Biography
Interests
Bouabdellah, M.1*, Bouzidi, R.1, Ammar, A.2, Hadhri, K.1, Lebib, H.1 & Kooli, M.1
1Department of Orthopedic and Traumatology of Charles Nicolles Tunis
2Institute of Orthopedic Surgery Mohamed Taieb Kassab Manouba, University Tunis Elmanar
*Correspondence to: Dr. Bouabdellah, M., Department of Orthopedic and Traumatology of Charles Nicolles Tunis.
Copyright © 2019 Dr. Bouabdellah, M., et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
The objective of this study was to evaluate and to compare the dynamic hip screw and intramedullary
Gamma™ nail fixation for the treatment of pertrochanteric fracture in terms of stability,
complications and cost effectiveness.
This prospective randomized study included 36 patients hospitalized in an emergency setting for
instable per trochanteric fracture next term between June 2018 and December 2018. Two fixation
systems were used: the Gamma™ proximal femoral nail and the screw plate dynamic hip screw
DHS. We noted: operative data (type of implant, duration of surgical procedure), postoperative data
(blood loss, radiographic findings, early complications), and outcome mortality and radiographic results. All patients were assessed least six months after surgery. The series included 36 patients, 16
men and 20 women. The Gamma™ nail was used for 15 patients and the DHS for 21. The AO
classification was: A2 1= 11, A2 2 =10, A2 3 =4, A3 1 =3, A3 2 =2, A3 3= 6. All this fractures were
unstable.
Mean operative time was 125 minutes for intramedullary nailing and 92 minutes for screw plate
fixation (0. 004). Mean blood loss was 55ml for intramedullary nailing and 800ml for screw plate
fixation (p = 0.006). The mean hospital stays were 11 days in Gamma™ nail group and 12.5 in DHS
group. At six months, no mechanical complication was involved in the two groups, such as migration
of the cervical screw outside the femoral head. Three deaths occurred in the intramedullary nailing
group, and one in the DHS group.
Data in the literature report an advantage for intramedullary nailing, particularly a mechanical
advantage, for the treatment of per trochanteric fractures. Our findings show similar results with
less bleeding and earlier charge in the Gamma™ nail group.
Introduction
The trochanteric fractures are the most common of the elderly; they maintain a high mortality rate [1].
They are a public health problem, especially with the increase in life expectancy and the risk of osteoporosis.
The number of fractures of the upper extremity of the femur is expected to increase from 1.7 million in
1990 to 6.25 million in 2025. These figures give some idea of the magnitude of the problem, which has an
international dimension [2-4].
The frailty of these elderly patients makes it necessary to reduce the risk of surgical complications. Various means of osteosynthesis have been developed to treat these fractures: screw plate DHS, THS, nail with centro-medullary support: Gamma™, PFN ... [5]. The aim of this study is to evaluate the morbidity of surgical treatment of unstable per trochanteric fractures and to compare a support material on the lateral cortical of the femur: the DHS (Dynamic Hip Screw) and an endo-medullary material with cephalic anchor screws: the Gamma™ nail, both of which are commonly used in this indication. The evaluation of the perioperative parameters, stability, complications, and cost/effectiveness were sought.
Material and Method
This is a prospective, randomized study, including 36 patients, hospitalized in emergency for unstable
pertochanteric fractures in the department of orthopedics and traumatology of Charles Nicolle Hospital in
Tunis, Tunisia, between June 2018 and December 2018. The randomization was performed consecutively by
a random table. All measurements were performed by a single investigator.
The inclusion criteria were: patients who arrived in emergency for a fracture of the trochanteric region classified A2 or A3 according to the AO classification [6]. (Fig. 1) with an ASA score [7] less than or equal to 4.
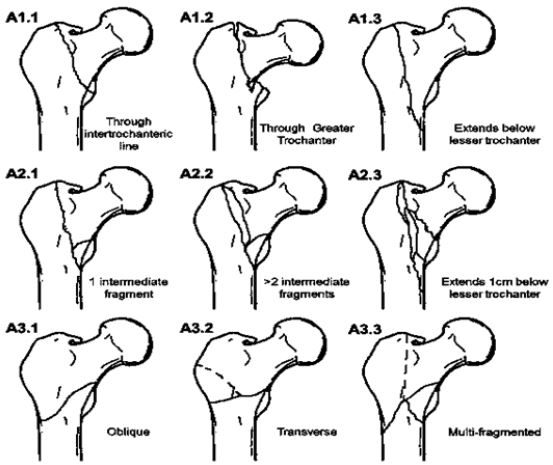
The exclusion criteria were: senile dementia, non-autonomous patients before the trauma, A1 type fractures according to the AO classification, and ASA scores from 5 to 6.
Two osteosynthesis techniques were performed: the Gamma™ nail and the DHS screw plate. Preoperative assessment included: sex, age, search of a chronic disease and ASA score. The fractures were classified according to the AO classification. The criteria of judgment between the two techniques of osteosynthesis were: the duration of the intervention, the anatomical character or not of reduction according to the criteria of Baumgaertner (anatomical or acceptable) [8]. The quantity of blood collected by the aspiration drain, the immediate postoperative complications, the duration of stay in hospital and the recovery time of weight bearing.
At six months postoperatively, the mortality rate and late mechanical complications were assessed. The statistical analysis of the different variables was performed using Statistic Package for Social Sciences (SPSS). Differences were considered to be statistically significant when P<0.05. The chi-square test was used to compare differences between the two techniques for each variable, and the Student’s t-test was used for quantitative variables.
Results
Thirty-six patients were included: 20 women and 16 men. The average age of the patients was 75 (62 to 88
years). 15 fractures were fixed by Gamma™ nail (9 women and 6 men), and 21 by DHS (11 women and 10
men). Twenty-eight patients (77%) had one or more chronic medical disease.
The average operating time for Gamma™ nails was 125 minutes and 92 minutes for DHS. According to the criteria of Baumgaertner, the reduction obtained was judged anatomical in 11cases (73%) and nonanatomical but acceptable in 4 cases for Gamma™ nails. For DHS, it was anatomical in 16 cases (76%) and acceptable in 5 cases. Mean blood loss was 550ml with Gamma™ nails and 800 ml with DHS with significant difference (0.004).
The length of stay was on average 10.5 (± 3) days for Gamma™ nails and 12.6 (± 2) days for DHS with a non-significant difference (0.02).
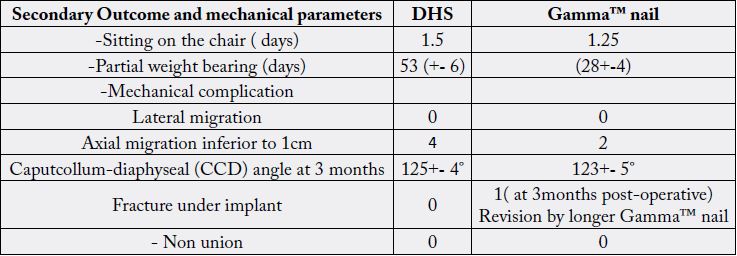
The resumption of the weight bearing was carried out, on average at the 28th day for the Gamma™ nail, and at the 53rd day for the DHS. These complications included deep vein thrombosis, two Escher, urinary tract infection, three anemia, pulmonary embolism, neuropsychiatric disorders, and stroke with right hemiplegia. Comparison between the two groups seems difficult. However, in absolute numbers, the overall complications for DHS were 8 for 21 patients (38%) and 2 for 15 (13%) patients treated with Gamma™nail, without prejudging their severity. An immediate postoperative death by ventricular tachycardia complicated by cardiac arrest in a patient operated by Gamma™nail was noted (Table 1).
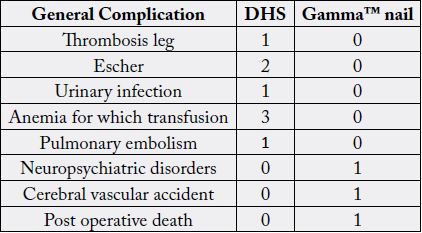
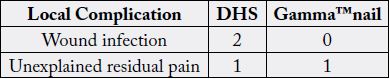
Local complications were more common with DHS, but some of these complications did not result in functional repercussions. The complications encountered were wound infection treated with surgical drainage and adapted antibiotic therapy in a patient treated with DHS.
Unexplained residual pain, persistent in one case treated with DHS and a case treated with Gamma™ nail (Table 2)
At six months, the mortality rate was 3 cases in the Gamma™ nail group and 1 case in the DHS group. Mechanically, no displacement of the cervical screw or axial migration was noted in both groups. The parameters of stability and consolidation are presented in Table 3.
Discussions
The trochanteric fractures are a major cause of mortality and morbidity and functional loss in the elderly.
Their morbidity is closely related to the degree of fracture instability and comminution as well as the quality
of reduction and osteosynthesis. Many devices have been described in the treatment of pertrochanteric
fractures [9-12]. Many studies have compared the Gamma™ nail, to screw plate systems.
At first, the Gamma™ nail seemed to provide better results: shorter operating time, less bleeding and earlier weight bearing compared to external plate systems [13].
Nailing seems to have a theoretical advantage in reducing bleeding, the risk of sepsis, and the risk of tissue damage and the time of surgical procedure compared with direct open surgical techniques. At last followup, the clinical and radiographic results are equivalent [14].
Many study showed better functional results in the Gamma™ nail group compared to the DHS group. This was due to the minimally invasive approach, reduced pain, with a quick chair setting [15,16].
These results were confirmed by a meta-analysis published by Ma KL [17] comprising 14 studies with 1 983 patients comparing nailing versus the outer plate. On the other side, this meta-analysis reports a greater risk of femoral shaft fracture with intramedullary nailing. Similarly ,Yeganeh et al. [18] showed clinical and radiographic superiority with lower bleeding and earlier weight bearing of PFN nail compared to DHS screw plate . Calderón et al. [19] reported the superiority of the nail in a shorter time of surgical procedure and postoperative pain, less bleeding and earlier weight bearing. On the other hand, the clinical and radiographic results were equivalent in the long term.
Nevertheless, level I studies have reported different conclusions. Ahrengart et al. [20] showed in a study out of 426 patients an increased operative time and bleeding for the Gamma™ nail.
The classic complications of the Gamma™ nail mentioned in many publications were intraoperative fractures of the greater trochanter, caused by the large metaphyseal diameter of the implant as well as fractures under the nail [17,21-24]. And Svenson et al. [25] showed a higher rate of surgical revision in the Gamma™ groups for secondary displacement of the fracture or fracture under the nail. Finally, Adams et al. [14] showed that, despite the greater stability of the Gamma™ nail compared to the screw plate, the difficulties of optimal positioning of the cephalic screw with increased risk of secondary displacement type and its characteristic complications (diaphyseal fractures, trochanteric rests). For this reason, its superiority over the screw plate was not admitted.
A stress fracture of the nail can occur especially when the fracture is pathological or unstable with a subtrochanteric component [26].
Open direct approach osteosynthesis has the theoretical advantage of allowing anatomical reduction, with the disadvantage of additional devascularization of the fracture site and increased bleeding and infectious risk. Moreover, this method does not allow an optimal fixation of unstable fractures and therefore does not always allow early weight bearing with complete safety [27-29].
The use of the DHS screw plate is a reliable and simple method for the synthesis of pertrochanteric fractures [30]. Oger et al., with 84 fractures in 82 patients, found 100% consolidation and 4.8% mechanical complications (sweeping and disassembly of the plate). The sliding of the screw is more important in unstable fractures and this despite deferred weight bearing.
A study by Kaiser et al. [31], on 24 human cadavers, shows a greater deformation of the DHS compared to the Gamma™ nail. On the other hand, this rigidity is accompanied by a higher degree of femoral diaphyseal fracture. For open osteosynthesis, the use of locked compression plates could improve mechanical stability. Indeed, in a prospective randomized comparative study between PFN nail and proximal femoral locked plate (PFLCP), Singh et al. [32] found equivalent clinical and radiographic results in the treatment of unstable trochanteric fractures at 2 years of follow-up.
Biomechanical tests on cadavers have also been performed by Haynes et al. [33], to analyze the phenomenon of cervico-cephalic screw scanning. The larger diameter of its screw shows that the use of Gamma™ nail seems to reduce the risk of sweeping compared to DHS.
Butt et al. [34] compared Gamma™ nail and DHS in a prospective study and reported a number of larger complications with Gamma™ nail, particularly femur fractures.
The rate of cut-out migration for first-generation nails averaged 3.1% according to Parker et al. [35].
Hoffmann et al. [36] found no significant difference in the management of pertrochanteric fractures between the Gamma™ nail and DHS.
In their meta-analysis, of all the randomized trials published comparing Gamma™ nail and DHS screw plate, Parker et al. [35] do not recommend using Gamma™ nail for trochanteric fractures. They showed that the Gamma™ nail significantly increased the risk of femoral fracture as well as the number of surgical revisions. Similarly, in a retrospective study of 1314 proximal femur fractures, Muller [37] found a greater number of fractures under nail PFN (2.1%) compared to DHS (0.5%). In our study, we noted one case of fracture under a Gamma™ nail which required its revision by a long Gamma™ nail.
Conclusions
Fractures of trochanteric region have an increasing incidence, with significant socio-economic impact. The
operative technique and the choice of the implant influence the functional and radiographic result. They
must essentially take into account whether the fracture is stable or not. The analysis of the literature shows
an advantage to the intramedullary nail in the short term, despite the risk of femoral fracture on nail. Our
study found no significant difference in bone consolidation and functional outcome at last follow-up, but it
confirms the superiority of Gamma™ nail in postoperative, due to lesser bleeding and earlier weight bearing.
Conflict of Interest
The authors declare that there is no conflict of interest relevant to this article.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!