Biography
Interests
Muhammed Alsherbeeny, A.1*, Mousa Alhosawy, M.1 , Mohammed Ali, F.2 & Mostafa Almahe, S.2
1Consultant of Orthopaedics and Lower Limb Reconstruction Surgery, Department of Orthopaedics Surgery and
Traumatology, King Salman bin Abdelaziz Medical City, Saudi Arabia
2Senior Registrar of Orthopaedics and Trauma Surgery, Department of Orthopaedics Surgery and Traumatology,
King Salman bin Abdelaziz Medical City, Saudi Arabia
*Correspondence to: Dr. Muhammed Alsherbeeny, A., Consultant of Orthopaedics and Lower Limb Reconstruction Surgery, Department of Orthopaedics Surgery and Traumatology, King Salman bin Abdelaziz Medical City, Saudi Arabia.
Copyright © 2022 Dr. Muhammed Alsherbeeny, A., et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Peroneus longus tendon can be used for revision anterior cruciate ligament reconstruction cases. The choice of the graft is one of the most challenging steps in the revision of the anterior cruciate ligament. An alternative autograft option with less donor site morbidity and adequate strength should be planned, especially in revision cases, which directly impact on rehabilitation programs and fast return to preinjury status. Peroneus longus tendon was the graft of choice.
A case of soccer player with right knee instability after contact injury is presented here. The patient underwent bilateral ACL reconstruction; the right knee was two years, and the left was three years ago, using an ipsilateral hamstring autograft. Right knee ACL graft rupture due to rotatory instability of the knee due to the vertical femoral tunnel. Assessment of knee pain and stability is used to measure the outcome. The donor site showed no complication on follow-up. The results showed advantageous recovery with excellent objective and subjective results.
The use of the International Knee Documentation Committee and the American Orthopedic Foot and Ankle Score to evaluate the postoperative biomechanical outcome. Satisfactory with the potentially favorable outcome when using ipsilateral peroneus longus tendon graft, which is superior and comparable to other graft options in revision cases of anterior cruciate reconstruction.
The peroneus longus tendon graft is a reasonable option in revision anterior cruciate ligament reconstruction cases without any significant postoperative morbidity regarding the donor site.
Introduction
In anterior cruciate ligament (ACL) reconstruction, few studies have described the use of peroneus longus
tendon (PLT) graft. However, the PLT autograft is described in many orthopedics surgeries, including
spring ligament reconstruction, deltoid ligament reconstruction, and medial patellofemoral ligament
reconstruction [1,2]. Studies describe that the peroneus brevis is the main evertor of the ankle; the use of
the PLT graft will not affect the ankle joint function [3]. Harvest of the PLT will not lead to any injury
to the knee joint [4]. Although the patellar tendon graft is commonly used in revision ACL surgery, it
causes chronic anterior knee pain [5]. ACL reconstruction surgeries increased on the last 20 years [6]. As
the primary reconstruction increased, the number of revision ACL reconstruction cases increased up to
13.3% of all primary ACL reconstruction surgery [7]. In revision ACL reconstruction, the knee joint will be
exposed to the third hit, the first hit is the knee injury, the second one is the arthroscopic reconstruction and
graft harvesting from around the knee joint. Harvesting the graft for reconstruction of the ACL away from
tendons around the knee joint will minimize the knee injury due to the second hit, which will positively
impact the outcome of reconstruction surgery.
Moreover, avoiding harvesting the hamstring tendon in the primary ACL reconstruction will faster the rehabilitation program as no added injury to the muscle, which will decrease the pain at the donor site. The graft options available for reconstruction of ACL are Hamstring tendon, bone-patellar tendon-bone (BPTB) and quadriceps tendons (QT) [8,9].
Each one of the options tendon graft available for ACL reconstruction has advantages and disadvantages. However, all are similar in causing more knee injuries as the graft harvesting from around the knee joint. Studies showed complications like patellar fracture, chondromalacia patellae and chronic anterior knee pain with BPTB graft, quadriceps weakness, and kneeling pain with QT graft [8,10,11]. In revision cases of ACL reconstruction with the previous hamstring tendon harvesting, the choice between patellar tendon and quadriceps tendon will add more injury to the knee. In view of the above, the choice of the PLT graft for ACL reconstruction will avoid the third hit to the knee and decrease postoperative knee pain, increasing patient satisfaction and faster rehabilitation. Many studies support the use of PLT graft for ACL reconstruction without donor site morbidity [12].
The patient presented to our clinic with the main complaint of right knee pain and instability; pain increased
with activities. Three years earlier, the patient had a history of a twisting knee injury while playing soccer.
The patient underwent bilateral ACL reconstruction; the right knee was two years, and the left knee was
three years ago using an ipsilateral hamstring autograft. There is no history of a medical condition and
irrelevant family medical history. Lachman’s, anterior drawer, and pivot shift tests were positive on physical
examination. Plain radiographs revealed normal knee. Magnetic Resonance Imaging (MRI) confirmed the
diagnosis of a complete tear of the ACL graft. We discussed with the patient for revision ACL reconstruction
using PLT autograft from the ipsilateral.
Surgical Procedure
We obtained the graft from the ipsilateral PLT by making a 2cm longitudinal incision over the posterior
border of the lateral malleolus. The skin incision was 1.5cm posterior to the posterior border of the distal
fibula and about 3cm proximal to the tip of the lateral malleolus [Figure. 1]. We identified the superior
peroneal retinaculum, the peroneus longus, and peroneus brevis tendons. The peroneus brevis was deep and
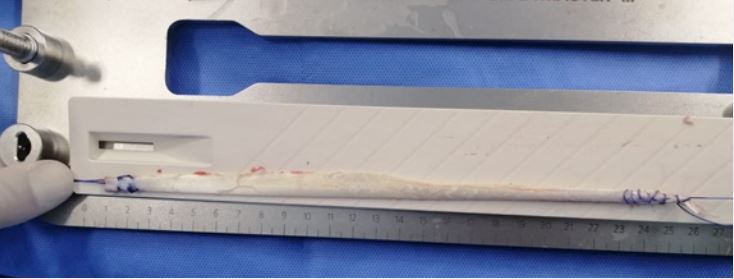
had a tiny fleshy attachment along its posterior aspect. Suturing the distal part of the PLT [Figure. 2,3].
The distal stump was sutured to the peroneus brevis tendon. To prevent peroneal nerve injury, we release the
tendon of peroneus longus about 5cm distal to the head of fibula using the tendon stripper [Figure. 4,5]. A
double-fold graft was about 8.5mm in diameter and 13cm in length in this patient [Figure. 6].





Diagnostic arthroscopy confirmed the diagnosis of the rupture ACL graft. We performed preparation and
drilling on ACL footprint on both the femoral and tibial sides for the femoral and tibial tunnels. The
double-fold graft was inserted and fixed through the femoral and tibial tunnels using EndoButton for the
femur side fixation and a screw for the tibia side.
Immediate postoperatively, we applied a knee immobilizer at 0º
extensions with a gradual increase in
the flexion range to 90º
by the first week post-surgery. The patient was discharged on a knee brace the
following day and started active and passive motion exercises. The outcome was evaluated using the visual
analogue pain scale, International Knee Documentation Committee, and American Orthopedic Foot and
Ankle scores. The follow-up results in favorable recovery with improvement in all objective parameters.
The pain was absent at the 7-month postoperative. At 9-months of postoperative, the International Knee
Documentation Committee score was 100%. The American Orthopedic Foot and Ankle score was 100%
at 10 months postoperative. The patient clinical examination of the ankle was normal with absent of any
graft site morbidity. Ankle eversion and plantar flexion were normal. The patient knee examination showed
a negative Lachman’s test, anterior drawer test, and pivot shift test.
Discussion
With an increasing number of ACL reconstruction surgery cases, there are increased cases of revision
surgeries. Choice of the graft is a crucial factor in avoiding reinjury and redoing surgeries. Graft type is the
most critical step in preoperative planning, especially the revision cases.
Tendon grafts are commonly used in many reconstruction procedures in orthopaedics. In ACL surgery, autograft are always preferred. Semitendinosus, gracilis and patellar, quadriceps tendons are the familiar sources for autograft [9].Patellar bone graft is commonly associated with anterior knee pain, chondromalacia patellae, patellar fractures, and quadriceps muscle weakness, affecting the rehabilitation programs and early return to sports activity [10,11].
This is a case of revision ACL reconstruction. Both hamstrings are harvested for primary ACL reconstruction; to avoid knee joint complications result from patellar tendon graft harvesting, PLT graft has been the best option as an autologous bone graft with the advantage of avoiding a secondary injury in the knee region. In revision ACL reconstruction, avoiding a second hit to the knee will facilitate a rehabilitation program with a favorable range of motion outcomes. In this case, the PLT was harvested as a graft for reconstructing the ACL. The graft diameter was 8.5mm, which was reasonable enough for reconstruction.
Many studies supported PLT for the reconstruction of ACL due to its length and diameter. Several studies support a favorable outcome without any donor site morbidity, including ankle stability, motor power, and gait assessment. Because of the above, PLT is an excellent autograft choice in reconstruction surgeries [12]. PLT graft can be the graft of choice in reconstructing the medial patellofemoral ligament and ACL [2].
There are controversies about the suitable graft size for the reconstruction of the ACL. Some studies support graft size not less than 7 mm to prevent future failure [13]. While others document a diameter of at least 8 mm for the suitable graft size [14,15].
The main concerns about reducing the strength of eversion and plantar flexion if a PLT graft is taken, which will cause ankle instability. Some studies state that harvesting the PLT will not affect the ankle function, eversion, or first ray plantarflexion [16,17]. Harvesting the PLT will not affect the motor power of the ankle eversion [17,18].
According to the situation, a PLT graft was chosen as the patient had previous bilateral knee ACL reconstruction with bilateral semitendinosus tendons harvesting. The option to harvest the patellar tendon as a graft is associated with the complication as mentioned earlier and impact on the patient knee. So, we discuss the option of a PLT graft for revision ACL reconstruction with the patient [19].
Conclusion
PLT is a promising graft in revision ACL reconstruction cases. It is considered one of the promising options
for grafts in revision ACL reconstruction without any donor site morbidity. Long-term studies to evaluate
the optimal function and stability of the knee are still needed.
Funding
This research did not receive any grant in the public, commercial, or not-for-profit sectors.
Ethical Approval
Ethical approval was not required in managing the patients in this report.
Consent
Written informed consent was obtained for publication of this case report. A copy of the written consent is
available for review on request.
Declaration of Competing Interest
The authors report no declarations of interest.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!