CPQ Orthopaedics (2021) 5:3Mini-Review
Melatonin and Osteoporotic Bone
Ray Marks
Department of Health and Behavior Studies, Columbia University, Teachers College, New York, NY 10027, USA
*Correspondence to: Dr. Ray Marks, Department of Health and Behavior Studies, Columbia University,
Teachers College, New York, NY 10027, USA.
Copyright © 2021 Dr. Ray Marks. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 24 May 2021
Published: 31 May 2021
Keywords: Aging; Bone; Bone Regeneration; Melatonin; Osteoporosis; Prevention; Treatment
Abstract
Poor bone quality which persists in heightening premature disability and possibly death rates among
older adults, appears linked to possible deficits in the hormone melatonin. This overview focuses
on the possible link between melatonin and bone health, especially among those affected or at risk
for osteoporosis. Reviewed are relevant topical articles and past literature and research on these
topics located in the PUBMED, GOOGLE SCHOLAR, and SCIENCE DIRECT data base,
with a focus on those published between 2016 and 2021 using the keywords: melatonin and bone,
melatonin and osteoporosis, melatonin and bone regeneration. Results show melatonin can influence
bone metabolism favorably through different mechanisms, but its application in the clinical sphere
is only studied very sparsely. Given the immense burden of osteoporosis, and favorable preclinical
as well as clinical findings, more effort to examine melatonin in the clinical sphere is strongly
advocated.
Background
A wealth of literature shows older adults are at high risk for osteoporosis, a debilitating bone disease,
associated with multiple adverse costly health care outcomes, regardless of country of origin [1-3]. Strongly
associated with high hospitalization usage and costs, premature disability, and even death [4], osteoporosis characterized by low bone mass and micro architectural deterioration of bone tissue, with consequent
increases in bone fragility and susceptibility to fracture, remains a relatively intractable highly significant
health concern in the context of aging societies in all parts of the globe [5,6], especially among women
[7], and those with various comorbid health conditions such as diabetes, and kidney disease, plus those
dependent on steroid usage [2]. At the same time, research has shown that certain anti-resorptive and
anabolic pharmacologic agents such as denosumab, teriparatide, abaloparatide, romosozumab, and selective
estrogen receptor modulators are said to mitigate age associated bone loss, while limiting bone degeneration
[2,8], even though there may be unwanted side effects and economic costs among some older adults that
warrant attention [9]. Another related body of research shows aging and its impact on sleep among other
factors may be implicated in bone changes with aging that leads to bone fragility [6], thus drugs alone may
not be helpful if sleep has a bearing on bone health.
However, even though additional non pharmacologic bone density preventive programs do exist in efforts
to stave off excess age associated bone losses, and attain more efficacious health outcomes than presently
prevail among those adults at risk for osteoporosis [8], the hormone melatonin, a multifunctional amine
based signal molecule released by the pineal gland in synchrony with circadian light/darkness, sleep/wake
daily cycles, as well as by other tissues [2, 5,10] that has possible anabolic, anti-resorptive and antioxidant
bone impacts [11-16] is not commonly listed in either the pharmacologic or non pharmacolic bone loss
mitigation related studies described for older adults.
Yet, based on the rational provided by Sanchez-Barcelo et al. [7], melatonin, which plays a regulatory role
in many physiological processes, including bone physiology, appears to have consistent bone building effects
that appear highly relevant for preserving bone mass in older adults who commonly experience a decline in
the efficacy and production of melatonin as they age, a process that closely parallels any age-related loss of
bone mass.
To examine whether there is a basis for more intense study of this issue in the realm of efforts to effectively
prevent excess osteoporosis disability a scoping review and scan of the relevant literature was duly conducted.
Of specific interest was whether: Bone metabolism and melatonin are related in a clinically relevant way
as indicated many years ago by Li et al. [14], as well as by Susuki et al. [15], along with Sandyk et al. [16],
among others [17-19], such that older adults who may either be at high risk for osteoporotic bone loss, or
deficient melatonin production and functional deficits, or both, may yet be more likely than not to benefit
from appropriate supplementary applications of this hormone.
As outlined by Whitt-Enderby et al. [17] whereas recent therapies to offset osteoporotic bone pathology that
include targeting bone‐resorbing osteoclasts by use of bisphosphonates, estrogen, and calcitonin to prevent
further bone breakdown, these approaches remain limited because they do not result in bone formation as
is necessary in cases of individuals suffering from severe osteoporosis. Another drug that does stimulate
bone‐forming osteoblasts (namely, teriparatide) is however, limited in its usage to a two year period and is
expensive and not without risk.
Alternately, due to established links between bone and melatonin, melatonin has been discussed as well as
advocated as a therapeutic agent for purposes of the prevention and treatment of osteoporosis, as well as its
potential for influencing bone regeneration [18,19].
Since bone loss and subsequent bone injury are enormous health concerns among the older adult populations,
and osteoporosis is not readily susceptible to interventions that safely build bone, it appears important to
explore all innovative approaches in this respect, including melatonin [13,14].
Methods
To derive a fair conclusion concerning melatonin and osteoporosis bone health, an effort was made to
examine all relevant findings published in the peer reviewed literature, and located at the PUBMED
database, followed by a supplementary search on GOOGLE SCHOLAR and SCIENCE DIRECT to
identify any additional relevant materials published in the English language as full length articles, with a
focus on those published predominantly over the time periods 2016-2021. As well, bibliographic resources
were examined if they pertained to the present topic. All items that discussed either some aspect of the
current topic of interest either independently or combined, were deemed of interest to report on and were
duly examined in depth.
The search was limited however, by excluding studies detailing the link between melatonin and many health
issues such as cancer, conference abstracts, preprints, studies on dental or prosthetic implants, oral health,
adolescent based studies, and those that did not directly address the current topics. All forms of study or
reports were deemed acceptable if they appeared to address one or more items of specific present interest.
After examining the data, it was decided that in light of its diverse study approaches that were largely
conducted in the lab, only a narrative overview of what has emerged to date was likely to prove valuable,
although readers may want to examine a prior systematic review by Bao et al. [20]. However, even then,
the current review does not discuss the varied experimental approaches studied in detail, nor the metabolic
pathways and cell receptors and genes receptors that potentially link melatonin effects and bone structure
and physiology. This review also does not question of the validity of the various experimental models that are
the focus of the prevailing body of research. The role of melatonin in post surgical bone healing processes is
also not covered. Here readers can refer to Oryan et al. [21].
Results
As extracted from the relatively modest volume of potentially relevant publications listed using the key terms:
melatonin and osteoporosis, the literature on this topic, which goes back as far as 1894 for osteoporosis with
93,481 independent listing, and 1958 for melatonin with 27, 912 listings as of May 19, 2021, the combined
themes only began to be published in combination in 1992. After that, the publications were quite limited
when compared to the total numbers of theme based publications, and included a total of 113 articles, with
only 56 items listed between 2016-2021, and with the vast majority of these being preclinical in vitro or in
vivo studies or studies that had no immediate relevance to osteoporosis. For example, some focused on bone
in adolescents, while others focused on melatonin and its promise for oral health and dental care purposes.
However, despite the paucity of clinical studies discussing osteoporosis and melatonin effects directly, the search revealed linkages between possible causes of osteoporosis in later life and independent melatonin
associated examples of favorable findings in the research that were downloaded if they appeared to hold
promise in the future for being drawn on in the context of preventing, mitigating or averting some forms of
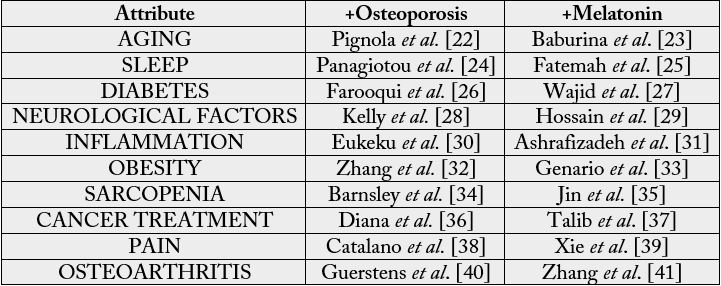
osteoporosis among the elderly successfully and safely. To this end, ten evidence-based possibly preventable
key osteoporosis determinants, along with evidence of melatonin benefits as regards these, are depicted
below in Table 1 to provide a snapshot of possible unexplored melatonin usage in the fight against premature
and excessive bone loss in the elderly.
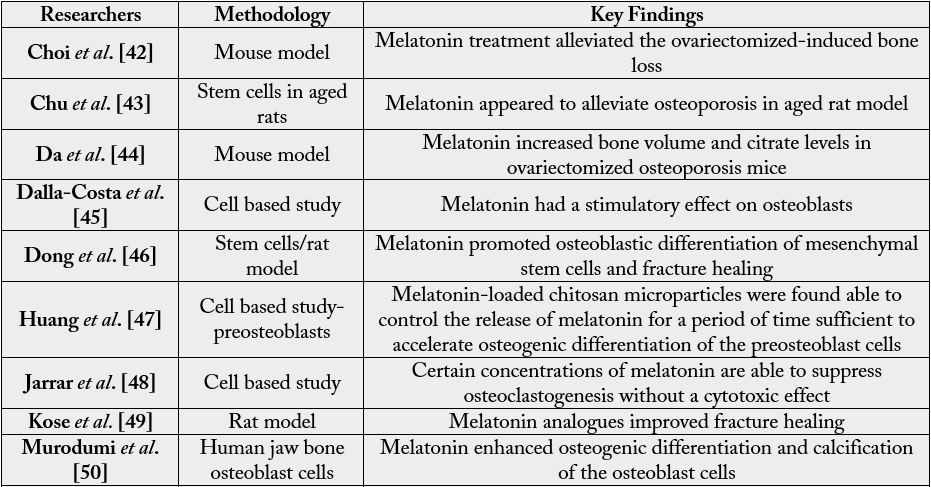
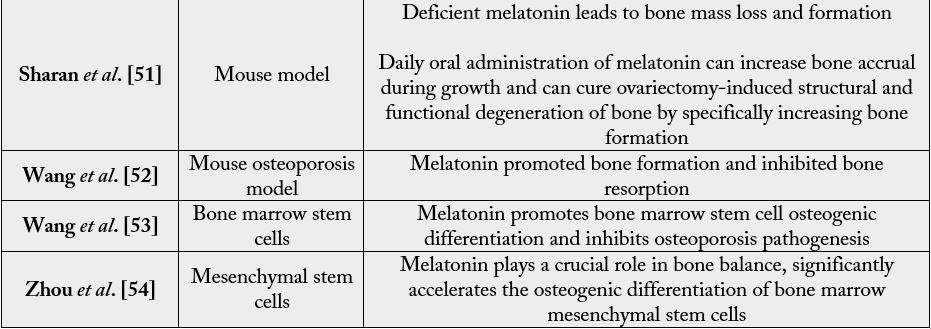
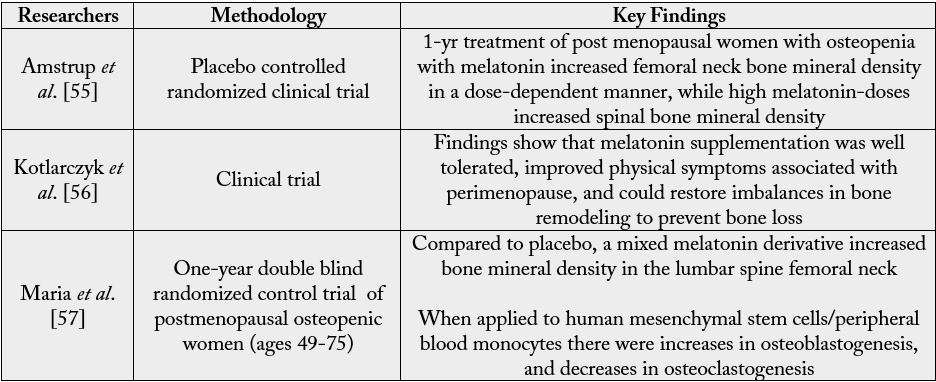
In addition, parallel research implying a favorable independent role for melatonin on bone structure that
might be harnessed in the future to offset the disease more effectively than is presently the case is shown in
Tables 2 and 3.
Table 1: Table Showing Examples of Key Osteoporosis Determinants and Parallel Research of a Favorable
Melatonin Impact On These Attributes
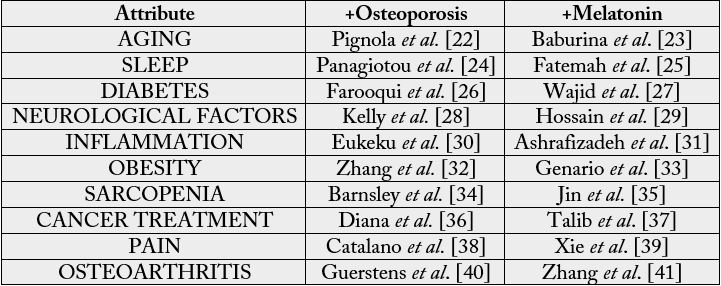 Table 2: Showing Representative Preclinical Research Findings Concerning Melatonin and Bone
Table 2: Showing Representative Preclinical Research Findings Concerning Melatonin and Bone
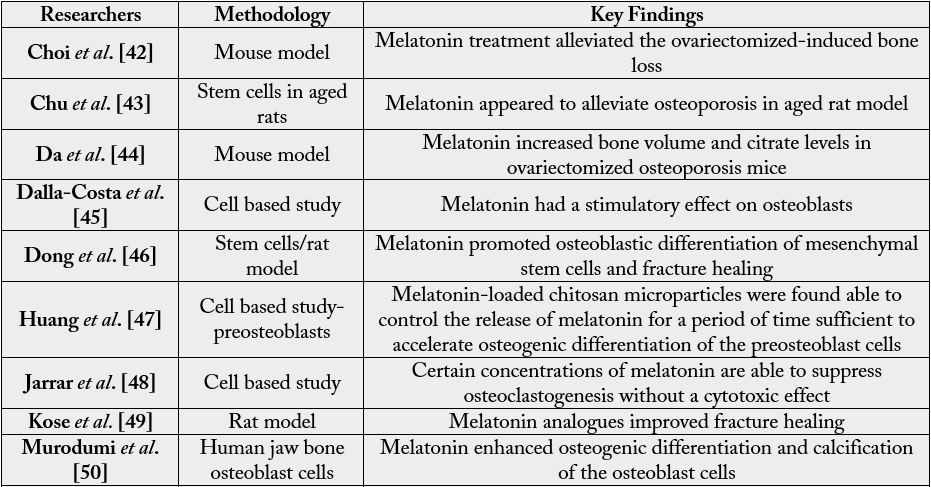
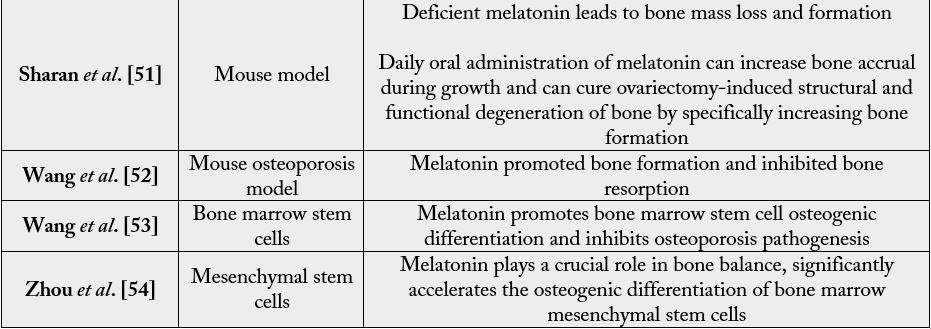 Table 3: Showing Representative Clinical Research Findings Concerning Melatonin and Bone
Table 3: Showing Representative Clinical Research Findings Concerning Melatonin and Bone
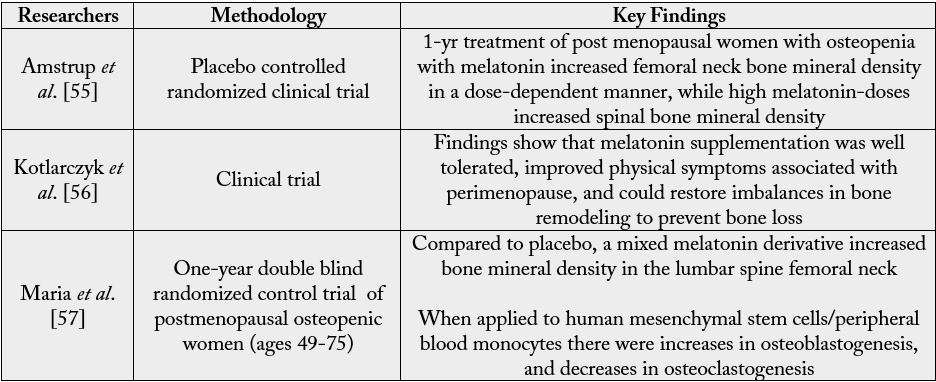
In sum, as outlined in Tables 1-3, which represents a high percentage of available publications listed on
PUBMED, SCIENCE DIRECT, and GOOGLE SCHOLAR over the time periods of 2016-2021 when
most of the research in this area has been conducted, we concur with Liu et al. [5] as well as Li et al. [13] that
while conventional anti osteoporosis medicines can inhibit bone loss, melatonin has the potential to suppress
bone loss, as well as promote new bone formation via a set of complex metabolic pathways that are consistent
with its ability to favorably mediate the osteoporotic bone environment, especially in cases where melatonin
production is deficient [58]. That is, even in the face of the pathophysiological process underpinning the
development of osteoporosis, where there is an imbalance, or uncoupling, of bone formation and resorption
with a net loss of bone [6], melatonin seems to have the potential to minimize or reverse these pathological
processes. In addition, it is clear from the literature that both aging as well as many health conditions, for
example diabetes, that prevail among older adult populations are possible secondary osteoporotic mediators
in their own right that could be targeted to minimize osteoporosis disease manifestations by employing
melatonin based intervention approaches.
Key independent or collective benefits of melatonin as far as bone health is concerned include it ability to:
Increase osteoblast differentiation
Decrease oxidative stresses
Inhibit osteoclastgenesis
Act as an antiinflammatory
Regulate metabolism
Protect mitochondria [14,59,60]
Discussion
Osteoporosis, a widespread generally chronically disabling and serious bone disease, with few remedial
approaches to mitigate this, continues to prove costly and an immense burden among older adults and aging
populations. Strongly associated with fragility fractures, and frailty, as well as pain, and limited mobility, ample
research indicates that the disease may not be inevitable in all cases. Moreover some degree of palliation is
possible through a combination of pharmacologic and non pharmacologic strategies.
At the same time, in view of their limited efficacy, and the findings of a strong linkage between the endocrine
hormone melatonin, studied in many health spheres for many years, and bone metabolism, this hormone appears to hold great promise as a possible small molecule that could be used favorably in a supportive role
the field of bone regeneration and bone disease treatment prevention, given its observed ability to foster
bone repair in an osteoporotic model [58], while inhibiting the differentiation of osteoclasts directly by
suppression of the NF-κB signaling pathway [48].
As outlined almost 20 years ago in the clinical realm, and supported in this review by data in Tables 1-3,
Ostrowska et al. [61], who observed secondary changes in melatonin to impact bone metabolism in a manner
commensurate with postmenopausal osteoporosis implied there is a strong basis for continuing to examine
this hormone [62]. As such, Della-Costa et al. [45] have similarly argued that melatonin does appear to
play a role in the homeostasis of bone metabolism and can be shown to be an important mediator of bone
formation and stimulation [59,63]. Moreover, it has multiple therapeutic effects [23], and there appears
to be a dose related response when applied as far as producing favorable protective and regenerative bone
impacts [60].
Chen et al. [64] too who confirmed that postmenopausal osteoporosis, one of the most common bone
diseases affecting millions of aging women, and where reduced osteogenesis and increased oxidative stress
have been implicated in the pathogeneis of osteoporotic bone marrow mesenchymal stem cells may be
favorably impacted by the administration of melatonin as a preventive as well as an intervention strategy as
discussed by Bao et al. [20] and Sanchez-Barcelo et al. [7]. Alternately, a negative cycle of events is likely as
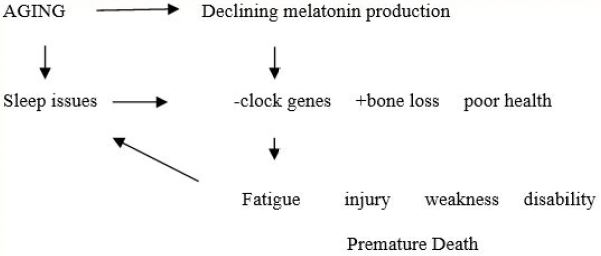
outlined in Figure 1 if no due course of action is forthcoming.
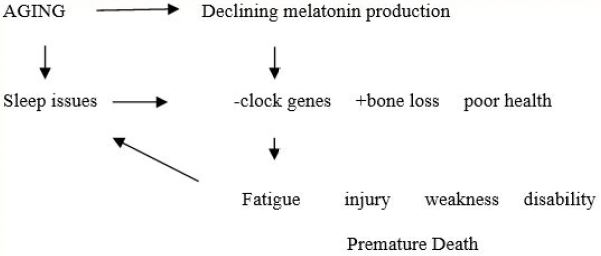
Adapted from: [6,14,65,66]
Figure 1: Hypothetical interactions of aging, bone loss, melatonin, and osteoporosis in the context of older adults
On the other hand, this ability of melatonin to regulate the metabolism of both bone in cases of osteoporosis
and older age [67], as well as the ability to promote bone formation and prevent bone resorption via several
mechanisms, which include the increase in the osteoblastic activity and differentiation, as well as the reduction
in orthoclastic differentiation and activity, and by increasing osteoprotegerin expression and scavenging the
free radicals responsible of bone resorption [7] appears to offer a safe and effective alternative to oftentimes restricted drug usage and exercise interventions. Moreover, melatonin is effective for improving bone
strength even in an aging model [68]. The additional fact that melatonin can be applied or delivered locally
to avoid systemic drug effects [69], tentatively increases its possible value in the realm of efforts to develop
efficacious bone preserving and building interventions in later life even if melatonin is rarely mentioned
in the osteoporosis literature as a potentially highly relevant albeit overlooked etiologic factor in the onset
and progression of postmenopausal as well as senescent and secondary osteoporotic situations. Its role in
fostering bone regeneration and prosthetic stability post-surgery, while not discussed here, also appears
highly promising and should be explored further [69].
Until then, while firm conclusions cannot be made on the basis of the almost sole publication of laboratory
based non human studies, the possible application of melatonin as an early bone building substrate among
osteopenic cases, as well as those in later life must largely remain theoretical, in spite of its promising
attributes. Given the large anticipated decline in this hormone with aging, as well as in cases where sleep
is of poor quality and neurological factors prevail that impair pineal gland function, why there are so few
clinical studies to date in this realm is unclear, but does appear of high value to explore. Moreover, since there
are also few negative studies at present, examining whether this reflects the reality or publication bias and is
an artifact should be further investigated and as cited in 2003 by Cardinali et al. [60] melatonin, which may
augment bone metabolism directly or via its favorable impact on one or more comorbid health contributors,
deserves study.
As well, with almost no study addressing the other causes of late life osteoporosis that are possibly preventable
or can be mitigated quite markedly by salient melatonin applications according to a substantive body of
data [see Table 1], efforts to explore the efficacy of melatonin in one or more of the age-associated key
osteoporosis correlates listed below as well as others are indicated:
Medical conditions such as diabetes [22]
Persistent pain [39]
Sleep deficits [65,66]
Neurological conditions [70,71]
Inflammatory pathology [72]
Conclusions
While much is currently being written about the impact of poor bone health among older individuals, as
regards bone pain, mobility, falls injuries, frailty, and fractures, more intense scrutiny and attention of the
therapeutic value of melatonin as a safe cost-effective countermeasure to age associated bone losses appears
warranted.
The timing of melatonin supplements and its production relative to bone metabolism should be specifically
investigated.
Bibliography
- Johnston, C. B. & Dagar, M. (2020). Osteoporosis in older adults. Med Clin North Am., 104(5), 873-884.
- Gupta, A. & Singh, P. (2019). Newly discovered molecules as potential candidates for treating osteoporosis. Global J Pharm & Pharmaceut Sci., 7(3), 91-93.
- Noh, J. Y., Yang, Y. & Jung, H. (2020). Molecular mechanisms and emerging therapeutics for osteoporosis. Int J Mol Sci., 21(20), 7623.
- Porter, J. L. & Varacallo, M. (2020). Osteoporosis. In: StatPearls [Internet]. Treasure Island (FL): Stat Pearls Publishing.
- Liu, J., Huang, F. & He, H. W. (2013). Melatonin effects on hard tissues: Bone and tooth. Int J Molecular Sci., 14(5), 10063-10074.
- Kim, A., McDonald, M. & Girgis, C. (2021). The relationship between sleep and bone: Strange bedfellows? Curr Opin Endocrine Metab Res., 18, 236-242.
- Sánchez-Barceló, E. J., Mediavilla, M. D., Tan, D. & Reiter, R. J. (2010). Scientific basis for the potential use of melatonin in bone diseases: Osteoporosis and adolescent idiopathic scoliosis. J Osteoporos., 2010(830231).
- Mauck, K. F. & Clarke, B. L. (2006). Diagnosis, screening, prevention, and treatment of osteoporosis. In: Mayo Clinic Proc., 81(5), 662-672.
- Tu, K. N., Lie, J. D., Wan, C. K. V., Cameron, M., Austel, A. G., et al. (2018). Osteoporosis: A review of treatment options. P T., 43(2), 92-104.
- Olcese, J. & Jockers, R. (2020). Editorial: Melatonin in health and disease. Frontiers in Endocrinol., 11, 613549.
- Amstrup, A. K., Sikjaer, T., Mosekilde, L. & Rejnmark, L. (2013). Melatonin and the skeleton. Osteoporos Int., 24(12), 2919-2927.
- Ferlazzo, N., Andolina, G., Cannata, A., Costanzo, M. G., Rizzo, V., et al. (2020). Is melatonin the cornucopia of the 21st century? Antioxidants., 9(11), 1088.
- Lu, X., Yu, S., Chen, G., Zheng, W., Peng, J., et al. (2021). Insight into the roles of melatonin in bone tissue and bone related diseases. Int J Mol Med., 47(5), 82.
- Li, T., Jiang, S., Lu, C., Yang, W., Yang, Z., et al. (2019). Melatonin: another avenue for treating osteoporosis? J Pineal Res., 66(2), e12548.
- Suzuki, N., Somei, M., Seki, A., Reiter, R. J. & Hattori, A. (2008). Novel bromomelatonin derivatives as potentially effective drugs to treat bone diseases. J Pineal Res., 45(3), 229-234.
- Sandyk, R., Anastasiadis, P. G., Anninos, P. A. & Tsagas, N. (1992). Is postmenopausal osteoporosis related to pineal gland functions? Int J Neurosci., 62(3-4), 215-225.
- Witt‐Enderby, P. A., Radio, N. M., Doctor, J. S. & Davis, V. L. (2006). Therapeutic treatments potentially mediated by melatonin receptors: potential clinical uses in the prevention of osteoporosis, cancer and as an adjuvant therapy. J Pineal Res., 41(4), 297-305.
- Majidinia, M., Reiter, R. J., Shakouri, S. K., Mohebbi, I., Rastegar, M., et al. (2018). The multiple functions of melatonin in regenerative medicine. Ageing Res Rev., 45, 33-52.
- Stagnaro. S. & Caramel, S. (2012). The role of mediterranean diet, coq10 and conjugated-melatonin in osteoporosis primary prevention and therapy. Curr Nutr Food Scie., 8(1), 55-62.
- Bao, T., Zeng, L., Yang, K., Li, Y., Ren, F., et al. (2019). Can melatonin improve the osteopenia of perimenopausal and postmenopausal women? A meta-analysis. Int J Endocrinol., 2019(5151678).
- Oryan, A., Monazzah, S. & Bigham-Sadegh, A. (2018). The effects of melatonin in bone healing. Vet Sci Res., 3(2), 000155.
- Pignolo, R. J., Law, S. F. & Chandra, A. (2021). Bone aging, cellular senescence, and osteoporosis. JBMR Plus., 5(4), e10488.
- Baburina, Y., Lomovsky, A. & Krestinina, O. (2021). Melatonin as a potential multitherapeutic agent. J Pers Med., 11(4), 274.
- Pangiotou, M., Michel, S., Meijer, J. H. & Deboer, T. (2021). The aging brain: Sleep, the circadian clock and exercise. Biochem Pharmacol., 2021(114563).
- Fatemeh, G., Sajjad, M., Niloufar, R., Neda, S., Leila, S., et al. (2021). Effect of melatonin supplementation on sleep quality: A systematic review and meta-analysis of randomized controlled trials. Journal of Neurology.
- Farooqui, K. J., Mithal, A., Kerwen, A. K. & Chandran, M. (2021). Type 2 diabetes and bone fragility- An under-recognized association. Diabetes Metab Syndr., 15(3), 927-935.
- Wajid, F., Poolacherla, R., Mim, F.K., Bangash, A. & Rutkofsky, I. H. (2020). Therapeutic potential of melatonin as a chronobiotic and cytoprotective agent in diabetes mellitus. J Diabetes Metab Disord., 19(2), 1797-1825.
- Kelly, R. R., Sidles, S. J. & LaRue, A. C. (2020). Effects of neurological disorders on bone health. Front Psychol., 11, 612366.
- Hossain, M. F., Wang, N., Chen, R., Li, S., Roy, J., et al. (2021). Exploring the multifunctional role of melatonin in regulating autophagy and sleep to mitigate Alzheimer's disease neuropathology. Ageing Res Rev., 67, 101304.
- Ekeuku, S. O., Pang, K. L. & Chin, K. Y. (2021). The skeletal effects of tanshinones: A review. Molecules., 26(8), 2319.
- Ashrafizadeh, M., Najafi, M., Kavyiani, N., Mohammadinejad, R., Farkhondeh, T., et al. (2021). Anti-inflammatory activity of melatonin: A focus on the role of NLRP3 inflammasome. Inflammation.
- Zhang, Y., Zhang, C., Wang, J., Liu, H. & Wang, M. (2021). Bone-adipose tissue crosstalk: Role of adipose tissue derived extracellular vesicles in bone diseases. Journal of Cellular Physiology.
- Genario, R., Cipolla-Neto, J., Bueno, A.A. & Santos, H.O.. (2021, Jan). Melatonin supplementation in the management of obesity and obesity-associated disorders: A review of physiological mechanisms and clinical applications. Pharmacol Res., 163(105254).
- Barnsley, J., Buckland, G., Chan, P. E., Ong, A., Ramos, A. S., et al. (2021). Pathophysiology and treatment of osteoporosis: Challenges for clinical practice in older people. Aging Clin Exp Res., 33(4), 759-773.
- Jin, H., Xie, W., Hu, P., Tang, K., Wang, X., et al. (2021). The role of melatonin in sarcopenia: Advances and application prospects. Exp Gerontol., 149, 111319.
- Diana, A., Carlino, F., Giunta, E.F., Franzese, E., Guerrera, L.P., et al. (2021). Cancer treatment-induced bone loss (ctibl): State of the art and proper management in breast cancer patients on endocrine therapy. Curr Treat Options Oncol., 22(5). 45.
- Talib, W. H., Alsayed, A. R., Abuawad, A., Daoud, S. & Mahmod, A. I. (2021). Melatonin in cancer treatment: Current knowledge and future opportunities. Molecules., 26(9), 2506.
- Catalano, A., Martino, G., Morabito, N., Scarcella, C., Gaudio, A., et al. (2017). Pain in osteoporosis: From pathophysiology to therapeutic approach. Drugs Aging., 34(10), 755-765.
- Xie, S., Fan, W., He, H. & Huang, F. (2020). Role of melatonin in the regulation of pain. J Pain Res., 13, 331-343.
- Geusens, P. P. & van den Bergh, J. P. (2016). Osteoporosis and osteoarthritis: Shared mechanisms and epidemiology. Curr Opin Rheumatol., 28(2), 97-103.
- Zhang, Y., Lin, J., Zhou, X., Chen, X., Chen, A.C., Pi, B., et al. (2019). Melatonin prevents osteoarthritis-induced cartilage degradation via targeting microRNA-140. Oxid Med Cell Longev., 2019, 9705929.
- Choi, J. H., Jang, A. R., Park, M. J., Kim, D. I. & Park, J. H. (2021). Melatonin inhibits osteoclastogenesis and bone loss in ovariectomized mice by regulating PRMT1-mediated signaling. Endocrinol., 162(6), bqab057.
- Chu, Z. M., Li, H. B., Sun, S. X., Jiang, Y. C. & Wang, B. (2017). Melatonin promotes osteoblast differentiation of bone marrow mesenchymal stem cells in aged rats. Eur Rev Med Pharmacol Sci., 21(19), 4446-4456.
- Da, W., Tao, L., Wen, K., Tao, Z., Wang, S., et al. (2020). Protective role of melatonin against postmenopausal bone loss via enhancement of citrate secretion from osteoblasts. Front Pharmacol., 11, 667.
- Dalla-Costa, K., Yurtsever, F. V., Penteado, J., Martinez, E. F., Sperandio, M., et al. (2020). Melatonin has a stimulatory effect on osteoblasts by upregulating col-i and opn expression/secretion. Acta Odontol Latinoam., 33(2), 125.
- Dong, P., Gu, X., Zhu, G., Li, M., Ma, B., et al. (2018). Melatonin induces osteoblastic differentiation of mesenchymal stem cells and promotes fracture healing in a rat model of femoral fracture via neuropeptide Y/neuropeptide Y receptor Y1 signaling. Pharmaco., 102(5-6), 272-280.
- Huang, R. Y., Hsiao, P. Y., Mau, L. P., Tsai, Y. C., Cochran, D. L., et al. (2020). Synthesis and characterization of melatonin-loaded chitosan microparticles promote differentiation and mineralization in preosteoblastic cells. J Oral Implantol., 46(6), 562-570.
- Jarrar, H., Çetİn Altindal, D. & GÜmÜŞderelİoĞlu, M. (2020). The inhibitory effect of melatonin on osteoclastogenesis of RAW 264.7 cells in low concentrations of RANKL and MCSF. Turk J Biol., 44(6), 427-436.
- Köse, D., Köse, A., Halıcı, Z., Gürbüz, M. A., Aydın, A., et al. (2020). Do peripheral melatonin agonists improve bone fracture healing? The effects of agomelatine and ramelteon on experimental bone fracture. Eur J Pharmacol., 887(173577).
- Murodumi, H., Shigeishi, H., Kato, H., Yokoyama, S., Sakuma, M., et al. (2020). Melatonin induced miR 181c 5p enhances osteogenic differentiation and mineralization of human jawbone derived osteoblastic cells. Mol Med Rep., 22(4), 3549-3558.
- Sharan, K., Lewis, K., Furukawa, T. & Yadav, V.K. (2017). Regulation of bone mass through pineal-derived melatonin-MT2 receptor pathway. J Pineal Res., 63(2), e12423.
- Wang. X/, Liang. T/, Zhu. Y/, Qiu. J/, Qiu. X/, et al. (2019). Melatonin prevents bone destruction in mice with retinoic acid-induced osteoporosis. Mol Med., 25(1), 43.
- Wang, X., Chen, T., Deng, Z., Gao, W., Liang, T., et al. (2021). Melatonin promotes bone marrow mesenchymal stem cell osteogenic differentiation and prevents osteoporosis development through modulating circ_0003865 that sponges miR-3653-3p. Stem Cell Res Ther., 12(150).
- Zhou, Y., Wang, C., Si, J., Wang, B., Zhang, D., et al. (2020). Melatonin up-regulates bone marrow mesenchymal stem cells osteogenic action but suppresses their mediated osteoclastogenesis via MT2 -inactivated NF-κB pathway. Br J Pharmacol., 177(9), 2106-2122.
- Amstrup, A. K., Sikjaer., T, Heickendorff, L., Mosekilde, L. & Rejnmark, L. (2015). Melatonin improves bone mineral density at the femoral neck in postmenopausal women with osteopenia: A randomized controlled trial. J Pineal Res., 59(2), 221-229.
- Kotlarczyk, M. P., Lassila, H. C., O'Neil, C. K., D'Amico, F., Enderby, L. T., et al. (2012), Melatonin osteoporosis prevention study (MOPS): A randomized, double-blind, placebo-controlled study examining the effects of melatonin on bone health and quality of life in perimenopausal women. J Pineal Res., 52(4), 414-426.
- Maria, S., Swanson, M. H., Enderby, L. T., D'Amico, F., Enderby, B., et al. (2017). Melatonin-micronutrients Osteopenia Treatment Study (MOTS): a translational study assessing melatonin, strontium (citrate), vitamin D3 and vitamin K2 (MK7) on bone density, bone marker turnover and health related quality of life in postmenopausal osteopenic women following a one-year double-blind RCT and on osteoblast-osteoclast co-cultures. Aging (Albany NY)., 9(1), 256-285.
- Uslu, S., Uysal, A., Oktem, G., Yurtseven, M., Tanyalcin, T., et al. (2007). Constructive effect of exogenous melatonin against osteoporosis after ovariectomy in rats. Anal Quant Cytol Histol., 29(5), 317-325.
- Cardinali, D. P. & Vigo, D. E. (2017). Melatonin, mitochondria, and the metabolic syndrome. Cell Mol Life Sci., 74(21), 3941-3954.
- Cardinali, D. P., Ladizesky, M. G., Boggio, V., Cutrera, R. A. & Mautalen, C. (2003). Melatonin effects on bone: experimental facts and clinical perspectives. J Pineal Res., 34(2),81-87.
- Ostrowska, Z., Kos-Kudla, B., Swietochowska, E., Marek, B., Kajdaniuk, D., et al. (2001). Assessment of the relationship between dynamic pattern of nighttime levels of melatonin and chosen biochemical markers of bone metabolism in a rat model of postmenopausal osteoporosis. Neuro Endocrinol Lett., 22(2), 129-136.
- Vriend, J. & Reiter, R. J. (2016). Melatonin, bone regulation and the ubiquitin-proteasome connection: A review. Life Sci., 145, 152-160.
- Coto-Montes, A., Boga, J. A., Tan, D. X. & Reiter, R. J. (2016). Melatonin as a potential agent in the treatment of sarcopenia. Int J Molecular Sci., 17(10), 1771.
- Chen, W., Chen, X., Chen, A. C., Shi, Q., et al. (2020). Melatonin restores the osteoporosis-impaired osteogenic potential of bone marrow mesenchymal stem cells by preserving SIRT1-mediated intracellular antioxidant properties. Free Radic Biol Med., 146, 92-106.
- Karasek, M. (2004). Melatonin, human aging, and age-related diseases. Exp Gerontol., 39(11-12), 1723-1729.
- Poza, J. J., Pujol, M., Ortega-Albás, J. J., Romero, O. & en representación del Grupo de estudio de insomnio de la Sociedad Española de Sueño (SES). (2018). Melatonin in sleep disorders. Neurologia., S0213-4853(18)30200-7.
- Tresguerres, I. F., Tamimi, F., Eimar, H., Barralet, J., Prieto, S., et al. (2014). Melatonin dietary supplement as an anti-aging therapy for age-related bone loss. Rejuvenation Res., 17(4), 341-346.
- Igarashi-Migitaka, J., Seki, A., Ikegame, M., Honda, M., Sekiguchi, T., et al. (2020). Oral administration of melatonin contained in drinking water increased bone strength in naturally aged mice. Acta Histochem., 122(6), 151596.
- Xiao, L., Lin, J., Chen, R., Huang, Y., Liu, Y., et al. (2020). Sustained release of melatonin from gelma liposomes reduced osteoblast apoptosis and improved implant osseointegration in osteoporosis. Oxid Med Cell Longev., 2020(6797154).
- Cardinali, D.P. (2019). Melatonin: clinical perspectives in neurodegeneration. Front Endocrinol., 10(480), 1-22.
- Luo, C., Yang, Q., Liu, Y., Zhou, S., Jiang, J., et al. (2019). The multiple protective roles and molecular mechanisms of melatonin and its precursor N-acetylserotonin in targeting brain injury and liver damage and in maintaining bone health. Free Radic Biol Med., 130, 215-233.
- Carrascal, L., Nunez-Abades, P., Ayala, A., Cano, M. (2018). Role of melatonin in the inflammatory process and its therapeutic potential. Curr Pharm Des., 24(14), 1563-1588.