Biography
Interests
Safaa Mahran, A.
Associate Professor Rheumatology and Rehabilitation, Assiut University, Assiut, Egypt
*Correspondence to: Dr. Safaa Mahran, A., Associate Professor Rheumatology and Rehabilitation, Assiut University, Assiut, Egypt.
Copyright © 2019 Dr. Safaa Mahran, A. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Rheumatoid arthritis (RA) is a chronic progressive autoimmune disease of unknown aetiology. It affects the synovial joints of the body with special predilection of the small joints of the hands and feet. Many other extraarticular manifestations do exist with affection of the skin, lung, heart, kidneys among others
Nervous system affection in RA could be central or peripheral. Central nervous system affection in RA may be due to cervical spine involvement by the rheumatoid pannus with the consecutive destruction of the supporting ligaments and bone erosions. Asymptomatic cervical spine involvement is reported in about 20% of RA cases. Cerebral vasculitis and optic neuropathy are rare manifestations.
Careful examination of RA patients for the presence of subclinical involvement of cervical spine and considering the central nervous system in these patients are mandatory to avoid the serious permanent sequels.
Introduction
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease of uncertain aetiology that primarily
targets synovial tissues. Although the clinical hallmark of RA is arthritis, many extra-articular manifestations could be encountered. Among these is the central nervous system affection.
Central nervous system affection of RA Includes cervical myelopathy, meningitis, focal neurological dysfunction and optic atrophy.
Cervical Myelopathy
Compression of the spinal cord at the cervical spine level is one of the serious extraarticular manifestation
of RA. In 1951, Davis and Markley detailed medullary compression as a cause of death in patients with
rheumatoid arthritis [1]. In 1969, Mathews reported that 25-30% of patients with rheumatoid arthritis who
were admitted to the hospital had radiographic evidence of cervical spine involvement [2].
Involvement of the cervical spine typically begins early in the disease process and often parallels the extent of peripheral disease.
Cervical involvement tends to be asymptomatic in the scenario of systemic rheumatoid manifestations.
The most common cervical affection in RA is atlantoaxial instability (AAI) with excessive movement at the junction between the atlas (C1) and axis (C2) because of either a bony or ligamentous abnormality.
There are several ways in which a subluxation can occur:
1-Anteroposterior subluxation: Anterior subluxation is the most common type of AAI, causes spinal cord compression with consecutive cord myelopathy. It occurs due to disruption of the supporting ligaments. Posterior Subluxation is less frequent than the anterior one and is due to erosion of the dens with high risk of cervical myelopathy than the anterior subluxation.
2-Rotatory subluxation, known as atlantoaxial rotatory fixation (AARF) is divided into four different types [3], type I: the atlas is rotated on the odontoid with no anterior displacement, type II: the atlas is rotated on one lateral articular process with 3 to 5mm of anterior displacement, type III: comprises a rotation of the atlas on both lateral articular processes with anterior displacement greater than 5mm and type IV: characterised by rotation and posterior displacement of the atlas.
3-Vertical subluxation with upward migration of the odontoid. It is serious and can lead to sudden death.
4-Lateral subluxation: Occurs in about 20% of RA cases and usually accompanies rotational subluxation [4].
Subaxial subluxation can also occur. It is usually secondary to destruction of the facet and discovertabral joints. It can occur at single or multiple levels leading to staircase deformity [5].
Patients with AAI may be presented with upper motor neuron lesion with weakness, exaggerated reflexes and incontinence. Manifestations of vertebrobasilar insufficiency with vertigo, tinnitus, loss of equilibrium, visual disturbances, and dysphagia can be also found.
Facial pain, auricular pain and occipital pain can result from compression on C2 sensory branches to the trigeminal tract, Greater auricular nerve and greater occipital nerve respectively.
The Ranawat classification [6] can be used to categorize patients with rheumatoid myelopathy:
Class I - No neural deficit, Class II - Subjective weakness, dysesthesias, and hyperreflexia, Class IIIA - Objective weakness and long-tract signs; patient remains ambulatory, Class IIIB - Objective weakness and long-tract signs; patient no longer ambulatory.
All RA patients should undergo routine cervical x-ray to detect the AAI which could remain asymptomatic for a long time.
For early diagnosis of AAI, a plain lateral cervical spine x ray in full flexion and full extension is needed.
The distance between the posterior border of the anterior arch of C1 and the anterior border of the odontoid process also termed atlantodens interval (ADI), is measured. (Fig 1) An interval of more than 3 mm in an adult or 4 mm in a child is considered abnormal. Some investigators have found that the AADI does not reliably discriminate between patients who are neurologically intact from those with neural deficit [7]. Taking into consideration the 3-dimensional changes that take place with progressive subluxation, this method might not be the ideal way for AAI detection.
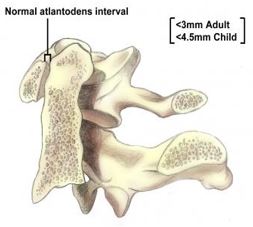
Boden and associates demonstrated this pitfall by examining the sensitivity, specificity, accuracy, and positive and negative predictive values of the AADI in predicting paralysis based on varying critical intervals [8].
Measuring the posterior ADI from the posterior edge of the odontoid to the anterior margin of the lamina of C1, was shown to be more sensitive than the traditional anterior measure [8]. Normal posterior ADI should be of 14mm or less.
Vertical subluxation (Superior migration of the odontoid/SMO) can be better assessed in lateral films taken in neutral position.
The McGregor line has become the most consistent reference, because it connects the posterior margin of the hard palate to the most caudal point of the occiput. (Fig 2) Vertical settling is defined here by migration of the odontoid by more than 4.5mm above this line.
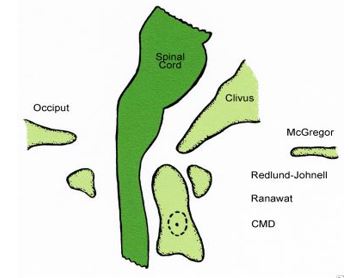
Other methods to assess the SMO include the Redlund-Johnell line, the Ranawat index, the McRae line and the Chamberlain line.
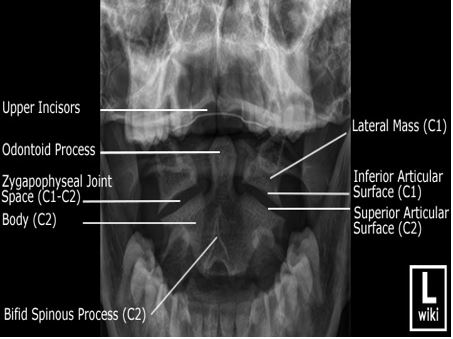
In lateral atlantoaxial subluxation, C1 is displaced laterally resulting in abnormal head posture. It is Diagnosed by an anteroposterior open-mouth radiograph, which shows involvement of one or both C1-C2 joints with a greater than 2-mm shift of C1 on C2 and tilting of C1 on C2. (Fig 3) The degree of tilting reflects the extent of the damage to the lateral mass of C2 [9].
Subaxial vertebral subluxations is diagnosed in lateral cervical radiographs as translation forward in millimetres or as a percentage slip of the total anteroposterior diameter of the inferior vertebral body. The sagittal diameter of the subaxial canal was found to correlate better with the presence and degree of paralysis more often than does the percentage of vertebral slip. Patients with canal diameters of 13mm or less are at higher risk for neurologic involvement.
Cervical spine computed tomography (CT) scanning and magnetic resonance imaging (MRI) are not routinely performed and are generally reserved for either extreme cases or situations of diagnostic uncertainty.
Proper assessment of the atlantoaxial joint is advisable in all RA patients undergoing general anaesthesia to avoid cord damage during intubation of head positioning [10].
Other less common CNS affection in patients with RA include aseptic pachymeningitis presented with aphasia and convulsions [11], Cerebral vasculitis presenting with headache and gait disorders [12] rheumatoid nodule formation [13] and cerebral arteritis presenting with headaches, focal neurological dysfunction and optic atrophy [14]. These pathologic changes could be diagnosed by MRI angiography, cerebral angiography and cerebrospinal fluid analysis.
Conclusion
In conclusion, cervical spine involvement in RA ranges from being asymptomatic to cervical cord myelopathy.
Careful history taking and physical examination in patients with RA should done for early detection of
CNS manifestations.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!