Biography
Interests
Ray Marks
Department of Health and Behavior Studies, Teachers College, Columbia University, USA
*Correspondence to: Dr. Ray Marks, Department of Health and Behavior Studies, Teachers College, Columbia University, USA.
Copyright © 2019 Dr. Ray Marks. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Osteoarthritis, a painful irreversible disabling joint disease, and one that predominantly affects articular cartilage, is rapidly increasing in prevalence among older populations. This work aimed to: 1) examine whether vitamin E, a powerful anti oxidant involved in many physiological processes can influence the disease by potentially improving muscular status in the context of the osteoarthritic damaged joint; 2) offer clinical and research suggestions related to this topic. To this end, a comprehensive overview of relevant English language research reports published over the last 20 years was undertaken using key words Vitamin E, Muscle, and Osteoarthritis. Although limited in number, prevailing results show some support for a possible protective, reparative or mediating role for vitamin E as regards the key muscle parameters affecting or affected by osteoarthritis, such as muscle atrophy and muscle weakness. Since no cure exists for osteoarthritis, and muscle is a treatment target of increasing importance in this disease, further research in this regard is strongly recommended and would appear to hold great promise for alleviating the magnitude of the high costs and undue suffering imposed by the disease.
Background
Osteoarthritis, a widespread chronic progressively disabling joint disease strongly associated with progressive
lesions of the articular cartilage tissue lining synovial joints such as the hip and knee, is also commonly
accompanied by pathological changes in the surrounding muscle, as well as bone. Often considered an
inevitable component of aging with no currently truly effective means of preventing or treating this condition,
discussions about the role played specifically by muscle in this disease has led to the idea that muscle is
potentially an important treatment target, including primary, secondary, and tertiary levels of osteoarthritis
prevention. Although vitamin E appears to be efficacious for treating osteoarthritis in its late stages [1], and
a role for muscle in osteoarthritis pathology has been implicated in the disease cycle [2,3], alongside the
potential of dietary factors in general for preventing and treating osteoarthritis [4,5], very few discussions
have ensued as to whether vitamin E-a generic term referring to a total of 4 tocopherol and 4 tocotrienal
derivatives [6] is of any import in specifically protecting against osteoarthritic muscle damage and atrophy
[7], given its well established anti-inflammatory and neuroprotective functional influences [6].
In light of the enormity and extent of osteoarthritis disability incurred globally by aging adults, and some evidence that an inadequate vitamin E intake and/or subnormal plasma concentrations of this compound may be implicated as one possible understudied pathogenic factor, it was perceived that it may be useful to examine whether there is any evidence to support the possibility of a consistent directional association between vitamin E levels and aspects of muscle status such as muscle mass and muscle composition, frequently impaired in people with varying degrees of osteoarthritis. Given that human skeletal muscle is a vital organ involved in movement and force generation that suffers from deterioration in mass, strength, and regenerative capacity with aging [8], as well as in osteoarthritis [2], support for a linkage between these factors in the relevant literature was sought.
Aims
Accordingly, this present review aimed to examine the degree of consensus in favor of a clinically relevant
role for vitamin E in predicting or influencing the extent or rate of muscle pathology found in osteoarthritis,
either directly or indirectly. Since no specific approach can currently be shown to safely alter the natural
course of osteoarthritis, or produce long-term, clinically relevant benefits in this condition, and exercise
strongly advocated for this condition is often ineffective in the long-term, a further aim was to establish
if vitamin E supplementation can possibly provide a novel and efficacious supplementary approach in this
regard.
Methods
To obtain data relevant to the present topic of interest, a scoping review using the search terms Vitamin E and
Muscle, Skeletal Muscle, Muscle Atrophy, Muscle Strength, or Muscle Cells, Vitamin E and Osteoarthritis,
and Muscle and Osteoarthritis was applied. Acceptable information sources for this review included
peer-reviewed literature reviews, case studies, cross-sectional studies and prospective studies, regardless of
substrate studied.
The key data base used was PUBMED, although other data bases such as Google Scholar were searched. To identify key issues in this diverse literature, the available data published over the years 2000-2019 were specifically scanned, and relevant papers were then downloaded, and scrutinized. As well, a manual search of references in these papers was conducted, where indicated. The selected materials were then divided into those that discussed aspects of osteoarthritis related to vitamin E and muscle, plus studies representing laboratory research approaches that have examined vitamin E and muscle interactions of some sort, versus those that have been performed on human samples. A narrative perspective was chosen to depict the nature of the data, given the paucity of data and its obvious heterogeneity. For that reason, no distinction was made between studies examining vitamin E subgroups of tocopherols and tocotrienols or their isomers, and the terminology discussed in this paper follows that reported by the authors in the reviewed studies.
Results
The overall finding of the literature search was that the number of articles matching the present key words
was very limited, especially if compared to other related topics in this realm such as vitamin D and muscle,
and osteoarthritis and exercise. Of the available vitamin E studies that examined its association with muscle,
most were clearly preclinical in nature, with no consistent approach or substrate. Varied forms of vitamin E,
as well as dosages, plus muscle features were evident and the diverse substrates or subjects studied in both the
laboratory and clinic venues precluded any form of robust quantitative analysis. In addition, very few clinical
studies focusing in some way on this present topic were well-designed, and the majority were observational
or experimental rather than intervention studies. Many articles have recently focused on muscle problems in
osteoarthritis, but none linked this feature of the disease specifically to osteoarthritis. To elaborate upon the
prevailing literature in this regard, the key results identified in the literature are reported below in narrative
and tabular formats.
Over and above the hallmark characteristic of osteoarthritis, namely its adverse effect on articular cartilage
structure and function, the literature reveals a sizeable volume of contemporary research that indicates
muscle strength losses, as well as muscle atrophy commonly accompany the osteoarthritic disease process
[9-12]. As well muscle co-activation processes may be abnormal, as may fat content. Muscle inflammation,
and deficits in muscle power, endurance, and function [13-17] also prevail. Other muscle related problems
that adversely impact osteoarthritis progression include various degrees of:
• Muscle protein degradation
• Muscle atrophy of both fiber types
• Muscle proprioception changes
• Muscle fiber distribution abnormalities
• Muscle denervation
• Muscle contractile deficits
• Muscle fatigue
• Muscle inflammation
• Reduced muscle cross-sectional area
• Muscle inhibition
• Muscle weakness [18]
Important in the context of the present discussion is the observation that the underlying muscle problems and the general progression of osteoarthritis involve the presence of excess oxidative stress and inflammation [19,20] that can interact to foster a negative set of joint destructive processes. Although the origin of muscle dysfunction in osteoarthritis is not clear, a role for vitamin E through its impact on multiple pathways including muscle [1-22] cannot be ignored. Unfortunately, muscle problems in osteoarthritis, which may be both causative or reactive in nature [18], and which are key to improving life quality and joint status in this disease, are not readily resolved to any long-term degree through traditional therapeutic exercise approaches. While many reasons for this prevail, a role for vitamin E in this respect is not one that has been considered to any degree to date, despite some compelling evidence as outlined below that could potentially be exploited help to attenuate any ensuing potentially reversible strength and muscle endurance deficits.
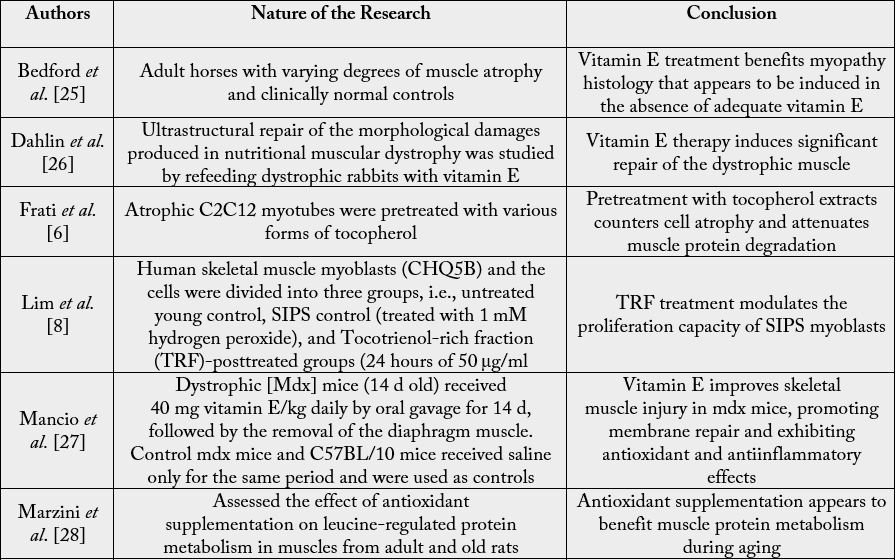
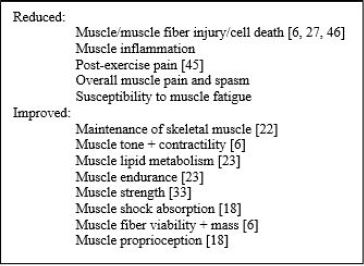
Although small in number, laboratory studies examining linkages between the antioxidant properties of vitamin E and muscle structure and function, generally support the view that while oxidative stress may contribute to muscle damage, the presence of adequate levels of vitamin E may protect against muscle damage and dysfunction [23,24]. In addition to helping to prevent muscle atrophy, vitamin E may help to offset potential muscle protein losses, as well as muscle cell damage, myoblast atrophy and myotube degeneration [23].
Its presence at adequate levels may also impact favorably on muscle lipid metabolism, as well as muscle inflammation, often associated with osteoarthritis, while a persistent state of vitamin E deficiency may foster the onset of a myopathy [25], as well as exercise induced fatigue [23], muscle atrophy [25], a heightened muscle proteolytic rate, and type I muscle fiber contractile dysfunction [23] as depicted in Table 1 below.
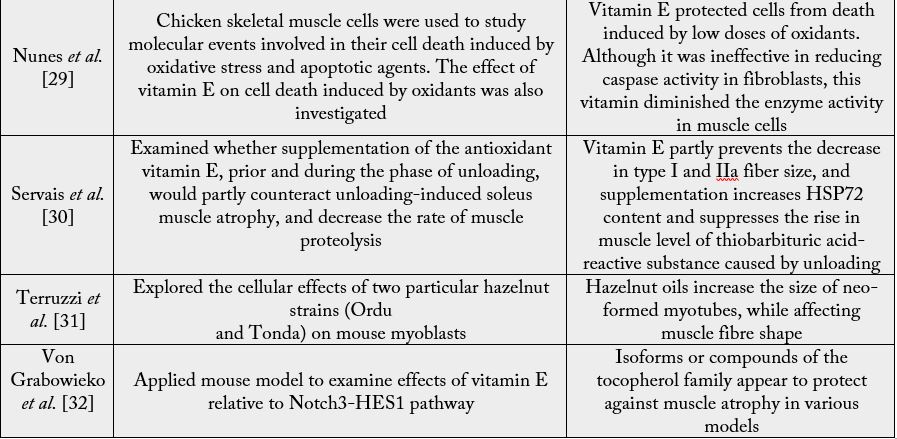
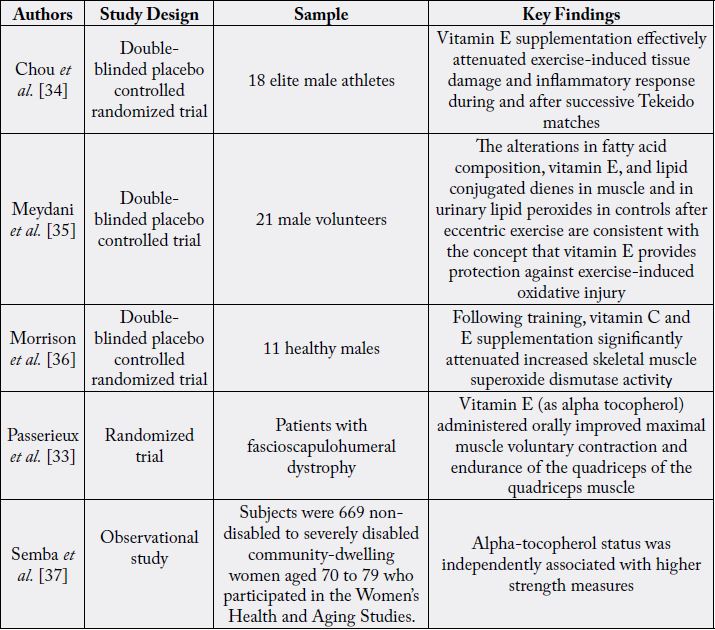
Among the few clinical studies that pertain to the present topic, as with laboratory outcomes, those below
imply a positive role for vitamin E in the maintenance and functional status of muscle, despite their diversity and limited approaches and samples. See Table 2. While no study could be found that directly set out to
explore vitamin E and its association with osteoarthritis muscle, a major reason provided for the observed
benefits of vitamin E in some cases is its established impact on susceptibility to oxidative stresses [33],
although its protective effect might impact several other functional pathways of osteoarthritic muscle
tissue [32]. Unfortunately, even though quite a number of clinically oriented studies detailing vitamin E
associations with osteoarthritis prevail, none assessed muscle related associations to any degree, other than
providing estimates of function with and with or vitamin E presence [19], and not all were in agreement as
to whether vitamin E is at all beneficial for preventing or treating osteoarthritis.
Discussion
The role of nutriceuticals as well as muscle in mediating or moderating osteoarthritic joint outcomes has
received increasing support in the past decade or so due to the need to better understand the origins of the
disease as well as to uncover novel non toxic solutions to this seemingly intractable progressive disease. At
the same time, several laboratory and clinical studies confirm that vitamin E is essential for the maintenance
of the structural and functional components of skeletal muscle [38,39], and that its deficiency produces
muscle degeneration [40] as well as apoptosis and death of skeletal muscle cells [29,38,41]. A vitamin E
deficiency is also found to produce dystrophy and alterations in the chemical composition and functional
behavior of muscle [38] that closely resembles some features of osteoarthritic muscle pathology, which is
susceptible to oxidative damage, and subsequent muscle mass as well as strength losses. Other data show
that vitamin E deficiencies can influence those detrimental oxidative processes that impact muscle structure
and function in older adults, regardless of health status, as well as the onset or rate of progression of any
prevailing sarcopenia [24]. Angthong et al. report that as the concentration of vitamin E in synovial fluid
decreases, the severity of knee osteoarthritis increases [42], a situation wherein the effects of low vitamin E
levels as a risk factor for muscle weakness in osteoarthritis cannot be ruled out.
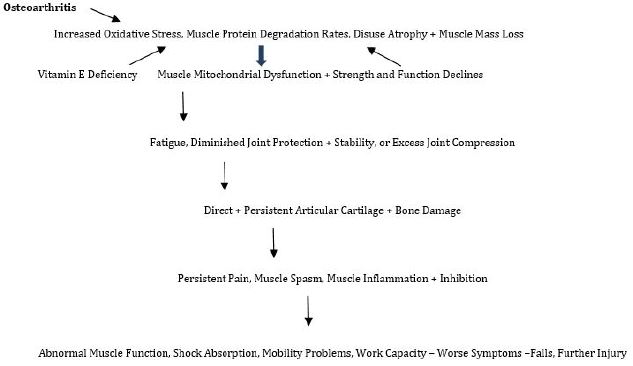
Moreover, acting directly on other features of muscle pathology found in osteoarthritis, such as muscle protein degradation, the presence of vitamin E may arguably either help to offset or reduce the extent of joint pathology attributable to muscle in this disease, that correlates with disease progression [38], or its absence may hasten muscle dysfunction and the ensuing rate of joint degeneration. Vitamin E also affects metabolic syndrome and cardiovascular disease features, as well as inflammation, pain, collagen degradation, and cellular damage [43] frequent correlates in osteoarthritis that could affect muscle function and its properties either positively or negatively, directly, as well as indirectly. Since muscle and muscle quality reportedly influence subchondral bone status, mobility status, joint shock absorption, cartilage nutrition, and joint stability and alignment, subject to further research, efforts to ensure vitamin E levels are not deficient, along with the use of vitamin E to reduce and prevent the degree of osteoarthritis muscle pathology that may ensue where indicated may yet provide a highly innovative as well as cost-effective efficacious approach to ameliorating the interactive cycle of osteoarthritic disability as a whole as portrayed in Figure 1.
Conclusion
Although data is limited and caution is advised in interpreting the available data, preliminary research
strongly implies there is added value to ensuring desirable vitamin E serum levels prevail in the context of
averting premature or excess muscle related deficits, especially among the older population, and sarcopenic
older adult [43], very prone to injury and osteoarthritis and muscle pathology. In particular, and consistent
with available data of a strong moderating or mediating association between vitamin E and muscle structure
and function, as well as an increasing volume of evidence of a highly significant association between
osteoarthritis and damage to the muscles surrounding the affected joint[s], it appears further consideration
of this body of research, along with rigorous and thoughtful research in this area might not only prove highly
revealing, but highly advantageous clinically in multiple ways.
Indeed, since there is little dispute in the current body of research describing vitamin E-linkages to muscle status, including a possible vitamin E muscle-strength connection in osteoarthritis [44], it appears a focus on examining the diverse forms of vitamin E and their potential influence on the various muscle mechanisms and derangements that prevail in osteoarthritis is likely to yield highly valuable clinical insights.
In this regard, and despite no proof -of-principle- trial in this regard, in favor of a viable role for vitamin E in fostering muscle maintenance and mass in osteoarthritis situations is its well-established anti-oxidative and anti-inflammatory properties [45] observed to protect muscle cells from damage caused by free radicals [27,46]. Other data show vitamin E can both positively as well as negatively influence skeletal muscle maintenance and fiber degeneration, among other muscle related deficits that raise the risk for pain, joint array of disabling functional features, pathology, and inflammation that is challenging to resplove. To the contrary, a parallel body of research data show Vitamin E is efficacious in fostering overall health benefits that may well impact osteoarthritis muscle dysfunction indirectly and favorably [47-49] as alluded to in Box 1.
Moreover, its possible role in reversing this disease cannot be ruled out in cases where muscle is the key pathogenic factor [49,50].
To this end, it is concluded that concerted efforts to continue to examine the proof of concepts presented in this overview will prove of immense value and may help reveal novel insights not only concerning the osteoarthritis disease process, but as to what is needed in specific cases to foster its prevention, amelioration, or optimal outcome.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!