Biography
Interests
Ray Marks
Departments of Health, Physical Education & Gerontological Studies and Services, City University of New York, York College and Health and Behavior Studies, Columbia University, Teachers College, New York, USA
*Correspondence to: Dr. Ray Marks, Department of Health and Behavior Studies, Teachers College, Columbia University, New York, USA.
Copyright © 2018 Dr. Ray Marks. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Osteoarthritis, a widespread highly painful oftentimes incapacitating joint disease with few efficacious remedies continues to pose immense personal and societal challenges on a large scale in an aging population. In absence of any effective cure or treatment for this condition, this brief was designed to update the reader as to whether anxiety, a widespread psychological syndrome affecting many adults, remains an underestimated contributor to osteoarthritis disability. Drawn from the prevailing peer reviewed data sources in the leading electronic data bases, using the keywords osteoarthritis and anxiety, detailed are some recent research observations published predominantly between the years 2014-2018 in this regard. Although not extensive, nor amenable to any systematic analysis, the search revealed that anxiety is indeed often present among sizeable numbers of osteoarthritis cases, and its presence appears to have a multitude of negative health effects at all disease stages. Consistent with prior reports on this topic, it is concluded that the topic of anxiety, which may play a bi-directional role in influencing disease outcomes, warrants attention as a potentially clinically relevant disease predictor or outcome variable on a more consistent basis. Moreover, where present, multidisciplinary follow-ups and tailored treatments may enhance overall well-being, and prevent excess disability, regardless of joint[s] affected and their severity or status.
Background
Osteoarthritis, a highly prevalent health condition affecting many older adults commonly produces varying
degrees of local joint and bone pain, as well as muscle and soft tissue pain consequent to progressive destruction
of the cartilage tissue lining one or more freely moving joints, as well as its bone surfaces and surrounding
tissues, along with heightened central sensitivity to pain, if the condition persists. Often heightening the risk
for-or concurrently associated with other chronic health conditions [1], most notably, cardiovascular diseases
and obesity, as well as varying degrees of inflammation, and considerable activity limitations, treatments for
this condition continue to focus largely on pharmaceutical drugs that are often toxic with detrimental side
effects, alongside the likelihood of joint replacement surgeries, which are often associated with short and
long term complications, and a general failure to fully restore mobility or eliminate pain. However, while
this disease clearly has several physical components, the viewpoint that osteoarthritis is predominantly
a biomechanical disorder associated with aging, may be one reason why physical treatments applied in
isolation do not always ameliorate the prevailing pain or disability of osteoarthritis at all successfully.
Given that a linkage between pain and anxiety is a prevalent one in the mainstream literature, along with knowledge that cognitive status or emotional states can impact health decisions and health behaviors, and that anxiety is highly prevalent among adults in general, and among adults with a variety of medical disorders [2] and chronic physical conditions, in particular [3], it seems plausible to continue to examine if anxiety is a potentially important, albeit underestimated osteoarthritis disease disabler or a determinant that warrants more careful and consistent attention. In particular, if the observation by Gay et al. [4] that the osteoarthritis population is less active, and more sedentary, with higher numbers of comorbidities and more barriers to physical activity practices than the overall population is potentially related in some way to the presence of unidentified and treated anxiety, addressing this correlate may arguably foster more opportunities to reduce disease outcomes due to inactivity, feeling overwhelmed, catastrophizing, and excess comorbidity than standard approaches.
Aims
This work aimed to update our knowledge base of this topic as this pertains to the wellbeing of the older
adult diagnosed with osteoarthritis. The key question driving this updated work was whether a reasonable
body of updated literature continues to support the idea of implementing some routine examination that
would identify the presence of excess or unwanted anxiety levels among osteoarthritis cohorts, regardless
of setting. Another was whether osteoarthritis pain and disability are likely to be affected by the presence
or absence of anxiety in a significant way and to what degree. Another was whether it would be possible to
limit, prevent, or minimize anxiety where it exists among osteoarthritis cases, regardless of disease status.
Methods
To obtain representative salient publications that might provide relevant peer reviewed data, the PsycINFO,
PUBMED, Scopus, Science Direct, and Web of Science consolidated data bases over the last five years
[January 2014-August 2018] were explored using the search terms anxiety and osteoarthritis. The items
retrieved were carefully examined and selected for discussion only if they addressed one or more of the study questions. Selected data extracted from this data base were then scrutinized and summarized largely in
narrative or tabular formats if they appeared to assist in answering the review questions. That is, recent studies
that focused on exploring the extent to which anxiety appears to prevail among adults with osteoarthritis
were specifically sought, along with studies that showed either an important clinical association with the
disease or did not demonstrate this. Interventions recommended for ameliorating excess anxiety in the face
of chronic osteoarthritis, and gaps in the literature were also specifically sought and reviewed.
This mini review did not differentiate articles examining trait anxiety from state anxiety, or focus on any specific form of osteoarthritis, and given the limited data base, all forms of research design were deemed acceptable. Excluded were foreign articles, incomplete reports, reports older than 6 years, and those that examined mixed cohorts of arthritis. The term anxiety, a psychological disturbance representing a form of emotional distress, was employed in a generic sense throughout to represent all three variants of clinical anxiety, generalized anxiety disorder, state anxiety and trait anxiety, rather than their unique and differential effects in the context of the disease. Readers seeking a prior update on this topic are referred to reference [5].
Results
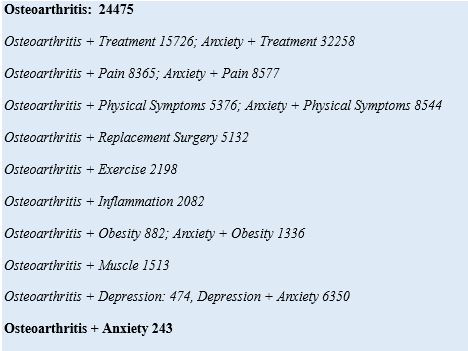
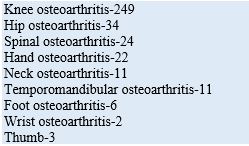
Despite the possible utility of studying anxiety in the context of osteoarthritis, this mini review found
very few studies specifically focused on anxiety as a clinically important osteoarthritis disease correlate,
especially when compared to other topics [See Box 1]. Moreover, as shown in Box 2, almost no data on
this topic prevail for joints other than the knee and hip, which have for example 244 and 94/500 articles
specifically listed from 1980-on PUBMED, with 22 or less for all other joints that can be affected, in this
context. Similarly, targeted intervention studies were not readily available, and even if proposed, have not
been conducted, or remain pilot or incomplete studies. However, of the articles published over the last five
years, a small number, do appear to stress some important and valuable clinical and research related points
that warrant consideration in our view, even if this is only due to selection bias, where negative studies are
often not widely published. The Hospital Anxiety and Depressions [HAD] and Spielberger Anxiety Scales
were most commonly used, even though these do not prove anxiety is clinically present. Other self-report
instruments used were the Beck Anxiety Scale, the Mental Health Inventory, or anxiety assessed using a
single question.
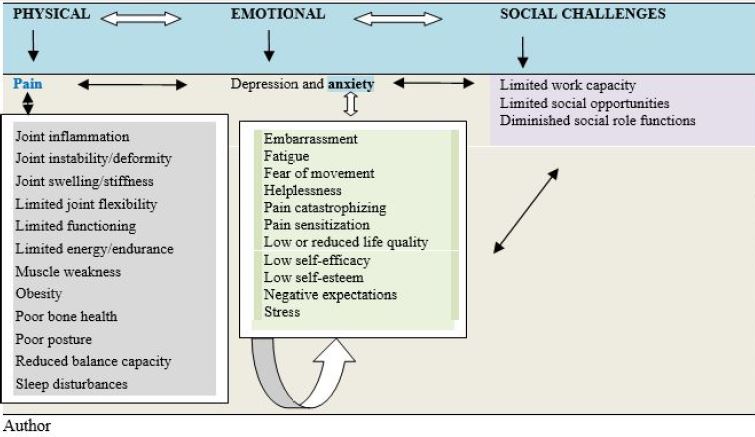
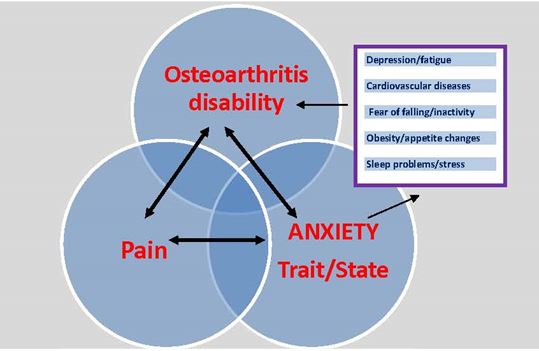
As outlined in relatively recent studies, for example, that by Tan et al. [6] and consistent with earlier studies,
for example, that by Murphy et al. [7], the presence of a state of anxiety appears quite common in the context
of osteoarthritis, regardless of how this is assessed. Additionally, where anxiety exists, the condition often coexists
with depression [5], along with other long-term health conditions. In addition to that, those suffering
from anxiety alone, or anxiety and depression are also more likely than not to suffer from chronic pain or
excess chronic pain, among other factors [see Figure 1]. As well, even though Kang et al. [8] negated a role for anxiety in terms of trapeziometacarpal arthritis, and anxiety was not mentioned as a pain correlate by
Heidari et al. [9], the presence of anxiety, alone or in combination with other health conditions, is consistently
found to reduce health-related quality of life and to manifest in poorer clinical outcomes for all comorbid
conditions, including osteoarthritis. Anxiety is also a significant clinical feature of knee osteoarthritis [10],
especially among women [11], as well as a consistent predictor of total joint arthroplasty outcomes [12],
including an increased risk of post-operative complications [13], and levels of experienced pain [14], and
possibly centralized osteoarthritis pain [15]. Findings by Nazarinasab et al. [16] who studied 94 patients
with osteoarthritis, 30 male patients (31.9%) and 64 female (68.1%), showed that 58.5% of these patients
had a mental health disorder including anxiety. In addition, the prevalence of mental health problems in
their osteoarthritis groups was significantly higher in the age range of 18 to 20 years old (p = 0.002) than in
older cases, and in the first months of diagnosis. Patients taking corticosteroids also appeared at high risk for
mental health disorders including anxiety (p = 0.00).
In a related study, Nur et al. [17] similarly confirmed anxiety to be among the factors contributing to knee pain and function in women with knee osteoarthritis. Barnett et al. [18] likewise found adults with joint pain reporting clinical anxiety, were quite numerous, in general, and were those more likely to exhibit severe, rather than mild pain. It was further observed that the number of pain sites was also positively associated with the presence of clinical anxiety, and that those adults with symptoms of clinical anxiety appeared less likely to undertake general fitness exercises. They were also more likely to use walking aids and assistive devices, plus opioids than non-anxious adults with joint pain. While not universally present among osteoarthritis cases, Jones et al. [19] found 44 percent of knee replacement surgery cases were clearly anxious as deduced by a 14 item self-reported survey. While this high number of cases may have been due in part to the method of calculating anxiety as normal or abnormal in that study, Wong et al. [20] as well as Castano et al. [21], Stubbs et al. [5] and Guglielmo et al. [22] reported the presence of anxiety to be of the order of 20 percent or higher in various osteoarthritis or arthritis samples where this has been examined. Moreover, anxiety levels were elevated in community dwelling knee osteoarthritis cases compared to the general population [23], and where present, these anxious osteoarthritis patients had higher pain levels at rest and on activity than non-anxious patients. Bierke et al. [24] found rates of trait anxiety alone to be approximately 14 percent among cases with disabling osteoarthritis awaiting treatment, suggesting a number of osteoarthritis patients may not only suffer from state anxiety, which is understandable, but from a generalized anxiety disorder or a form of chronic anxiety. Importantly, those identified as having a habitual pattern of anxiety behavior had higher mean dissatisfaction scores at 6 and 12 months after surgery than those with no anxiety. Khan et al. [11] similarly found high levels of anxiety among osteoarthritis cases compared to non-osteoarthritis cases, especially among women.
According to Harmelink et al. [25] and others such as Liddle et al. [26], even if anxiety rates are deemed acceptable or clinically unimportant, acknowledging the presence of any form of anxiety is arguably very crucial in osteoarthritis remediation efforts in light of the fact that unrelieved anxiety can be expected to impact the pain experience quite negatively and significantly [27,28]. As well, unrelieved anxiety can potentially exacerbate harmful chronic oxidative stress levels and inflammatory responses [29], while markedly reducing daily activity participation rates [30], and functional ability [23]. Research in the surgical realm further shows the presence of anxiety can delay healing, while reducing satisfaction with the surgical results [31], and impeding attainment of anticipated functional benefits [19,32-36]. Anxious patients may also be more reluctant to participate in optimal forms of exercises or processes at restoring fitness, and especially after total joint replacement surgery may experience a lower subjective assessment of the possibility of any return to work during the lengthy post-operative rehabilitation period and readiness to undergo treatment [37]. Although Janikowska-Holowenko et al. [37] found the subjective assessment of pain after post-surgical rehabilitation was not significantly associated with anxiety as a trait, and no connection was found between anxiety and subjective assessments of physical activity, the assessment of pain was correlated with the level of anxiety after secondary rehabilitation. Hernandez et al. [38] who conducted a systematic review of 37 studies concluded that pre-surgical anxiety does indeed influence post-operative pain in a consistent manner. It also impacts life quality negatively and significantly [39,40], as well as sleep [41], the onset or perpetuation of neuropathic pain [27], pain intensity and pain distress [42], and non-surgical multidisciplinary treatment outcomes [43].
Indeed, data show that even where anxiety rates can be considered to be quite low, the presence of anxiety still has substantive negative implications for the osteoarthritis patient [44,45]. Conversely, Helminen et al. [46] who employed the Beck Anxiety Inventory to examine the severity of anxiety found adults with knee osteoarthritis with lower anxiety symptoms had better pain outcomes and function over a one-year followup of joint replacement surgery as did Hassett et al. [47].
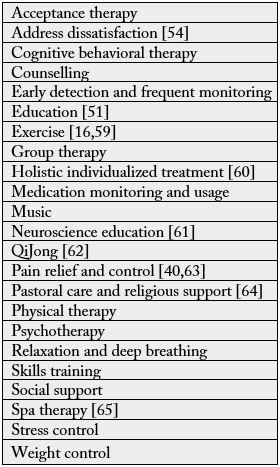
Unfortunately, despite these potentially relevant findings that concur quite strongly with others that precede them, recent community-based efforts to address and treat anxiety among osteoarthritis cases were deemed largely unsuccessful in this regard [48], did not substantially reduce patients’ pain and disability [49], and in the realm of cost-effectiveness, were not effective [50]. However, as pointed out by Hirakawa et al [51], and other researchers highlighted in Table 1, at a minimum, efforts to uncover and reduce persistent and oftentimes pervasive negative thoughts regarding future pain among osteoarthritis cases scheduled for total joint replacement surgery remain warranted in efforts to limit delays in returning to work, the onset of low self-efficacy beliefs, and lower than desirable overall life quality [52]. Unfortunately, the interventions that might help to minimize, avert, or prevent anxiety among cases with osteoarthritis are not well studied-thus claims that intervention does not benefit subjects cannot be made with any robust certainty at the present time. The optimal time course for those behavioral and other interventions recommended for minimizing anxiety related problems outlined in Table 2-is also unknown.
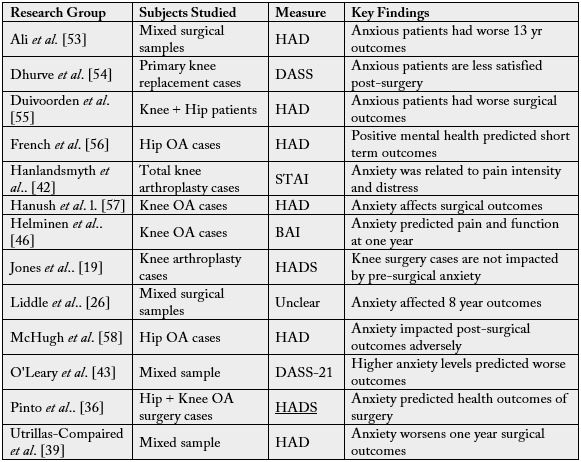
BAI-Beck Anxiety Inventory; DASS-Depression, anxiety and stress scale; STAI-State trait anxiety inventory; HADS-Hospital Anxiety and depression Scale; OA=osteoarthritis
Discussion
Osteoarthritis, a highly prevalent health condition remains a serious impediment to many older individuals
who seek to remain independent and mobile. This mini narrative review, which examined recent evidence
concerning the possible role of anxiety, a highly prominent psychological condition in its own right among
older adults was undertaken in an effort to evaluate the status quo concerning the topic of anxiety in
potentially playing a significant role in mediating, moderating, or exacerbating osteoarthritis disability. As
an osteoarthritis correlate that been examined quite recently, this mini review was specifically focused on
data that has emerged in the past five years or so in the key data bases believed to house state of the art and
gold standard articles on this topic.
Results showed that while still limited, and much less studied than either topic alone and others, these data were generally consistent with similar previous literature that concluded this realm of endeavor holds promise and needs more careful exploration.
However, even though the current evidence base tended to support the value of previous recommendations to screen the osteoarthritis patient for anxiety, and to treat this as indicated more routinely, this view is by no means conclusive, or universal. Limiting the progress made in this field are clearly the lack of well-designed longitudinal studies that focus on osteoarthritis samples other than surgical candidates, or in the context of joints other than the knee or hip [See Box 2 and Table 1]. At the same time, those that have examined anxiety in the context of osteoarthritis do not follow any consistent research design, and often employ mixed samples, and diverse data collection procedures, precluding any meaningful synthesis. The additional failure to examine whether anxiety if present, is a longstanding intrapersonal trait or whether it is a reactive state as a result of the disease or both, further clearly impedes the emergence of any unified understanding of the implications of anxiety in its diverse forms among various stages and degrees of disabling osteoarthritis. As well, the mechanisms whereby anxiety can impact osteoarthritis disability and what its unique determinants are in this respect are also very poorly defined, despite the potential importance of this information.
These research related limitations, and others, which have now persisted for at least three decades according to conclusions reached by several researchers are undoubtedly extremely disappointing given the failure of most current approaches to ameliorate osteoarthritis disability safely and effectively, and the fact anxiety is a modifiable disease correlate. They are especially disadvantageous for improving the outlook for adults with osteoarthritis in our view for at least two reasons. First, because anxiety may not always be favourably impacted by standard pharmacologic and surgical approaches used to treat osteoarthritis, and indeed may be associated with the excess intake of a variety of over-the-counter, or prescribed potentially addictive or harmful medications. Second, and most importantly, this omission arguably increases the extent of the prevailing disability experienced by a sizeable number of osteoarthritis sufferers, while diminishing or retarding the achievement of anticipated goals of remediation [66-72].
They also imply that distressed osteoarthritis cases who remain untreated may have worse functional scores than those with no anxiety [52,73,74], as well as higher perceived levels of current and forthcoming pain [69,75-79], plus lower local pain pressure thresholds [76].
Additional data show that untreated or unrecognized anxiety routinely leads to delayed healing, and attainment of optimal post-surgical outcomes [23,37,51,68]. Osteoarthritis patients who suffer from excess untreated anxiety may also be at a heightened need for arthroplasty revision surgery [26]. They can also be expected to experience a lower than necessary life quality [37,60], and diminished responsiveness to standard interventions, along with the heightened risk of acquiring subsequent chronic health conditions [15], states of physical inactivity and sedentary behaviours [78].
Other data reveal osteoarthritis patients suffering from concomitant anxiety may be vulnerable to excess opioid usage [18], fear-avoidance versus active resolution strategies, sedentary behaviors that could contribute to weakness and joint instability [80], and failure to attain exercise benefits- the most frequently prescribed osteoarthritis self-management remedy [81]. The enormous associated social and fiscal costs associated with a failure to address anxiety in a timely way are surely incalculable as well.
In addition, potential causes and predictors of anxiety such as other medical illnesses, pain, factors in the environment, including the subjects’ physical, psychological and dietary environment, obesity, having limited health insurance and having low perceived health and high levels of disability [73] are rarely examined in a systematic way despite their bearing on the resultant disease prognosis and treatment recommendations as was discussed 10 years ago by Smith and Zautra [77]. There is also almost no evidence to guide the clinician as far as best intervention practices for ameliorating anxiety go and whether a possible reduction in the extent of osteoarthritis disability will accrue through a timely anxiety diagnosis and its subsequent treatment.
Unfortunately, even where anxiety is examined clinically, results may be confounded if they include simultaneous measures made to rheumatoid arthritis patients [39], patients with hip fractures, osteoporosis, or back pain, and correlates of depression [26,57], and mixed forms of osteoarthritis, known to have differential outcomes [12]. As well, there are very few hypothesis testing research designs that provide salient follow up data [75], and among those that do, most are unable to clearly establish if anxiety is a key outcome determinant and to what degree given the questionable reliability of the presently documented anxiety, function, or pain measures [19]. Subject to error, under reporting, over reporting, inadequate reporting, lack of methodologic collection rigor, and misclassification because anxiety is usually assessed through self-reported data survey estimates, the present anxiety estimates and their relationships with other self-reports are insufficient for purposes of producing compelling evidence and advancing more universal consensus concerning the clinical significance of anxiety as a possible highly relevant osteoarthritis outcome determinant.
In short, although a case for examining anxiety in the context of routine osteoarthritis care has prevailed for some time [68-69, 82] and this call for a more consistent focus on this correlate in the realm of treatment is continuing [eg 43,68], the weaknesses of most prevailing and past studies, including their limited numbers, along with the relative absence of longitudinal studies that examine anxiety presence and any possible long-term functional as well as structural disease relationships among clearly defined osteoarthritis cohorts, greatly limits acceptance of the rationale for recommending this line of action as a standard clinical approach, regardless of disability status. It also limits understanding of the cause-effect relationship between osteoarthritis pain and anxiety-and its resultant omission in the therapeutic treatment realm may simply increase-rather than decrease- in the face of prevailing undetected anxiety levels. As well, what the most profound determinants of anxiety are relative to osteoarthritis, such as whether these stem from body image concerns, functional concerns, fear, perceived diminished control, financial factors, and limited ability among other factors remains unknown.
The present observations are disappointing, because in terms of the conceptual model presented in Figure 1, and the possible cost savings and heightened well-being alone that could be realized by comprehending this potentially relevant set of clinical factors, one can anticipate that excess suffering will prevail among millions of older adults with osteoarthritis whose anxiety states remain undiagnosed and untreated. Sufficient evidence of a possible consistent link to the osteoarthritic patients’ overall pain experience, plus their life quality and ability to carry out self-care actions, including exercising motivation [63] alone are valuable factors to consider in efforts to reduce the immense burden of this disease. Less anxious patients may also sleep more soundly, and experience less depression, risk of acquiring comorbid medical conditions, and drug dependence [83]. The osteoarthritis patient who is able to remain calm or is calmed appropriately despite their disabling health condition may also be more willing to undergo reconstructive surgery earlier-rather than later-when they stand a better chance of success, and returning to work, rather than only agreeing to undergo surgery when the condition is very severe, and their heightened anxiety state limits their overall chances of a successful physical and social as well as emotional outcomes [24].
Conclusion
Although recent and past research provides a tentative rationale and degree of support for routinely examining
and treating the correlate of anxiety in the context of osteoarthritis care, it is concluded that more robust
research efforts are needed to solidify this idea.
To this end given the potential importance of unravelling the role of anxiety in the osteoarthritis disease process, as conceptually illustrated in Figures 1 and 2, it is concluded extensive interdisciplinary research efforts, rather than stand-alone efforts are desirable.
It is also concluded that to further advance the knowledge base examining anxiety in the context of various osteoarthritis, validated anxiety assessment instruments coupled with quantitative sensory testing [68] is imperative. Sorely needed as well are carefully controlled studies that evaluate the relative efficacy of various forms of treating anxiety, where it exists among diverse osteoarthritis cases. In addition, examining the voices of sufferers through qualitative approaches and if any attendant excess anxiety accompanying this painful disease can be reduced or prevented by employing an empathetic and holistic approach on the part of the provider [60,84] appears warranted.
In the interim, as per Figures 1 and 2, plus Table 1, it can be tentatively concluded that this topic warrants more attention to assess the value of routine screening [7], and -where apparent- what its treatment implications are [24,25,74]. In addition, whether following up on routine screenings of the osteoarthritis patient deemed at risk for state or trait anxiety or both, is efficacious or not in attenuating the burden of the disease should be examined [12,30,67,75,78].
Alternately, it is concluded that failing to carry out concerted future research efforts in this realm will preclude a considerable number of older adults with this disease from attaining a high life quality and maximum available treatment benefits. On the other hand, efforts to broaden and solidify the knowledge base regarding anxiety across the time course of the disease, and to resolve negative study findings [85-87], and to do this sooner rather than later may yield significant long-term social and fiscal benefits, even though short term costs of doing this may be substantive [88,89].
In particular, specific attention to examining anxiety and its causes as a potentially highly relevant therapeutic target in the context of various forms of osteoarthritis, which has not been well examined, along with careful consideration to minimize confounding factors in related studies should be forthcoming [76].
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!