Biography
Interests
Franciane Machado
Department of Trauma-Orthopedic, Physical Fisioterapia, Brazil
*Correspondence to: Dr. Franciane Machado, Department of Trauma-Orthopedic, Physical Fisioterapia, Brazil.
Copyright © 2021 Dr. Franciane Machado. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
With the announcement of the pandemic in March 2020, the challenge has begun to seek not only a cure but also treatment for the repercussions of COVID-19. After the disease, many patients present a variety of problems, among which are musculoskeletal manifestations. This study promotes some considerations about the management of musculoskeletal pain in these patients. Evidencing the importance of the Physiotherapist and a multidisciplinary team in the post- COVID-19 patient.
Introduction
The global pandemic of COVID-19, an emerging infectious disease caused by severe acute respiratory
syndrome coronavirus 2 (SARS-Cov-2), was reported by the World Health Organization in March 2020, after
1 year more than 125 million confirmed cases and over 2.7 million deaths, with a total of 462,824,374 vaccines
administered worldwide [1]. The epidemiological and clinical features, pathogenesis, and complications of
patients with COVID- 19 in the acute phase have been described, the most common clinical manifestations
are fever, cough, and dyspnea, mild cases may progress to severity, requiring ventilatory assistance in intensive
care unit [2], however long-term follow-up studies on persistent symptoms, pulmonary, neurological, cardiac
diseases, musculoskeletal, joint and psychological changes are of utmost need [3]. Some individuals present musculoskeletal and joint pain after recovering from COVID, either due to complications related to the time
they were hospitalized, such as muscle weakness, myopathy, and arthralgia [4,5], or the same manifestations
in individuals with moderate symptoms without the need for hospitalization.
Musculoskeletal pain and arthralgia are the most common complaints in routine physiotherapeutic practice, which has a range of techniques to rehabilitate the lost function and pain management, such as therapeutic exercises, manual therapies, and modalities.
Methods
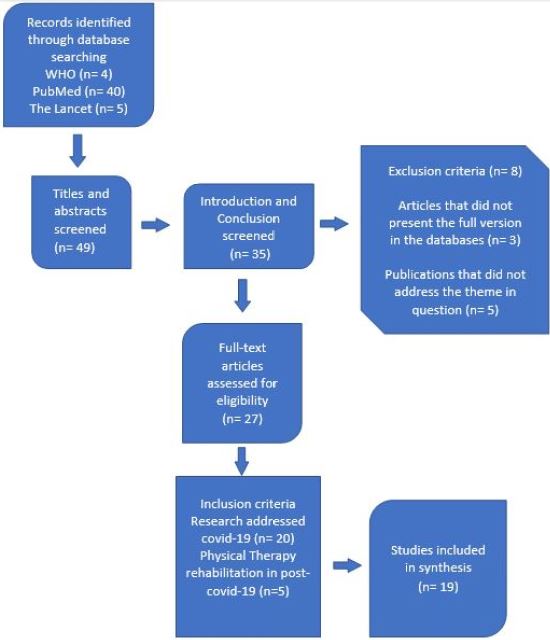
The study was used for methodological purposes as a literature review research. Between June 2020 and
March 2021, the search for publications, as well as texts and reliable articles, indexed in the following
databases: WHO, The Lancet, and PubMed, were diverse articles on the theme of the study were defined
and cataloged. These databases and libraries were chosen because they were considered covering the subject.
The inclusion criteria were: research that addressed COVID-19 as well as its definition, transmission,
study and management of pain, musculoskeletal repercussions, and physical therapy rehabilitation in post-
COVID-19 patients, possible sequelae resulting from the disease, published in Portuguese and English.
As exclusion criteria, the articles that did not present the full version in the databases and libraries searched were discarded, as well as publications and articles that did not address the theme in question.
The articles were evaluated and the productions that met the inclusion criteria were selected for this research by reading the title and the abstract, which were consistent with the theme of the study, the introduction and conclusion were read, seeking a direct relationship with the objective and guiding question of the study (Figure 1).
Results and Discussions
In individuals on mechanical ventilation in the ICU occur sarcopenia and muscle weakness, encompassing
polyneuropathy associated with myopathy and neuromyopathy, regardless of the underlying disease of
hospitalization. Hypotrophy is precocious and begins during the first week of critical illness, such changes
come mainly, from immobilism, mechanical ventilation, and infection [6,7].
A January 2021 cutoff study, which evaluated the health consequences of adult patients discharged from the hospital recovering from COVID-19. It found that after 6 months of symptom onset, most patients had at least one symptom, particularly fatigue or muscle weakness, difficulty sleeping, and anxiety or depression. More severely ill patients were at increased risk of pulmonary diffusion abnormality, fatigue or muscle weakness, and anxiety or depression. Seropositivity and neutralizing antibody titers were significantly lower than in the acute phase [8].
In individuals with moderate and mild symptoms, the musculoskeletal consequences are characterized as nonspecific myalgia in the upper and lower limbs without changes in conduction velocities, in addition to the precise pathophysiological mechanisms in post-COVID-19 individuals are not yet fully understood. The symptomatology is diverse and can last long after hospitalization and infection [6,9].
One should deeply analyze the clinical features, considering the new evidence and new variants of COVID-19. Associate laboratory findings such as inflammatory parameters, related to infection (marked elevation in creatine kinase and lactate dehydrogenase levels, Interleukin-6, Procalcitonin, C-reactive protein) [5,9,10]. It is still unclear whether COVID infection directly affects peripheral muscles or nerves, or whether indirect effects resulting from inflammatory processes and/or immune response occur. Such findings may help to plan rehabilitation protocols in patients with COVID.
The present study aims to elucidate the musculoskeletal manifestations in patients after COVID-19 and bring possible directions for the rehabilitation of these patients considering current guidelines.
Rehabilitation should be patient-centered and adjusted to the patient’s necessities. Consideration should be
given to comorbidities that may affect the patient’s progress, education of the patient and their family members.
A holistic approach should be considered when dealing with these patients, as well as a multidisciplinary
team, considering the potentially serious complications that COVID can cause, especially in patients who
have remained in the ICU, who in addition to respiratory repercussions, may present cognitive, psychological,
neurological, and myoarticular changes, such as prolonged pain, muscle weakness, and poor quality of life.
Therefore, it is prudent to closely monitor patients in the long term [7].
Another notable musculoskeletal complication of SARS was osteonecrosis implicated in steroid therapy, in a dose-dependent manner. Since the WHO has recommended a balanced approach to steroid use for COVID-19, the risk of osteonecrosis should become less likely [7,11]. Thus, making Physical Therapy increasingly indicated to rehabilitate function, manage pain and improve quality of life for these patients.
The complexity and variability of the damage caused by COVID-19, along with the long-term disabling conditions, associated with the presence or absence of pre-existing diseases, leads us to the fact that there is no single, specific method of COVID-19, but rather the necessity for a series of therapeutic conducts and a multidisciplinary team.
In an initial assessment it is important to know the previous symptoms, whether the patient already had pain and/or muscle or joint weakness before COVID, the current symptoms, fatigue, conditioning, well-being, pain, abnormal sensations, what the cognition is like, what the patient is like emotionally, their disabilities and limitations to perform daily activities [11,12].
The COVID-19 clinical management guide published in May 2020, instructs the use of standardized assessment instruments when available. And the provision of personalized rehabilitation programs, from the post-acute to the long-term phase, according to the patient’s needs [13,14].
The management of musculoskeletal pain after COVID-19 can be considered in various aspects, such as the use of telemedicine; biopsychosocial pain management; Physical therapy; the use of opioids, steroids, and non-steroidal anti-inflammatory drugs. [5,12,15].
A holistic approach should be considered when dealing with these patients, as well as a multidisciplinary team, considering the potentially serious complications that COVID can cause, especially in patients who have remained in the ICU, who in addition to respiratory repercussions, may present cognitive, psychological, neurological, and myoarticular changes, such as prolonged pain, muscle weakness, and poor quality of life. Therefore, it is prudent to closely monitor patients in the long term [7].
Another notable musculoskeletal complication of SARS was osteonecrosis implicated in steroid therapy, in a dose-dependent manner. Since the WHO has recommended a balanced approach to steroid use for COVID-19, the risk of osteonecrosis should become less likely [7,11]. Thus, making Physical Therapy increasingly indicated to rehabilitate function, manage pain and improve quality of life for these patients.
The complexity and variability of the damage caused by COVID-19, along with the long-term disabling conditions, associated with the presence or absence of pre-existing diseases, leads us to the fact that there is no single, specific method of COVID-19, but rather the necessity for a series of therapeutic conducts and a multidisciplinary team.
In an initial assessment it is important to know the previous symptoms, whether the patient already had pain and/or muscle or joint weakness before COVID, the current symptoms, fatigue, conditioning, well-being, pain, abnormal sensations, what the cognition is like, what the patient is like emotionally, their disabilities and limitations to perform daily activities [11,12].
The COVID-19 clinical management guide published in May 2020, instructs the use of standardized assessment instruments when available. And the provision of personalized rehabilitation programs, from the post-acute to the long-term phase, according to the patient’s needs [13,14].
Therapeutic considerations and recommendations for the management of musculoskeletal pain post-
COVID-19 can be considered in various aspects, such as the use of telemedicine; biopsychosocial pain
management; Physiotherapy; the use of opioids, steroids, and non-steroidal anti-inflammatory drugs
[5,12,15].
Physical therapy has techniques for musculoskeletal pain management, such as soft tissue mobilizations, myofascial release techniques, modalities, exercises, and others.
Exercises are an important part of post-COVID recovery, they improve physical condition, reduce shortness of breath, increase muscle strength, improve coordination and balance, reduce stress and improve mood, improve memory, can be used for pain management, as well as strength training in patients who have been hospitalized, with low intensity and a moderate number of repetitions, with the evolution of the patient can offer overload and variables in their execution. Starting with less complex exercises (monoarticular) in open kinetic chain, evolving to more complex exercises (multi-articular) in closed kinetic chain [6,12,16,17].
Myofascial release techniques, massage, manual therapies, dry needling, and hot packs may play a role in pain reduction however, they have a low quality of evidence. There is a need for more research to address these findings and examine the effectiveness of these methods for pain management [15].
An easy and portable modality for pain relief is transcutaneous electrical stimulation (TENS) devices. TENS devices use different parameters of frequency and intensity, to stimulate sensory and peripheral nerves. Studies have revealed that TENS can successfully reduce acute pain and chronic pain [15,18].
Part of all rehabilitation is patient education. This encompasses patient self-management and support from caregivers (family members and other professionals).
Conclusions
Complaints of musculoskeletal pain are frequently encountered among patients after COVID-19 and may or
may not be associated with muscle weakness. The mechanism of COVID-19 infection in the musculoskeletal
system has not yet been fully elucidated. Some recommendations for pain management, ensuring continuity
of care, analgesic resources of physical therapy, use of telemedicine, and biopsychosocial follow-up are of
utmost importance for the functional recovery and better quality of life of the survivor of COVID-19.
Acknowledgements
I would like to express my gratitude towards my family for the encouragement which helped me with the
completion of this paper. My beloved and supportive husband, Alexandre who is always by my side when
times I needed him most and helped me a lot in making this study, and my lovable children, Jade and Maitê
who served as my inspiration to pursue this undertaking.
Conflicts of Interests
The author declare no conflicts of interest.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!