Biography
Interests
David M. Burt, MD1*, Chris E. Stout PhD2,3, Lindsey Loughran ATC4 & Grace A. Wang BA3
1Midwest Sports Medicine Institute, USA
2University of Illinois at Chicago, USA
3ATI Physical Therapy, USA
4Grand Canyon University, USA
*Correspondence to: Dr. David M. Burt, MD, Orthopaedic Sports Medicine Surgeon, Midwest Sports Medicine Institute, USA.
Copyright © 2018 Dr. David M. Burt, MD, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
To examine return to overhand sports and level of play in a cohort of young, elite, female, overhand
athletes after arthroscopic repair of type 2 SLAP lesions, as most of the literature focuses only on
male baseball players.
A case series in which we retrospectively reviewed 12 young, elite, female, overhand athletes at the
high school, club, and college levels who underwent arthroscopic repair of a type 2 SLAP lesion.
Average age at surgery was 16.25 years (range 15-19 years). Four athletes underwent debridement
of a partial rotator cuff tear at the time of SLAP repair. Outcomes were measured using the Kerlan
Jobe Orthopaedic Clinic Shoulder and Elbow (KJOC) score and the American Shoulder and
Elbow Society (ASES) score. Independent Sample t-tests were used to evaluate differences in
scores for those who did and did not return to sport, the effects of concomitant partial rotator cuff
tear, number of anchors used, and type of sport.
At an average of 32 months, ten of twelve (83%) patients were able to return to play at the same or
higher level. The average KJOC score for athletes who returned to sport was 69.2/100 compared to
37.6/100 for those who did not. This was statistically significant (p=.017). Mean ASES for those
who returned to play was 87.55/100 versus 67.39/100 for those who did not, and did not reach
statistical significance (p=.26). Debridement of a partial rotator cuff tear, type of sport, or number
of anchors used did not correlate statistically with differences in KJOC or ASES scores, or athlete’s
ability to return to overhand sports.
After failed conservative care, arthroscopic repair of a type 2 SLAP lesion is a viable option with
a high success rate for return to play in young, elite, female, overhand athletes who wish to remain
active in their sport.
Introduction
Glenoid labrum lesions were described in 1983 by Pappas et al. [1] as a source of mechanical symptoms
and instability in the shoulder as seen in open surgery, and further identified arthroscopically by Andrews
et al. [2] in 1985. Snyder et al. [3] then published their arthroscopic classification of superior labrum from
anterior to posterior (SLAP) lesions in 1990, noting the type 2 lesion to be most common.
Overhand sporting activities are among the most common causes of SLAP lesions in the shoulder [2], and this is consistent with the significant forces occurring about the shoulder during movements such as throwing or overhand hitting [4-6]. Various mechanisms of injury have been identified, ranging from traumatic to overuse. Specific biomechanical factors predisposing to superior labral tears have also been described, including longitudinal traction of the biceps [2], compressive force [3], and torsional force acting at the biceps/labral complex causing a “peel-back” phenomenon [7].
Anatomical factors such as poor vascularity of the superior portion of the labrum may prevent spontaneous healing, even after cessation of overhand activity, thus necessitating operative intervention in those who fail non-operative management [8-11].
In the presence of a type 2 SLAP lesion, an overhand athlete often can no longer perform at their previous level of competition [12]. According to Edwards et al. [11] only 63% of competitive overhand athletes with SLAP lesions return to pre-injury or higher level of competition without surgical intervention, despite high scores on American Shoulder and Elbow Surgeons scores (ASES). Recognizing this mismatch between ASES score and return to play, Alberta et al. [13] designed and validated the Kerlan Jobe Orthopaedic Clinic (KJOC) outcome assessment tool to address more specifically the return to play and performance ability in the overhand elite or competitive athlete. Use of this outcome measure to evaluate return to overhand sports has been further validated [14-16], and was utilized in the current study.
Arthroscopic SLAP repair may help to prevent further glenohumeral instability especially in young, overhand athletes [17,18] allowing a return to competitive overhand sports. Therefore in the setting of failed conservative care, including rest from sports and a comprehensive rehabilitation program, surgical repair remains the only viable option for athletes wishing to return to overhand sports [19]. And while many authors report successful results after arthroscopic repair of type 2 SLAP lesions across a wide range of age groups and activity levels in general [10,17-23]. Closer analysis of studies that contain younger competitive overhand athletes reveals mixed results for ability to return to play. Reported levels of return to play after SLAP repair may vary in these studies from as low as 22% to 38% [24-26] to as high as 75% to 84% [16,27,28].
Furthermore, the majority of the currently available data on young, competitive overhand athletes after SLAP 2 repair is focused on male baseball players. Data reporting on young female athletes is lacking in the literature, yet the participation rates, intensity levels, and emphasis on year-round sports among female overhand athletes have all increased, leading to a higher incidence of SLAP tears [29-32]. As with their male counterparts these young women desire to be competitive in their sports after treatment. This presents surgeons with a difficult treatment challenge given that the prognosis for return to play with non-surgical treatment is relatively low [11], and prognosis for return to play after SLAP repair in this cohort of young, elite, female, overhand athletes is not clearly established in the literature. The purpose of this study was to determine whether young elite female overhand athletes could return to sport at the same or higher level of competition after arthroscopic repair of a type 2 SLAP tear. We hypothesized that arthroscopic repair of type 2 SLAP lesions would provide sufficient improvement in pain and function to allow return to the same or higher level of play in the majority of study participants.
Materials and Methods
After approval from our institutional review board a retrospective chart analysis was performed identifying
16 young, elite, female, overhand athletes who had undergone arthroscopic repair of a type 2 SLAP lesion
between July of 2007 and September of 2013. Sample size was determined by the population of surgical
patients that met criteria. Inclusion criteria were as follows: female, overhand athlete, age 25 or younger,
presence of a type 2 SLAP tear diagnosed at surgery, and failed conservative management for a minimum of 3 months preoperatively. Exclusion criteria included: age greater than 25 years, male, rotator cuff repair,
frank dislocation or bankart lesion, prior shoulder surgery, or clinical evidence of multidirectional instability.
Outcomes measurements utilized were the Kerlan Jobe Orthopedic Clinic (KJOC) score and the American
Shoulder and Elbow Surgeons (ASES) score. KJOC and ASES scores were categorized identically with
“excellent” being a score range of 90-100, “good” 80-90, “fair” 70-80, and “poor” below 70.
Between July of 2007 and September of 2013, 141 patients underwent arthroscopic repair of a type 2
superior labral tear by the senior author. After retrospective chart review 16 patients were identified who met
the above inclusion criteria. Four patients who met inclusion criteria were unable to be located after utilizing
extensive measures to attempt to contact them including phone, cell phone, email, US mail, and internet
search. This left 12 patients to comprise the study group for a final participation rate of 75%. Average age
of this group at the time of surgery was 16.25 years (range 15-19 years). Ten athletes at the time of surgery
were high school and elite club level, and two athletes were playing competitive college sports at the time
of surgery. Of those who returned to play post-surgery three advanced to college level and two remained at
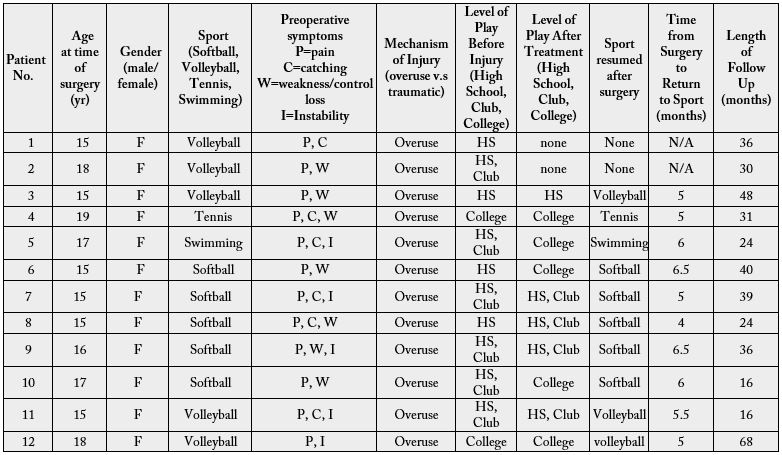
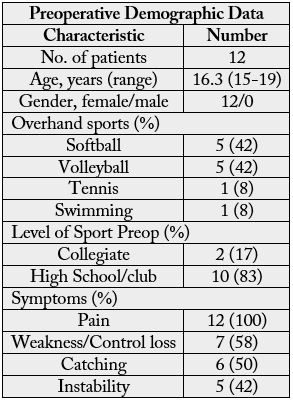
the college level, while the others remained at the high school and elite club level. (Table 1) Five athletes
were softball players of which two played catcher, and three were position players. Five athletes played
volleyball, of which three were outside hitters, one was a middle hitter, and one played Libero. One athlete
was a tennis player with surgery performed on the right dominant shoulder, and one swimmer underwent
surgery on her right dominant shoulder. (Table 2) All patients in the study underwent surgery on their
dominant shoulder. History and physical examination were performed on all patients including evaluation
of range of motion, strength, and laxity testing. No patients demonstrated any evidence of multidirectional
instability on exam and all patients in this series did show a positive active compression test (O’brien’s)
[33] on physical exam. Plain radiographs were obtained in all cases and none were found to have any bone
pathology or degenerative changes. All patients were suspected to have superior labral tearing based upon
history, physical exam, preoperative MRI-arthrogram, and all tears were confirmed at surgery. All athletes
in the study participated in physical therapy for a minimum of three months pre-operatively. In all cases the
etiology of symptoms was determined by history to be atraumatic and as a result of repetitive overuse of the
shoulder from overhand sports. No patients reported a specific traumatic event. Symptoms included pain,
catching, instability, loss of control, loss of speed, and loss of strength in the involved shoulder (Table 2).
At a mean follow-up of 32 months (range 16-68 months) 12 elite female overhand athletes were evaluated.
Eleven of twelve athletes in the final study group were available in person for questionnaires and physical
examination and one athlete submitted questionnaires by mail. Physical exam portion of the ASES was
performed by an independent examiner who is a certified athletic trainer. Range of motion was measured
with hand-held goniometer, measuring external rotation with both the arm at the side and at 90 degrees of
abduction. In addition forward flexion was measured, and internal rotation was measured at 90 degrees of
abduction. Athletes were asked to fill out the ASES and KJOC questionnaires.
The ASES score was obtained from the subjective portion of the questionnaire utilizing the published formula [34], which derives a score out of 100 from the visual analog pain scale and functional ability questions. The KJOC assessment tool is a self-reported subjective 2-part questionnaire which has been validated by Alberta et al. [13] The first section allows athletes to establish if they are playing pain free, playing with pain, or not playing due to pain. Current and highest levels of play are also reported in this section, and this information was used in comparison to each athlete’s known pre-injury level of play (high school, club, collegiate) to determine if they reached the same, higher, or lower level of competition after arthroscopic repair. The second section is comprised of ten visual analog scale questions of ten points each relating to overhand sport performance for a total possible score of 100, with higher scores indicative of better or higher performance.
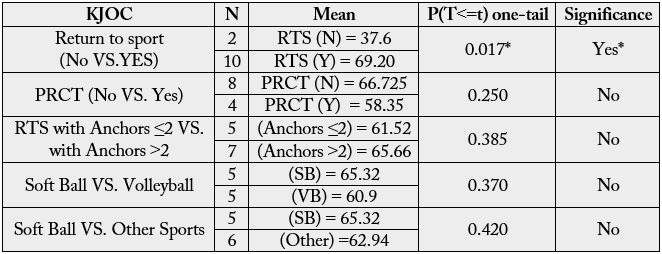
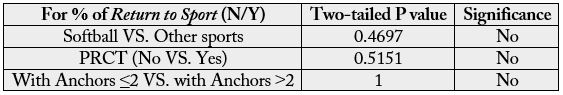
In order to compare the means between two independent groups (e.g., soft-ball versus volleyball athletes),
Independent Samples T-tests (Microsoft Excel 2010, Redmond, WA) were used. This was done for both
KJOC (Table 3) and ASES findings (Table 4).
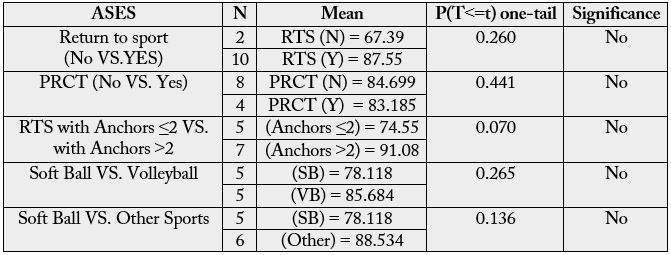
To compare the difference of proportions of return to sport among various classifications (e.g., number of anchors used, presence or absence of partial rotator cuff tear, type of sport) Fisher’s Exact Tests were used to perform probability testing (VassarStats, http://vassarstats.net/tab2x2.html, Poughkeepsie, NY, Richard Lowry) (Table 5).
All repairs were performed arthroscopically in the lateral decubitus position by a single surgeon under general
anesthesia and augmented with interscalene block. Prior to lateral positioning all patients underwent exam
under anesthesia. The shoulders were placed through full range of motion, specifically forward elevation,
external rotation arm at the side, and internal and external rotation at 90 degrees of abduction. Inferior
translation was measured by means of Sulcus testing. Anterior and posterior laxity was measured by manual
translation of the humeral head on the glenoid at varying degrees of abduction and rotation. No shoulders
demonstrated any degree of pathologic laxity on exam under anesthesia. The arm was placed into balanced
suspension with ten pounds of traction, 45 degrees of abduction, and 10 degrees for forward flexion. Standard
posterior and anterior-superior portals were made in all cases. As needed in some cases, an anterior-inferior
portal was made for suture management and in all cases a posterolateral Port of Wilmington [35] was made
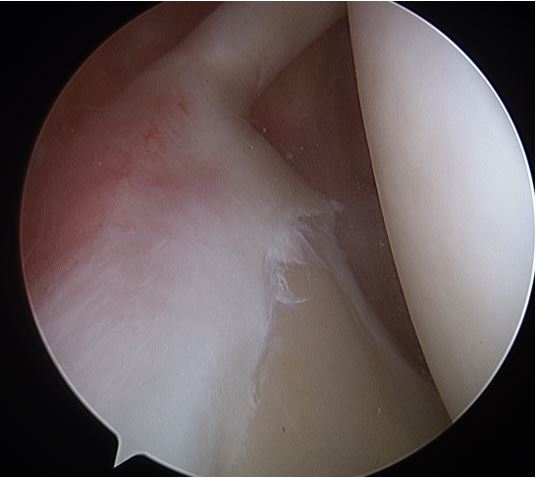
to affect the appropriate trajectory for placement of posterior-superior anchors. Diagnostic arthroscopy
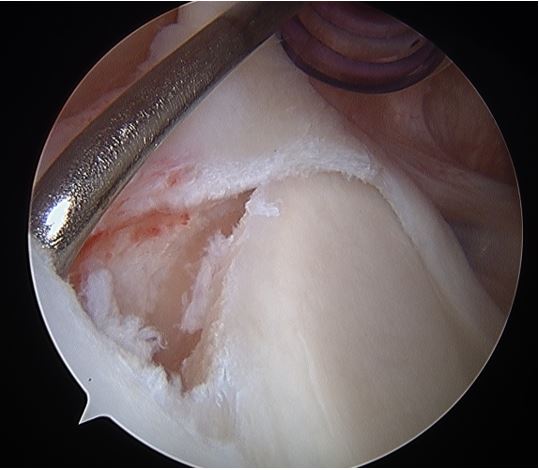
was performed assessing the glenohumeral joint, capsule, rotator cuff, labrum, and biceps tendon. Four of
twelve athletes were found to have a partial rotator cuff tear (PRCT) at the articular margin of the mid to
anterior supraspinatus. These ranged in size from 10% to 20% thickness as measured by loss of footprint
attachment from the articular margin with a calibrated probe. All four of these patients underwent standard
debridement with a motorized shaver. Any full thickness tears or tears greater than 50% were repaired and
thus excluded from the study group. Diagnosis of a type 2 SLAP tear was made based on the presence of
instability of the superior labral- biceps complex in the form of either an observed arthroscopic peel-back
during abduction and external rotation intra-operatively [7], a labral-glenoid junction gap at the superior
labrum that was unstable to probing and into which a probe or elevator type of instrument could be easily
placed, or a grossly unstable superior labral-biceps complex by either probing or intraoperative humeral
rotation.
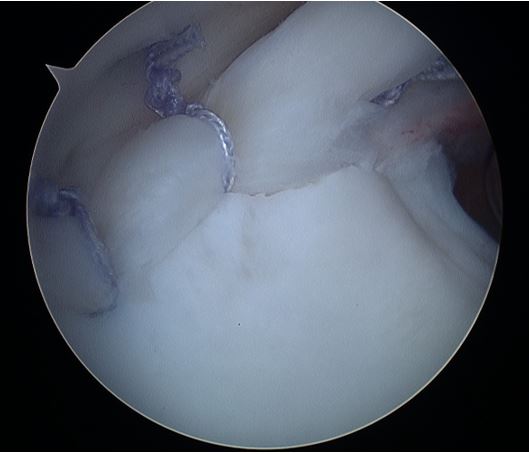
Once identified, the glenoid margin under the tear was prepared to bleeding bone with a motorized shaver. Suture anchors (Arthrex, Naples, FL) loaded with single #2 non-absorbable suture were used. The average number of anchors used was 2.6. Simple suture configuration was used for all cases. For standard anchors, a simple sliding knot was used with 3 alternating half-hitches to achieve good loop and knot security. In some cases knotless anchors were used with proper tensioning of the suture at time of anchor deployment for loop security. Two or three anchors were placed posterior to the biceps tendon, and in some cases a single anchor was placed just anterior to the biceps tendon depending on the extent of the tear. At the end of the procedure all patients were placed into an abduction sling in neutral rotation. No surgical complications were encountered with any patient.

Results
At an average follow-up of 32 months, 10 of 12 (83%) of patients were able to return to play at the same or
higher level of competition. Two patients did not return to sports at all after surgery. Of these two patients
one completed successful rehabilitation and was cleared for play by the operating surgeon and her physical
therapist, but chose not to return to any sport. Further discussion with her mother at the time of data
collection revealed that the family agreed that she was physically ready to return to sport, but a decision was
made to not return in an effort to avoid any potential future injury. The other athlete who did not return
subsequently underwent a second surgery to remove scar tissue and frayed labral tissue at the site of the
repair. The repair was otherwise well healed; there was not found to be any suture impingement, and the
rotator cuff was intact. Despite an improvement in her pain after the second surgery, she was unable to
achieve a level of performance for return to volleyball.
Of the ten athletes who returned to sports at the same or higher level of competition 5 (50%) were playing pain-free or without any arm trouble at time of follow-up and 5 (50%) were playing with arm trouble or pain. The average time from surgery to release for play was 4.45 months (range 4-6.5 months). The average postoperative KJOC score for all athletes was 63.93 of 100 (range 25.7 to 90.7) with 25% good to excellent, 16.67% fair, and 58.33% poor. Average KJOC score for athletes who returned to sport was 69.2 of 100 compared to 37.6 of 100 for those who did not return, and this difference was statistically significant (p=.017). The Average ASES score for all athletes was 84.19 out of 100 (range 46.13-100), with 66.67% falling into the good to excellent range, 16.67% fair, and 16.67% in the poor range. The mean ASES for those who returned to play was 87.55 of 100 versus 67.39 of 100 for those who did not and this difference did not reach statistical significance (p=0.260).
Four of twelve athletes underwent debridement of a partial rotator cuff tear (PRCT). The average KJOC for those with a PRCT was 58.4 versus 66.7 for those without PRCT, showing a trend for worsening performance in those with partial tear, but not reaching statistical significance (p=0.25). Mean ASES score for those who underwent PRCT debridement was 83.2, versus 84.7 for those without partial tear, and this did not reach statistical significance (p=0.441). We also found no significant relationship between type of sport, demographics, or number of anchors used, and any differences in KJOC or ASES scores, or the ability to return to play postoperatively.
Discussion
The main finding in the current study was that 83% (10/12) of overhand athletes in our cohort were able to return to the same or higher level of competition in their sport after arthroscopic repair of a type 2 SLAP lesion. We did find a statistically significant difference (p=.017) in KJOC score between those who returned to play (69.2/100) and those who did not (37.6/100). Statistical analysis failed however to correlate type of sport, demographic data, or number of anchors used with any differences in KJOC or ASES scores, or the ability to return to play postoperatively.
We also found that arthroscopic debridement of a partial rotator cuff tear (PRCT) at the time of type 2 SLAP repair showed a trend for worsening performance postoperatively, but did not reach statistical significance in relationship to differences in KJOC (p=.25) or ASES (p=.44) scores, or athlete’s ability to return to overhand sports (p=.52). This is in contrast with Neri et al., [36] who found in a cohort of young professional and collegiate baseball players that partial rotator cuff debridement led to statistically significant lower KJOC scores in PRCT athletes (avg. 66.0) versus non-PRCT athletes (avg. 82.8), and a much lower rate of return to play (12.5%) in PRCT athletes versus non-PRCT (80%) athletes. Morgan et al. [35] also reported that although of 44/44 (100%) baseball pitchers returned to play after SLAP repair, 7/44 (14%) did not return to the same level of play; and this correlated statistically with debridement of a partial thickness undersurface rotator cuff tear in those 7 athletes.
Interestingly, despite the high percentage of athletes returning to play at the same or higher level of competition in our study, the mean KJOC score for those who returned still fell into the poor range (69.2 of 100). These results are not dissimilar however to other studies which have shown a high level of return to play despite lower KJOC scores. Neuman et al. [16] reported an average KJOC score of 73.6 among all overhand athletes in their study with a subjective perception of 84% return to previous level of play. In a cohort comprised primarily of young professional baseball players, Neri et al. [36] found an average KJOC score of 86.4, for those who returned at the same or higher level of play. Chalmers et al. [37] recently published a related study examining postoperative kinematic and electromyographic differences between SLAP repair and biceps tenodesis in elite level throwing athletes. Despite the fact that the study group was comprised of pre-selected athletes who had returned to the same or higher level with no pain, the average KJOC scores were still low at 66/100 and 50/100, respectively, for biceps tenodesis and SLAP repair in this study. This is further supported by Franz et al., [14] who showed that the average KJOC scores for players with a history of shoulder or elbow surgery (75.+/- 15.1) were significantly lower than for players without a history of arm surgery (94.4 +/- 11.1) (P< .0001). Therefore, although the specific etiology is unknown, the KJOC scores in the current study may reflect some degree of pain and/or other continued arm trouble after SLAP repair in these overhand athletes, despite their return to a previous or higher level of competition. We believe this is consistent with the notion that overhand athletes may be more sensitive to subtle changes in their shoulder which affect performance [36], and with prior research validating the ability of the KJOC outcomes measure to better detect these types of subtle changes [14-16,36].
Postoperative alterations in biceps and thoracic rotation kinematics after SLAP repair may be such subtle factors which can negatively impact overhand performance and KJOC scores, despite a return to the same or higher level of competition. Chalmers et al. [37] analyzed 18 pitchers after SLAP repair or biceps tenodesis. Seven athletes were controls, 6 had returned to play at the same or higher level and pain free after SLAP repair, and 5 had returned to play at the same or higher level and pain free after biceps tenodesis. They demonstrated that while both biceps tenodesis and SLAP repair can restore physiologic neuromuscular control, the biceps tenodesis appeared to more closely restore the normal pattern of muscular activation within the long head of the biceps muscle than did the SLAP repair; and further the SLAP repair athletes may exhibit altered patterns of thoracic rotation during a pitching motion compared to controls, and to biceps tenodesis patients. To date, however, the role of biceps-based procedures to treat type 2 SLAP tears in young, competitive, overhand athletes has not been fully demonstrated.
There is a lack of uniformity in the literature as to defining success and return to play after SLAP repair [25,36,38,39]. In the current study group we demonstrated an 83% return to the same or higher level based upon the level (high school, club, collegiate) of competition to which the athlete returned. In contrast Neri et al. [36] defined return to “pre-injury” level of play as only those who returned to overhand sport pain-free at the time of evaluation. They reported on 23 overhand athletes with an average age of 25 (range 18-45) after SLAP repair, and they further organized athlete data into three groups with category 1 being painfree return to play, category 2 being return to play with pain, and category 3 no return to play. In their study 13/23 (57%) returned pain-free and 6/23 (26%) returned with pain, for an overall return to play rate of 83%, which is consistent with our findings. Similarly, if we combine the Grade 0 (no limitation), Grade I (mild limitation), and Grade II (moderate limitation) results of Kim et al. [25] this also shows a combined return to play, with or without some level of arm trouble or pain, of 83%. Additionally, Yoneda et al. [39] defined success as either an excellent result (return to play without pain), or a good result (return to play with occasional or mild pain) in 80% of 10 overhand athletes (baseball, volleyball, and badminton) with an average age of 17.8, after arthroscopic metal staple repair of a SLAP lesion. More recently, Fedoriw et al. [38] reported on return to play with an even more detailed and novel definition which they termed “return to prior performance” (RPP) in 37 professional baseball players (27 pitchers, 10 position players) with average age of 23.7 (range17-42) after type 2 SLAP repair. RPP was defined by the ability to return to the same or higher league level, duration of at least 1 season at that level, and a statistical performance (example: games started, innings pitched, ERA, plate appearances, batting average, slugging percentage, etc.) which was similar to their averages prior to injury. Return to play (RTP) in this study was defined as a return to spring training and at least 1 game thereafter regardless of level of play (same, higher, or lower professional baseball league level). Their results were overall less favorable for baseball pitchers with RTP and RPP of 48% and 7% respectively; compared to position players with RTP and RPP of 85% and 54% respectively. Therefore the results of our study (83% return) appear to be most similar to the RTP outcomes for position players (85%) by Fedoriw et al., [38] and are in agreement with the above studies when looking at level competition to which the athlete returned, with or without some level of arm trouble or pain [25,36,39].
Although we cannot conclude that younger age was a contributing factor for success as it relates to postsurgical performance in the current study, prior research has demonstrated younger age as a positive predictor for good outcomes and older age negatively impacting outcomes after type 2 SLAP repair. Provencher et al. [40] found a 36% failure rate in a military population with an average age of failed procedures of 39 years versus 29 years for those deemed successful. In 2002 O’Brien et al. [41] found that less than half (44%) of athletes treated with type 2 SLAP repair returned to their preinjury level of competition. His subjects had an average age of 39 years. In 2006 Cohen et al. [24] studied a similar population with average age of 34 and showed a parallel return to sport rate of 48%. Cohen et al. [5] in 2011 reviewed young elite overhand athletes after SLAP repair and compared those who returned at the same or higher level (average age 23.4) with those who returned at a lower level or not at all (average age 25.4). Statistical analysis revealed that younger age at the time of surgery was significant (p=0.023) for return to play at the same or higher level; however the age differences in this study were very minor and the clinical significance of this is not known.
Current literature demonstrates that successful outcomes can be achieved after arthroscopic repair of type 2 SLAP lesions in both old and young patients, athletes and non-athletes, and in overhand and non-overhand groups [5,17-23,35,42]. However, the older average age range seen in many studies may not reflect the higher demands placed on the shoulder by younger athletes competing at various elite levels (high school, club, college, or professional) [36]. Outcomes after type 2 SLAP repair in this sub-class of young elite-level overhand athletes vary widely and have included relatively few female athletes [5,25-28]. Given that the majority of the published data after SLAP repair for this sub-class of young elite overhand athletes has focused on male baseball players [5,25,36], we sought to determine a return to play rate and level of play in a cohort of young, elite, female, overhand athletes who are also keenly focused on ability to return to play after surgical treatment. The average age (16.25 yrs.) at time of surgery in the current study is reflective of the increased participation rates and intensity levels emerging at the high school and club levels, and our need to better outline treatment recommendations for these young women who have sustained shoulder injury and SLAP tear.
Limitations
There are several limitations to this study. The current study group of 12 patients is relatively small and may
not have allowed detection of differences across variables such as type of sport, number of anchors used, and
the existence of a partial rotator cuff tear. Our sample size is not dissimilar however to other studies which
include young elite athletes after SLAP repair, when the overhand sub-groups are separately analyzed. Neri
et al. [36] examined 23 elite college and early professional overhand athletes after SLAP repair; Kim et al.
[25] reviewed 34 patients after type 2 SLAP repair, of which only 18 were overhand athletes; Friel et al. [23]
reported on a total of 48 patients after type 2 SLAP repair, of which only 11 were overhand athletes; Yung et
al. [28] reported on 16 patients of which 5 were elite level overhand athletes; and Yoneda et al. [39] reported
on 10 overhand athletes after arthroscopic SLAP repair. Secondly, the retrospective nature of the study
has the potential to introduce recall bias, although only two of ten returners in our study had retired from
sport at the time of data collection. These athletes were asked to recall their highest level of postoperative
play at the time of data collection. One retired for non-shoulder related reasons after completing 3 years
of postoperative play, ending after her freshman college season. The other athlete played for two years of
junior college, then stopped sports to focus on academics for her final two years. The remaining returning
athletes (8/10) were active in their sport at time of data collection. Finally, this study does not include
preoperative ASES or KJOC scores for comparison, or a control group of young, elite, female overhand
athletes treated non-surgically for a type 2 SLAP tear. However historical control data suggests that the
potential for return to overhand sport without surgery and after failed conservative care is around 63% [11].
Certainly, a prospective analysis with larger sample size and a control group would be ideal.
Strengths of this study include that all operations were performed with a standardized arthroscopic technique by a single surgeon experienced in shoulder arthroscopy and the care of overhand athletes. All patients underwent a standardized rehabilitation protocol postoperatively, and our study criteria allowed a focus on level of return to play in narrowly defined group of young, elite, female, overhand athletes. In contrast to prior reports that vary in terms of age, outcomes measures used, and level of athletic participation (recreational versus competitive, overhand versus non-overhand) [10,17-23,35,42], the current study is narrowly focused on a group of young, elite, competitive overhand female athletes. Additionally, we utilized a more stringent outcomes measure (KJOC score) [13,16] that has been shown to be more accurate in analyzing return to play and level of performance in overhand athletes [16,36], especially as compared to the ASES which is more focused on return to activities of daily living.
Conclusion
There is a paucity of data in the literature reporting return to play outcomes after arthroscopic type 2 SLAP
repair in young, elite, female overhand athletes. In the current study we demonstrated an 83% return to same
or higher level of play after arthroscopic repair of type 2 SLAP lesions in this group, and this treatment is a
viable option in the setting of failed conservative care and the desire to continue overhand sports.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!