Biography
Interests
Zhang Wupeng, Yang Yongliang, Xu Shihong, Wang Fengrui, Tu Yi, Wang Bomin & Wang Fu*
Department of Emergency trauma, Shandong Provincial Orthopedic Hospital, Provincial Hospital Affiliated to Shandong University, Jinan, China
*Correspondence to: Dr. Wang Fu, Department of Emergency trauma, Shandong Provincial Orthopedic Hospital, Provincial Hospital Affiliated to Shandong University, Jinan, China.
Copyright © 2019 Dr. Wang Fu, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
The occurrence of osteopetrosis is related to the function defect or the decrease of the number of osteoclasts, which is characterized by the abnormal activity of osteoclasts, bone resorption defect and bone sclerosis, and eventually leads to the increase of bone density, the narrowing or even disappearance of bone marrow cavity, and the brittle bones. The disease was first reported by German radiologist albers-schnberg in 1904. The disease is obviously hereditary and familial. According to the classification, there are different clinical manifestations in different systems of human body. At present, there is no clear incidence statistics in China, and most of the introductions about this disease at home and abroad are case reports. In this paper, the classification, diagnostic evaluation and treatment principles of osteopetrosis were reviewed by reviewing the literature and combining with two patients with osteopetrosis diagnosed and treated in our hospital, so as to provide clinical references for the diagnosis and treatment of osteopetrosis and improve the level of diagnosis and treatment of osteopetrosis.
Introduction
Osteopetrosis is also known as osteosclerosis disease, marblebone disease, primary brittle osteosclerosis
disease, generalized brittle osteosclerosis, chalkopathy, etc. [1]. The disease was first reported by German
radiologist albers-schnberg in 1904 [2,3], and then named as osteopetrosis disease according to its pathological
characteristics. Osteopetrosis is a rare disease of abnormal osteoclast activity and bone resorption defect
caused by the function defect of osteoclast or the decrease of the number of osteoclasts [4]. It is a kind
of extensive skeletal disease characterized by osteosclerosis, obliteration of the medullary cavity, calcified
cartilage, and brittle bones [5,6]. It has been reported in foreign literature that the incidence of osteopetrosis
in North America is 1/500,000 [7]. According to epidemiological studies, Balemans, W., et al. reported that
the average incidence of ADO was about 5/100,000, the average incidence of ARO was about 1/250,000,
and XLO was extremely rare [8].
Clinical Classification and Characteristics
In 1942, CLAIRMONT and SCHING confirmed for the first time that osteopetrosis is familial
inheritance[9]. Osteopetrosis according to their different disease genes can be divided into autosomal
dominant osteopetrosis(ADO), autosomal recessive osteopetrosis(ARO), and X - linked osteopetrosis(XLO)
three kinds. ADO is benign osteopetrosis, mostly occurs in adults, without obvious clinical manifestations.
Most of the fractures were found in the proximal femur after admission due to trauma.ADO has three
subtypes: benign Ⅰ type (ADO - Ⅰ), benign Ⅱ type (ADO - Ⅱ) and benign Ⅲ type (ADO - Ⅲ) [8,10]. ARO
comes on early, occurs in infants and young children, mostly malignant, progresses rapidly, and has a high
fatality rate [11]. XLO is even rarer.
Characteristic X-ray Features
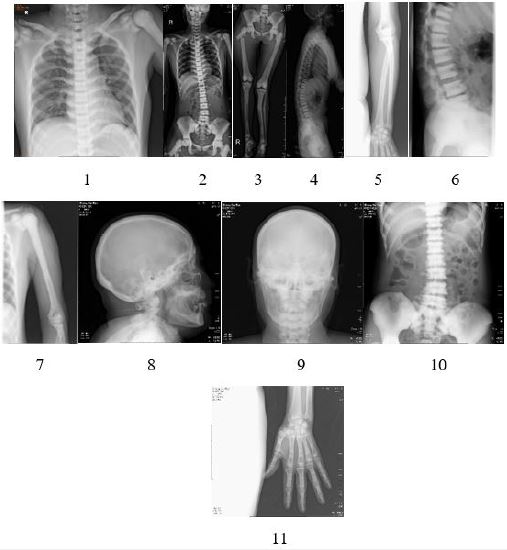
Preoperative X-ray examination of the patient was shown in the following figures [12]: (1) increased bone
density, osteosclerosis, obliteration of the medullary cavity, and calcified cartilage, also verified intraoperatively.
(2) mild scoliosis of the spine with “sandwich verte- brae” sign; The epiphysis end of the four limb bone is
widened, showing typical “erlenmeyer flask deformity” sign [13]; Rib “beaded” changes; (3) typical highdensity
shadows at the skull base and pelvis, thickening of the skull, obvious hardening of the skull base,
and typical “concentric ring sign” of iliac bone wings on both sides [14]; (4) various degrees of bone-in-bone
phenomena can be seen in the bones of the limbs, fingers and metacarpal.
Report of the Cases
The two patients were informed that these cases studies would be submitted for publication, and they
provided informed consent.
Case 1: the patient, male, 38 years old, was transferred to the department of trauma and emergency surgery of our hospital on February 22, 2018 due to “pain and dysfunction of right hip joint after trauma for more than one month”. Conservative treatment has been conducted since diagnosis in the local hospital in January. Physical examination after admission: right hip tenderness, percussion pain, limited movement, mild shortening deformity of the right lower extremity, good sense and movement of the right foot, good pulse of the dorsal foot artery, no obvious abnormality in the rest of the limbs. Admission diagnosis: 1. Subtrochanteric fracture of the right femur 2. osteopetrosis.
Admission laboratory examination: white blood cell 1.72×109/L, erythrocyte 2.24×1012/L hemoglobin 59g/L, platelet 68×109/L, hematocrit 19.40% total protein 62.2g/L, alkaline phosphatase 96U/L, adenosine dehydrogenase 25.10mmol/L total cholesterol 2.14mmol/L, blood phosphorus 1.54mmol/L, d-dimeric 1.01mg/L, uric acid 531umol/L, and other test indicators were not significantly abnormal.
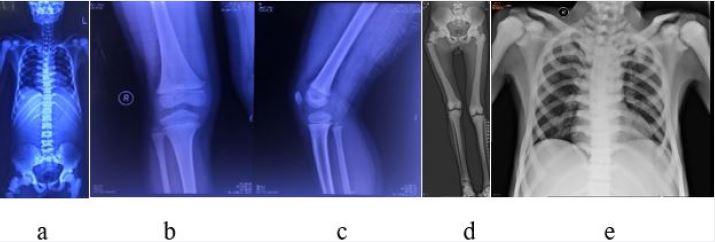
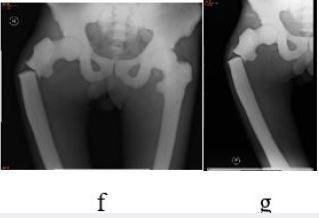

Case 2: the patient, female, 61 years old, was transferred to our department on June 17, 2018 due to “right hip pain caused by accidental trauma accompanied by limited movement for 7 hours”. Physical examination: right thigh proximal swelling, deformity, limited movement, obvious tenderness, palpable bone rubbing sensation, dorsal foot artery pulsating well, no paresthesia at the right lower limb. Over 40 years ago, the left leg was injured and the tibia fracture was malunion with conservatively treatment. Admission diagnosis: 1. Right femur subtrochanteric fracture 2. Osteopetrosis 3. Hypertension 4.old fracture malunion of left tibia fracture.
Admission laboratory examination: hematocrit was 34.00%, lymphocyte percentage was 18.9%, serum potassium was 3.09mmol/l, adenosine dehydrogenase was 26.60mmol/ l, d-dimer was 6.21mg/l, fibrin degradation product was 16.99ug/ml, urea nitrogen was 531mmol/l, ureanitrogen/creatinine was 131.5.


Discussion
Osteopetrosis disease is extremely rare in the world, and the search for clinical data at home and abroad
is mostly reported cases. Currently, there is no unified treatment plan. Zhu Guanghua et al. proposed that
hematopoietic stem cell transplantation can be used to treat osteopetrosis [15]. It has been pointed out
in the literature that hematopoietic stem cell transplantation is an effective method for the treatment of
osteopetrosis, and it can achieve a radical effect for some types [16]. Robert D Golden et al. successfully
treated one patient with osteopetrosis by applying the internal fixation and recombinant human bone
morphogenetic protein-7, but there was no data to support the application of recombinant human bone
morphogenetic protein-7 in delayed healing of patients with osteopetrosis [17]. Srivastav Amit et al. used
the distal femoral locking compression plate to treat osteopetrosis patients with subtrochanteric fractures,
which healed 22 weeks later [18]. Based on the review of previous literature, f. Seyfettinoglu et al. believe
that the treatment of fractures in patients with osteopetrosis will be difficult: healing takes a long time,
various intraoperative problems such as broken drill bit may occur, and the risk of postoperative infection for these fractures is high. Spare bits should be used, absolutely following general disinfection rules to avoid
infection. Regardless of the implant used, the perspective image must be carefully evaluated intraoperatively.
Patience is necessary to open the medullary canal during surgery [19]. Huang, J., et al., treated displaced
fracture with open reduction and internal fixation, and the fracture healed after 12 months [20]. Mert
Kumbaraci et al. first applied PFNA in patients with osteopetrosis [21]. Kunnasegaran, R., et al., believed
that tungsten carbide drill bit was a safe and effective method for treating proximal femur fracture with
osteopetrosis [22]. Akira Hashimoto, et al. believe that THA is a very useful method for the treatment of
osteopetrosis, but careful planning should be made in the treatment of THA [23].
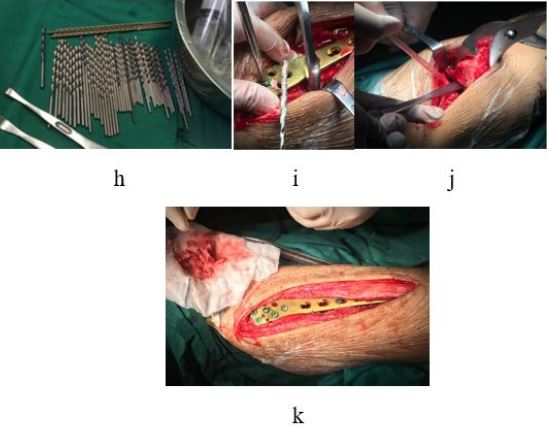
Osteopetrosis is a rare hereditary disease in the world, there is currently no special clinical treatment,and we think the treatment difficulties mainly include the following aspects: 1. In patients with osteoblastoma, bone density increases uniformly and widely, hardening, narrowing or even disappearance of the medullary cavity, and difficulty in reaming, so intramedullary fixation is not the first choice, and steel plate internal fixation can be preferred; 2. Due to the high hardness and brittleness of the bone, it is very likely that the common rigid drill bit cannot drill through to the contralateral cortex, and even the drill bit fracture remains in the bone or causes fractures in other parts, which further increases the difficulty of operation; 3. After fracture fixation, the patient is more likely to suffer fracture or breakage of internal fixator when receiving external force; 4. Patients with osteopetrosis have poor intramedullary hematopoietic function, poor blood supply at the broken end of the fracture, and long healing time at the broken end of the fracture, ranging from several months to several years. It is highly likely that the fracture will not heal. All members of the department carried out active case discussions and formulated detailed operation plans according to the patients’ special conditions: the drill bit with higher strength tungsten carbide was used to avoid the breakage of the drill bit during the operation; At the same time, multiple sets of internal fixation devices should be fully prepared in case of unpredictable intraoperative events.
Conclusion
In conclusion, osteopetrosis is a rare genetic disease with diverse, complex and difficult clinical manifestations
and with different treatment plans. At present, its pathogenic genes and pathogenesis need further
exploration and research by medical personnel and scientific researchers, so as to provide convenience for
clinical work. Specific X-ray imagings are the key points of its diagnosis. Appropriate symptomatic treatment
should be given according to clinical symptoms and signs. We believe that for patients with this type
ADO osteopetrosis, it is more effective to choose open reduction plate and screw internal fixation with
comprehensive consideration.
Conflicts of Interest
The authors declare no conflict of interest in this work.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!