Biography
Interests
Dr. Kanika Shanker
Summit Endocrinology, Summit Physician Services, Chambersburg, PA
*Correspondence to: Dr. Kanika Shanker, Summit Endocrinology, Summit Physician Services, Chambersburg, PA.
Copyright © 2018 Dr. Kanika Shanker. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Bone disorders in children can be divided into problems of bone mineralization, density and bone matrix.
It can present with problems in gaining height, fractures, bone deformities and biochemical disturbances in
minerals such as calcium, phosphorus, and hormones -vitamin D and parathyroid hormone.
Methods
References for this review were identified through searches of PubMed, Medline, and Embase for articles
published to July 2018using the terms “osteoporosis, rickets and osteogenesis imperfecta” [MeSH Terms]
OR “bone metabolic disorders” [All Fields] OR “bone disorders” [All Fields]. The reference lists of the
articles thus identified were also searched. The search was not restricted to English-language literature.
Problems in Bone Density
Bone density is a dynamic state in children. It is continuously increasing as children are gaining height and
weight. It is different in comparison to adults, as the peak bone mass is achieved between the second and
third decade of life followed by gradual loss. This loss is more significant in females around menopause as
they have lower bone mass in comparison of males due to decreased thickness of bones. It does not imply
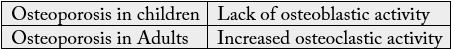
that boys and males do not get osteoporosis. Therefore, osteoporosis in children is more likely due to failure
to gain bone mass. In adult osteoporosis, it is caused by age-related bone mass.
Risk factors for osteoporosis are the history of fractures in the past, use of glucocorticoids, and hyperthyroidism.
Bone density is measured with the help of machine known as Dual Energy X-ray absorptiometry(DXA) [1,2]. It provides a quick estimate of bone mineral density and is considered the gold standard for the assessment of osteoporosis in children as well as well as adults. It does not give any unnecessary radiation exposure to the patient and the technician who is performing it.
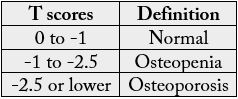
As far as interpretation is concerned, adult standard criterion, reported in T scores for diagnosing low bone density should not be used in children which is reported in Z scores. Using T scores in children will lead to underestimation of bone mineral density and hence over diagnosis of osteoporosis. National institute of Health in USA has developed free online pediatric bone density assessment calculator based on the age and height of child. It provides a handy tool for estimation of pediatric bone density as a Z scores which is standard deviation from the mean.
The first step in the treatment of Osteoporosis in children is ensuring optimum calcium and Vitamin D levels, and adequate physical activity. The most widely used medication for the treatment of pediatric low bone density is an intravenous medication which falls under the category of bisphosphonates. It is a synthetic stable pyrophosphate analogue. Bisphosphonates work by decreasing the bone resorption by binding to the hydroxyapatite crystals of the bone. The two most commonly used medications under this category are pamidronate and zoledronic acid. Zoledronic is an upcoming medication, with less frequency but requires closer monitoring of calcium and phosphorus levels. It is a non FDA approved usage of the medication (off label). It is well tolerated medication but can be used associated with low calcium levels and flu like symptoms, when used first time [4]. Website for bone mineral density z scores in children with height consideration: http:\\www.bmdcspublic.com.
Bone Mineral Problems
The most common problem under this category is Rickets. It refers to the changes at the growth plate
caused by deficient mineralization of bone and occurs before the closure of the growth plates. In adults
it is known as osteomalacia [5,6]. Bone mineral problems are more common in children in comparison
to bone density problems. Rickets occur due to deficiency of Vitamin D, the most common cause,
phosphorus(phosphopenic) and or calcium(calcipenic). The evaluation of a child with clinical signs of rickets
should include a dietary history with attention given to calcium and vitamin D intake, medication history
specially the use of glucocorticoids and anticonvulsants, and a history of sun exposure. There are more clearly
laid out recommendations in children by Institute of Medicine (last came in 2010) and American Academy
of Pediatrics for recommended daily allowances (RDA) for vitamin D and calcium intake. It is diagnosed on
the basis of biochemical finding of calcium, phosphorus, 25 hydroxy vitamin D levels, 1-25 hydroxy vitamin
D levels, parathyroid hormone level, urinary calcium levels and alkaline phosphatase levels. The treatment
is by replacing the calcium, phosphorus and Vitamin D. Oral method of replacement is preferred over
intravenous method of replacement [7].
Bone Matrix Problems
Osteogenesis Imperfecta, is an inherited connective tissue disorder with varied presentations also known
as brittle bone disease. It is caused by problems in the genes controlling the alpha-1 and alpha-2 chains
of type I collagen or proteins involved in posttranslational modification of type I collagen [8]. It presents
with increased bone fragility which presents with fractures, along with short stature, blue colored sclera
and hearing problems. Family history of similar presentations is also important and helpful in making the
diagnosis. If clinically significant, it is treated with bisphosphonates [9].
Conclusion
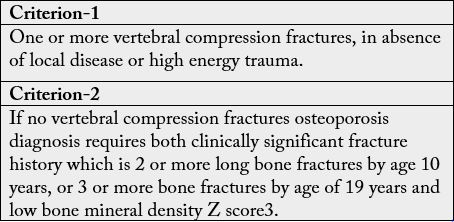
The most important question in the mind of the doctor ordering it, should be its clinical utility in the clinical
management and need for further evaluation. Even the definition of osteoporosis in children gives more
importance to the history of fractures and age of patient rather the absolute value of bone density.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!