Induced Hypoxia. Am J Cardiol., 117(1), 157-158.
- Mendiratta, V., Anand, R., Chander, R., Harjai, B. & Gupta, T. (2008). Multiple neonatal haemangiomatosis with liver haemangiomas and anaemia. Australas J Dermatol., 49(1), 42-43.
- Bar-Sever, Z., Horev, G., Lubin, E., et al. (1994). A rare coexistence of a multicentric hepatic hemangioendothelioma with a large brain hemangioma in a preterm infant. Pediatr Radiol., 24(2), 141-142.
- Behr, G. G., Fishman, S. J., Caty, M. G., Kulungowski, A. M., Paltiel, H. J. & Alomari, A. I. (2012). Hepatic mesenchymal hamartoma and infantile hemangioma: A rare association. J Pediatr Surg., 47(3), 448-452.
- Abuhamad, A. Z., Lewis, D., Inati, M. N., Johnson, D. R. & Copel, J. A. (1993). The use of color flow Doppler in the diagnosis of fetal hepatic hemangioma. J Ultrasound Med., 12(4), 223-226.
- Zenge, J. P., Fenton, L., Lovell, M. A. & Grover, T. R. (2002). Case report: infantile hemangioendothelioma. Curr Opin Pediatr., 14(1), 99-102.
- Kassarjian, A., Zurakowski, D., Dubois, J., Paltiel, H. J., Fishman, S. J. & Burrows, P. E. (2004). Infantile Hepatic Hemangiomas: Clinical and Imaging Findings and Their Correlation with Therapy. Am J Roentgenol., 182(3), 785-795.
- Meirowitz, N. B., Guzman, E. R., Underberg-Davis, S. J., Pellegrino, J. E. & Vintzileos, A. M. (2000). Hepatic hemangioendothelioma: prenatal sonographic findings and evolution of the lesion. J Clin Ultrasound., 28(5), 258-263.
- Warmann, S., Bertram, H., Kardorff, R., Sasse, M., Hausdorf, G. & Fuchs, J. (2003). Interventional treatment of infantile hepatic hemangioendothelioma. J Pediatr Surg., 38(8), 1177-1181.
- Bree, R. L., Schwab, R. E. & Neiman, H. L. (1983). Solitary echogenic spot in the liver: Is it diagnostic of a hemangioma? Am J Roentgenol., 140(1), 41-45.
- Itai, Y., Ohtomo, K., Araki, T., Furui, S., Iio, M. & Atomi, Y. (1983). Computed tomography and sonography of cavernous hemangioma of the liver. Am J Roentgenol., 141(2), 315-320.
- 55. Freeny, P. & Marks, W. (1986). Hepatic hemangioma: dynamic bolus CT. Am J Roentgenol., 147(4), 711-719.
- Powers, C., Ros, P. R., Stoupis, C., Johnson, W. K. & Segel, K. H. (1994). Primary liver neoplasms: MR imaging with pathologic correlation. RadioGraphics., 14(3), 459-482.
- Ros, P., Lubbers, P., Olmsted, W. & Morillo, G. (1987). Hemangioma of the liver: heterogeneous appearance on T2-weighted images. Am J Roentgenol., 149(6), 1167-1170.
- Li, K. C., Glazer, G. M., Quint, L. E., et al. (1988). Distinction of hepatic cavernous hemangioma from hepatic metastases with MR imaging. Radiology, 169(2), 409-415.
- Bennett, M. L., Fleischer, A. B., Chamlin, S. L. & Frieden, I. J. (2001). Oral corticosteroid use is effective for cutaneous hemangiomas: an evidence-based evaluation. Arch Dermatol., 137(9), 1208-1213.
- Boon, L. M., MacDonald, D. M. & Mulliken, J. B. (1999). Complications of systemic corticosteroid therapy for problematic hemangioma. Plast Reconstr Surg., 104(6), 1616-1623.
- Barlow, C. F., Priebe, C. J., Mulliken, J. B., et al. (1998). Spastic diplegia as a complication of interferon Alfa-2a treatment of hemangiomas of infancy. J Pediatr., 132(3 pt 1), 527-530.
- Schiestl, C., Neuhaus, K., Zoller, S., et al. (2011). Efficacy and safety of propranolol as first-line treatment for infantile hemangiomas. Eur J Pediatr., 170(4), 493-501.
- Chim, H., Armijo, B. S., Miller, E., Gliniak, C., Serret, M. A. & Gosain, A. K. (2012). Propranolol induces regression of hemangioma cells through HIF-1α-mediated inhibition of VEGF-A. Ann Surg., 256(1), 146-156.
- Manunza, F., Syed, S., Laguda, B., et al. (2010). Propranolol for complicated infantile haemangiomas: A case series of 30 infants. Br J Dermatol., 162(2), 466-468.
- Léauté-Labrèze, C., de la Roque, E. D., Hubiche, T., Boralevi, F., Thambo, J. B. & Taïeb, A. (2008). Propranolol for Severe Hemangiomas of Infancy. N Engl J Med., 358(24), 2649-2651.
- Marsciani, A., Pericoli, R., Alaggio, R., Brisigotti, M. & Vergine, G. (2010). Massive response of severe infantile hepatic hemangioma to propanolol. Pediatr Blood Cancer., 54(1), 176.
- Mazereeuw-Hautier, J., Hoeger, P. H., Benlahrech, S., et al. (2010). Efficacy of propranolol in hepatic infantile hemangiomas with diffuse neonatal hemangiomatosis. J Pediatr., 157(2), 340-342.
- Yeh, I., Bruckner, A. L., Sanchez, R., Jeng, M. R., Newell, B. D. & Frieden, I. J. (2011). Diffuse infantile hepatic hemangiomas: A report of four cases successfully managed with medical therapy. Pediatr Dermatol., 28(3), 267-275.
- Bosemani, T., Puttgen, K. B., Huisman, T. A. G. M. & Tekes, A. (2012). Multifocal infantile hepatic hemangiomas -Imaging strategy and response to treatment after propranolol and steroids including review of the literature. Eur J Pediatr., 171(7), 1023-1028.