Biography
Interests
Yousef Turkistani, A.*, Yousef Alghamdi, Fahad Attar G. & Faiz Felemban
Department of Musculoskeletal, International Medical Center, Jeddah, Kingdom of Saudi Arabia
*Correspondence to: Dr. Yousef Turkistani, A., Department of Musculoskeletal, International Medical Center, Jeddah, Kingdom of Saudi Arabia.
Copyright © 2021 Dr. Yousef Turkistani, A., et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background
The Extensor Mechanism disruption is a very rare yet unforgivable complication of a Total Knee Arthroplasty
(TKA), the incidence of Extensor mechanism disruption from quadriceps tendon is ranged between 0.1% to
1.1%, and the patellar tendon rupture range between 0.17% to 1.4% regardless the cause of the disruption
[1].
No specific nor clear way to treat, and many reports about similar cases showed unfavorable outcomes.
We are presenting this technique with a very satisfying outcome for the patient and the surgeon.
Summary
A 68-year-old lady, diabetic and hypertensive both controlled on medications, active, housewife. She has
bilateral knee pain left more than the right, progressing over years.
Diagnosed with advanced knee osteoarthritis, underwent a left total knee arthroplasty, complicated with iatrogenic injury to patellar tendon at the level of the inferior tip of the patella.
A repair technique using Gracilis for the repair as advancement for the remnant of the patellar tendon.
Case Presentation
A 68-year-old woman, diabetic, and hypertensive, both controlled on medications, housewife, active,
complaining of left knee pain progressed over years, with difficulty climbing stairs and going downstairs.
No history of recent trauma, and no clear history of a previous knee injury.
On examination, she has normally aligned knees bilaterally, left knee has tenderness over the medial joint line, positive grind test for patellofemoral joint pain.
The range of motion of the left knee is measured with a goniometer, extension -3 flexion 120 degrees.
No ligamentous instability, negative anterior drawer, posterior drawer, Lachman, and stress valgus and varus tests.
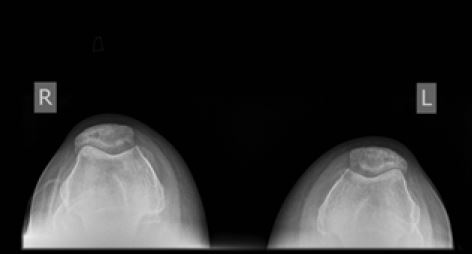
X-rays of the patient showed advanced osteoarthritis of the left knee (Figure 1- 3).


Conservative management failed to improve her complaint.
Underwent left total knee replacement for symptomatic advanced osteoarthritis. The surgery was performed through a midline skin incision and sub-vastus approach. A cruciate substituting posterior stabilized, cemented implant. The patella was everted, and patella resurface was done during the surgery, patellar remnant depth is almost 17mm.
During the approach, while doing the dissecting, unintentionally the patellar tendon was injured at the level of the lower pole by the cautery, almost 5mm below the lower patellar pole.
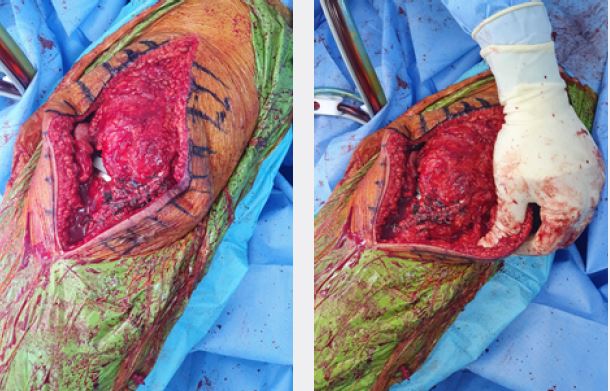
So, after the total knee replacement implantation of the prosthesis was done, we proceeded with the repair of the patellar tendon with reinforcement using a Hamstring graft. 2 bony anchors were put in the inferior pole of the patella, Proximal patellar tendon was then sutured using the bony anchors onto the inferior pole of the patella. After that, reinforced using 2 Ethibond sutures. Hamstring graft harvested both Gracilis and semitendinosus.
These were prepared and whip stitched and measured, a diameter of 6mm with adequate length was achieved.
Using a drill pit of 6mm, a central drill hole was done in the center of the patella superior to the button with the adequate bone stock still available.
Hamstring graft was pulled through.
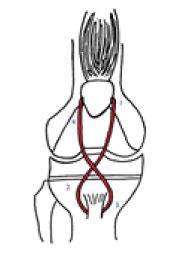
The tibial tuberosity was drilled with a 6mm drill pit and pulled the graft through in a figure-of-eight on top of the patellar tendon, tightened and secured with an interference screw (figure 4).
Then stitched the graft down on the tendon for reinforcement. Adequate repair and fixation achieved (figure 5 & 6), and knee full extension and near full flexion without any problems of the repair. And a stable patella.
Irrigation and closure were done after the insertion of a drain.
The patient put in a hinged knee brace with full extension and 30-degree flexion for 2 weeks, then increased to 60-degree flexion for another 2 weeks, 90-degree flexion for 2 weeks more, then removed the brace.
The patient was allowed and able to put full weight-bearing day 1 post-operatively. Post-operative x rays are accepted (Figure 7 & 8).


The patient’s first visits and follow-up after 2 weeks showed healed wound and staplers’ removal with no complications, pain is tolerable.
Weak extension and the brace in 30-degree flexion, flexion increased to 60-degree, physiotherapy for strengthening of the quadriceps encouraged.
The next follow-up, 2 weeks after, the patient was able to do a full extension on her own, and flexion down to 70 degrees with no brace, she is using the walking cane, pain is much better, the brace set to 90-degree flexion, and re-applied for another 2 weeks.
2 weeks later, the patient is walking normally and able to do a full extension on her own with flexion of more than 110 degrees. With very little pain on rare occasions.
8 weeks follow-up visit showed very stable knee and no complain, with full extension and flexion to 120-degree, the patella is stable.
3 months follow-up visit patient is happy, full range of motion, no ambulatory support with no complaints.
Discussion
Extensor mechanism disruption is a serious complication with TKA, luckily it is very rare. A patellar tendon
injury can happen intraoperatively due to multiple reasons, injury while taking bone cuts, injury while doing
the approach or post-operative due to trauma, soft tissues’ condition, and infection [2]. Different options
are available for these injuries such as immobilization, direct primary repair alone by suturing or wiring,
primary repair with grafts - biologic or synthetic - or allograft reconstruction of the disrupted extensor
mechanism [1,2]. No study suggests the gold standard technique and the results are different between the
patients. Many factors can affect the treatment, such as the general health condition, patients’ demands, the
level of disruption, functional affection, acute or chronic injury, and appropriate donor site tissue for direct
primary repair or augmentation [3]. Therefore, preventing an injury to the extensor mechanism is always
preferable. When you have an intraoperative rupture of EM, direct repair at this stage is of more benefit.
Dobbs et al. [4] assessed 18 patients operated by the direct repair of the extensor mechanism for patellar
tendon rupture after TKA, summarized that variety of results associated, only 25% of the patients having a
satisfying outcome.
To determine if the augmentation is strong enough, direct under-vision examination of the repair strength under stress with a range of motion and in rest. With primary repair, Autogenous graft augmentation provides normal collagen tissue to strengthen the repair tissue [5]. This can be used in patients with connective tissue diseases, infection, and previously operated knee with prosthesis. Different origins of Autogenous tissue graft can be used such as Hamstring -semitendinosus and Gracilis tendon, fascia lata free graft, Plantaris tendon graft, or Achilles tendon - gastrocnemius muscle flap.
The Hamstring graft can be placed over the patellar tendon, passing through a canal drilled in the patella using different techniques, and then sutured back on itself with proper tension. Using Achilles tendon or extensor mechanism allograft in TKA with disrupted EM is of benefit when autografts are mechanically insufficient and structurally inadequate to function. However, it is difficult to have these allografts in most of the centers. Other issues include graft rejection, the transmission of different diseases, and graft strength.
Burnett et al. [6,7] reported a good outcome after the use of an extensor mechanism allograft to reconstruct a disrupted extensor mechanism in patients with a previous total knee replacement. Crossett et al. [8] used Achilles’s tendon allograft to repair on disrupted extensor mechanism, satisfying results as improved walking and decreased extensor lag (was 44 preoperatively to 3 postoperative). In full extension, Tensioning the allograft is an essential factor to success as per Burnett et al. [7]. A protected and controlled knee flexion post-operative in hinged knee brace as in non-TKA patients who has patellar tendon injury.
Synthetic grafts and artificial ligaments allow good load sharing to the tissues in early phases post-operative and promote healing. It also prevents complications of the autograft such as donor site morbidity, although there is a risk of increased infection rates. Some authors preferred the reconstruction with wire cerclage and\ or metal fixation to allow early rehabilitation, but it has the disadvantage of intervention for implant removal later on.
In our case, the primary repair was the best choice as the patient’s overall health is good and her grafted tendons were strong when prepared intraoperative, and how stable the fixation was in the examination after securing.
Our method is recommended for such iatrogenic ruptures as it gave marvelous results.
Take Home Messages
- “Prevention is better than cure”. Take your time and try to prevent as much as possible of complications.
- Every patient must be treated individually, no perfect matches in all cases.
- Knowing what are the options that are available in your institute will help in taking decisions.
- It is always a great idea to take an expert opinion and to discuss with your colleagues, patients’ safety is the
priority [9-11].
Conclusion
EM disruption is rare. Acute rupture is better to be treated in a primary tendon reconstruction. No single
method is correct, evaluate the patient as a whole, then proceed with what is the best for them.
We found that this method in primary repair with the treatment plan such as the controlled flexion and the
good physiotherapy to give very satisfactory results to the patient and the surgeon.
Ethics Approval
International Medical Center and The Research Center.
Consent
Informed written consent signed by the patient
Funding
None.
Conflict of Interest
The authors declare no conflicts of interest, financial or otherwise.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!