Biography
Interests
Iffat Ahmed & Ravi Paul*
Department of Psychiatry, University Teaching Hospital, Zambia
*Correspondence to: Dr. Ravi Paul, Department of Psychiatry, University Teaching Hospital, Zambia.
Copyright © 2019 Dr. Ravi Paul, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Suicidal thoughts, or suicidal ideation, means thinking about or planning suicide [1]. Medical
doctors are one of the high risk groups for suicide [2,3]. According to a study done by Schernhammer
and Colditz (2004), the suicide rate among male physicians is more than 40% higher than males
in the general population, and that of female physicians is 130% higher than females in the general
population. This problem seems to arise during medical school [4,5]. A study done by Ricardo
and Carlos (2018) revealed that the prevalence of suicidal ideation ranged from 1.8% to 53.6%
in medical students from 17 different countries. They also found that depression and depressive
symptoms, a previous diagnosis of a psychiatric disorder, lower socioeconomic status/financial
difficulties, having a history of drug use, and feeling neglected by parents were the most common
factors associated with suicide ideation in these students.
Little is known about the prevalence of Suicide Ideation and its associated factors in the Zambian medical setting and this study was done to find the prevalence and associated factors of suicide ideation in medical students at Ridgeway Campus.
A three part self-administered questionnaire that contained a sociodemographic questionnaire,
SRSS and BDI was distributed amongst medical students at Ridgeway Campus to collect data for
a sample size of 283 participants. Data was analyzed using STATA Version 14.2.
The overall prevalence of suicide ideation was found to be 6.71% and there was an association with
depression, gender, marital status, year of study and whether the student sought counselling services
or not. Depression and whether the student accessed counselling services or not had the lowest
P values of 0.000. Out of the 19 at high risk for suicide, 2 were found to be severely depressed, 4
had moderate depression, 2 had borderline clinical depression, 9 had mild mood disturbance and
2 had ups and downs that were considered normal. 10 out of the 19 accessed counselling services
while the remaining 9 did not. The female gender had a higher prevalence of suicide ideation than
the male population (14 females’ vs 5 males). Out of the 19 at high risk, 11 were single, 6 were in
relationships, 1 was married and the remaining was divorced. Of note, prevalence was found to be
highest in the 4th year students than the rest of the students (9 out of the 19) No association was
found between suicide ideation, and age, type of sponsorship and Substance Abuse.
It can be concluded that there is a significant prevalence of suicide ideation in medical students
at Ridgeway Campus. 6.71% were found to be at high risk of suicide ideation. It can also be
concluded that female gender, single marital status, being in 4th year of study and scoring high on
BDI were higher risk factors for suicide ideation. It is also worthy to note that no association was
found between suicide ideation and substance abuse. This could mean that students use substances
to cope with stressors, however more research needs to be done on this factor. There is need for early
detection of suicide ideation to prevent deaths by suicide.
Introduction
Suicidal thoughts, or suicidal ideation, means thinking about or planning suicide [1]. There are two kinds
of suicide ideation; Passive and Active. Passive suicide ideation is when a person wishes they were dead or
that they could die, but do not actually have a plan to kill themselves [6]. They usually wish to die in their
sleep or be killed in an accident. They exhibit behaviors of not looking after themselves, like not eating or
drinking, or not taking medicines vital for their health [7]. Active suicide ideation on the other hand, is
when in addition to thinking about suicide, the person also has a plan on how to do it and intends to carry
out the plan [6]. Suicide ideation does not include the final act of suicide, which is the act of deliberately
killing oneself.
According to the World Health Organization (WHO), every year close to 800 000 people die due to suicide which can be translated to one person committing suicide every 40 seconds. There are indications that for each person that commits suicide, there may be more than 20 others who attempted suicide [8]. Suicide occurs throughout the lifespan, and in 2016 it was the second leading cause of death among 15-29-yearolds globally according to WHO [9]. The suicide mortality rate for Zambia in 2016 was 6.1 (per 100000 population) [10].
Medical doctors are one of the high risk groups for suicide [2,3]. According to a study done by Schernhammer and Colditz (2004), the suicide rate among male physicians is more than 40% higher than males in the general population, and that of female physicians is 130% higher than females in the general population. This problem seems to arise during medical school [4,5]. In their first year of studies, medical students have similar rates of psychological morbidity to the age-matched general population, but as they progress through their medical studies they experience a worsening of their mental health [11]. Suicidal ideation rates vary greatly in medical students, ranging from 6.0% to 43.0% [11].
Many factors contribute to the high rates of suicidal ideation in medical students. Due to the psychiatric stressors these students are susceptible to, they have alarming rates of burnout, anxiety, and depression [12]. Studies have shown that many students are depressed when they commit suicide [12]. Information overload, lack of leisure time, financial debt, being away from home, academic load, and work pressure also make medical students vulnerable to suicide ideation. Feeling neglected by parents was also associated with suicide ideation [11].
Other factors that may contribute to suicidal thoughts in medical students include; substance abuse, heavy curricular burdens, decreased life satisfaction, and certain personality traits including maladaptive behavior. Also, personality traits like neuroticism, introversion, and low self-esteem make medical students more vulnerable to mental health stressors and suicidal ideation [12].
Studies have shown that suicidal ideation has been associated with low social function scores. This indicates a decrease in the pursuit of social activities with family, friends, or colleagues because of physical or emotional constraints. Although not performed on medical students, one study concluded that social functioning may have a major impact on suicidal ideation [12]. Ricardo and Carlos (2018) are of the view that also contact with suffering, confronting with death, and caring for vulnerable persons could be factors that trigger emotional problems in medical students.
Concerns about time, confidentiality, stigma, and the potential negative effects on their careers make medical students reluctant to seek psychiatric help. Identifying the prevalence and factors associated with suicidal ideation in medical students would help early detection of this problem and appropriate interventions can also be provided earlier. Moreover, intervening at an early stage of medical training helps prevent mental health problems later. It also reduces the risk of suicide once students become practicing physicians [11].
Integrated medical curricula aimed at improving the well-being of medical students have gained popularity in some countries in recent years. These initiatives focus on students’ mental health, improving antiquated curricular structures, and offering systemic support. One example is the Vanderbilt Medical Student Wellness Program, which had its origins in the Vanderbilt Wellness Program established in 2005. This program has received positive feedback and responses from students [12].
The researcher did not come across any published data to show the prevalence of suicide ideation in medical students of Zambia. However, Kelsie Alexandra (2018), a Clinical Psychology doctoral student in San Diego California wrote on her GoFundMe page that, “During our last visit to Zambia in 2017, we saw a need for a counselling center on the medical school campus. Suicide rates among medical students are high because they feel incompetent as physicians. This stems from inadequate training and limited resources. Many of these students have found their identities as future doctors, so these feelings of failure challenge their core selves and lacking proper coping skills, they become hopeless and take their lives.”
She also wrote, “Last year, three students were sharing how the professors throw the cadavers down in front of them and tell them to start practicing surgical techniques. “We feel scared that we are working with real bodies, but we can’t process this because they will say we’re weak.” Others shared how they are barely getting four hours of sleep a night because of the extensive material they need to study.”
All this shows that there is need for further investigation on the prevalence of suicide ideation in medical students in Zambia and the factors that may contribute to it.
According to WHO about 1 million people die from suicide every year, and in the past 45 years, the rate of
suicide has increased by 60% worldwide. The suicide mortality rate for Zambia in 2016 was 6.1 (per 100000
population) [6].
Physicians are considered a high risk group for suicide as demonstrated by a study done by Schernhammer and Colditz (2004). They found that the suicide rate among male physicians is more than 40% higher than males in the general population, and that of female physicians is 130% higher than females in the general population [9]. This problem seems to arise during medical school [9,10]. A study done by Ricardo and Carlos (2018) revealed that the prevalence of suicidal ideation ranged from 1.8% to 53.6% in medical students from 17 different countries. They also found that depression and depressive symptoms, a previous diagnosis of a psychiatric disorder, lower socioeconomic status/financial difficulties, having a history of drug use, and feeling neglected by parents were the most common factors associated with suicide ideation in these students.
In the past few years, there has been an increase in the reported cases of suicide and suicidal attempts among medical students in Lusaka, Zambia. In 2015, a 6th year medical student from the University of Zambia, School of Medicine committed suicide by jumping off a bridge into the Kafue River. Another case of a postgraduate medical student overdosing on anesthetic drugs was reported in 2018. Many other cases of failed suicidal attempts have also been reported. It is worthy to note that such cases only come to attention via the media when individuals have already committed suicide or attempted to, hence implying that such cases are not picked at an earlier stage where interventions could have been made. This could be due to lack of awareness by individuals of mental health services offered and also lack of research in this area. Therefore, the researcher sought to investigate the prevalence of suicidal ideation in medical students at Ridgeway Campus and some of the factors that may be associated with it.
Suicidal ideation ranged from 1.8% to 53.6% in medical students in 17 different countries. However no
research has been done in Zambia. These high numbers suggest the need to firstly investigate whether this
problem exists in Zambia and the risk factors associated with it. This would help identify the mental health
wellbeing of medical students to medical educators, health professionals and policy makers and make them
aware of the importance of mental health. Secondly, it will also help implementation of preventive programs
to combat the various risk factors, as intervening at an early stage of medical training helps prevent mental
health problems later, and reduces the risk of suicide once students become practicing physicians [11].
Lastly, this study would benefit students themselves by making them more open to talk about suicide and
reduce on the stigma associated with it. Additionally, they would be informed and made aware of the help
that is available and the importance of seeking help in due course.
What is the prevalence of suicide ideation in the medical students of University of Zambia, School of
Medicine, and what are the common factors contributing towards such ideation?
To find the prevalence of suicide ideation in Medical students at the University of Zambia, School of
Medicine and associated factors.
To assess suicide ideation in Medical students at Ridgeway Campus.
To identify factors contributing to suicide ideation in Medical students at Ridgeway Campus.
To find out if there are preventive programs for suicide in place at Ridgeway Campus.
To investigate if Medical students at Ridgeway Campus do access help for suicide ideation.
Literature Review
About 1 million people die from suicide every year, and in the past 45 years, the rate of suicide has increased
by 60% worldwide [13]. In 2016, WHO reported the suicide mortality rate of Zambia to be at 6.1 (per
100000 population)
Research has proven that suicide rates among doctors are higher than those in the general population [14]. It was found that among male physicians the suicide rate is more than 40% higher than among men in the general population, whereas that of female physicians is 130% higher than among women in the general population [9]. According to an article published on Medscape by Pauline Anderson, the physician suicide rate was found to be 28 to 40 per 100,000, more than double that in the general population [15].
Beth Brodsky, PhD, associate clinical professor of medical psychology in psychiatry at Columbia University and the Irving Medical Center, New York City is of the opinion that the high physician suicide rate is not surprising, given the stressors physicians face. She also says that the stress starts in medical school and continues in residency because of the high demands, competitiveness, long hours, and lack of sleep [15]. Schernhammer (2005) is also of the opinion that the increased risk for suicide among physicians may begin during medical school.
The suicide rate among medical students is higher than in the age-matched general population. Some studies have shown that 3% to 15% of medical students have suicidal ideation during medical school training [9]. Studies have shown that suicidal ideation is a strong predictor of attempted suicide [11]. The National Comorbidity Survey found that of individuals in the general population that have suicidal ideation, 34% of them develop a suicide plan, and of those who plan, more than 70% will attempt suicide. Of note, 26% of individuals with suicidal ideation progressed directly to an unplanned suicide attempt [9].
Ricardo and Carlos (2018) did a systematic review of literature of articles published on the prevalence of suicidal ideation and associated factors in medical students between July 2011 and May 2018, and found that the prevalence of suicidal ideation ranged from 1.8% to 53.6%. This review included 17 studies comprising an overall total of 13,244 medical students recruited in 13 different Western and Non Western countries. They also found that the prevalence of suicidal ideation did not seem to vary between countries from different continents, thus it can be said that suicidal ideation is independent of geographical location [11].
Previous studies done in the Unites States between 2006 and 2007, found that approximately 1 of 9 students have thoughts of suicide, and the rate of suicidal ideation among medical students was 11.2%. This is higher than for individuals of similar age in the general U.S. population. (6.9% among 25- to 34-year-olds) [9] In an article published on Medscape by Deborah Brauser, it is said that in six studies that compared medical students to an age-matched population sample, three found the suicide rates to be higher in the students, two showed that they were lower, and one found the rates to be comparable [16]. A study done in South Africa also found a higher suicide rate among medical students than in the general age- appropriate population. They found a prevalence of suicidal ideation (32.3%) and suicidal attempt (6.9%), which is three times higher than the general age-appropriate population [17].
Research has shown that female medical students have significantly higher rates of suicidal ideation than
the general population [12]. Goyal et al (2012), are of the opinion that females studying in a medical college
are subjected to more stress than males because of issues like security and the societal pressure on them to
be at par with their male counter-parts. Research done in India found that in females, suicide ideation was
62.2% while in males it was 45.6%. This difference was found to be statistically significant [18]. However,
according to a study done in Pakistan females were found to have a prevalence rate of 32%, and males a
rate of 17% and this difference was not statistically significant [19]. Studies in Portugal on the other hand showed higher rate of suicidal behavior in male students than in female students. (4.6% compared to 3.6%
in females) [20] In Egypt, studies showed a slightly higher prevalence of suicidal ideation in females [21].
Ricardo and Carlos’s (2018) review found inconsistent results regarding the association between suicidal
ideation and gender. Some studies found no statistically significant difference between genders, while others
found that females are more prone to suicidal ideation [11].
Varying academic stress and examination pressure in different stages of training, could be associated with
different prevalence rates of suicide ideation in the different years of study. In India, research showed that
first year medical students showed the highest suicide ideation rates (64.4%). This could be due to the fact
that in addition to academic pressures, first year medical students face challenges in acclimatizing to the
new life and curriculum of medical school. In the same research the prevalence for second, third and fourth
year students was 56.7%, 40.4% and 44.4% respectively [18]. In Egypt also, the suicide ideation rate was
found to be highest in year 1 students compared to pre-clinical and clinical phase students [21]. On the
other hand studies done in Taiwan, China showed higher suicide ideation rates in second year compared to
first year [11].
Depression is frequently documented as one of the risk factors most likely to lead to suicidal thinking [12].
A study done in Portugal found that suicidal behavior was 66.7% in those with severe depression, 36.4% in
moderate depression, 28.6% in mild depression and 1.9% in those with no or minimal depression [20]. This
study clearly shows the strong association between depression and suicidal ideation. Researchers in Brazil
also found that moderate to severe depressive symptoms were linked with suicide ideation [22].
A study done by Breet, Goldstone and Bantjes, demonstrated a positive association between substance
use and Suicidal Ideation across all substances (i.e. alcohol, tobacco, cannabis, illicit drugs, non-medical
use of prescription drugs). They searched five databases using a combination of keywords for substance
use, Suicidal ideation and behavior, and Low- and middle-income countries to identify English-written
quantitative studies published between January 2006 and February 2016. Only 22% of the study came from
lower-middle-income and low-income countries [23]. However this study was not done specifically in
medical students.
Other factors that are associated with suicidal ideation include Burnout among others. A study done in
the United States found that the association between burnout and suicide ideation was large. (2- to 3-fold
increased risk) [9] Substance abuse such as alcohol abuse is another factor associated with suicide ideation.
Researchers in Portugal found that students who had a problem of alcoholism were at a higher risk of
suicidal behavior (8.5%) than those students that had no apparent alcohol problem [20]. Living alone was
also found to be associated with higher suicide ideation by researchers in Brazil and Portugal [20,22].
Suicidal ideation among medical students has been vastly discussed by researchers, however a similar
interest among medical educators has not been provoked. Maybe if researchers place a greater emphasis
on the specific risk factors associated with suicidal ideation, this would create more enthusiasm in medical
educators to implement prevention programs, like stress coping strategies into the medical curriculum [12].
Methodology
A quantitative cross sectional study was done. Self-administered questionnaires were used to get social
demographic characteristics of participants and suicidal ideation was assessed using the Suicidal Risk
Screening Scale and Becks Depression Inventory.
The study was conducted at The University of Zambia, Ridgeway Campus, Lusaka, Zambia.
The target population was medical students aged 18 and above in 3rd to 7th year enrolled in The School of
Medicine at Ridgeway Campus.
• Students aged 18 years and above
• Ability to give consent
The sample size calculated was 384 participants. The following formula was used to calculate the sample size:
where: n= sample size
z = standard deviation set at 1.96 (95% confidence level)
d = margin of error (usually 0.05)
p = prevalence rate in study area
For this study the prevalence of suicide ideation in Zambia is not known therefore 50% was used as the “p” value. Therefore,
n= [1.96²x50/100(1-50/100)]/ 0.05² = 384
Random sampling was done. The researcher randomly distribute about 60 questionnaires in each class (3rd
year to 7th year medical students). Participants that were available at the time and gave consent were included
in the study.
Data was collected by the researcher and research assistants.
Data was entered into questionnaires by the participants and then transferred onto an Excel spreadsheet by
the researcher. The data was then imported to STATA version 14 for further analysis.
Statistics were used to obtain means and standard deviation for the independent and dependent variables. These were used to determine the amount of variability and association between the dependent variables in relation to prevalence of sensitivity to suicidal ideation.
A correlation analysis was used to determine the associations between independent variables and the dependent variable. The independent variables were age, gender, year of study, marital status, sponsorship, substance abuse, depression and whether the client sought any professional help. While the dependent variable is prevalence of suicidal ideation.
Approval was sought from the University of Zambia Biomedical and Research Ethics Committee. Permission
was also sought from the University of Zambia, School of Medicine administration for research to be
conducted on their students. Informed consent was obtained from all participants that volunteered to take
part in the study and the objectives of the study were clearly explained to them. Participants were assured
of confidentiality on the information given, the names and codes would be used for follow up purposes
only which were kept separate from the data to be analyzed. Participants were free to withdraw from the
research if they wish to do so without any consequences. All information was kept safe under lock and key.
The participants signed the consent form as proof of agreement to participate in the research study. Those
participants that score high on the BDI and SRSS will be followed up and linked to Clinic 6 (Psychiatry)
at the University Teaching Hospital.
Presentation of Findings
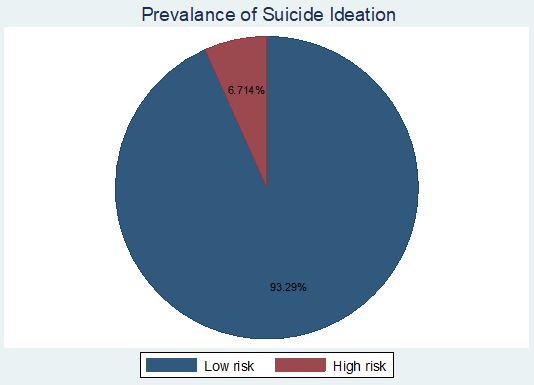
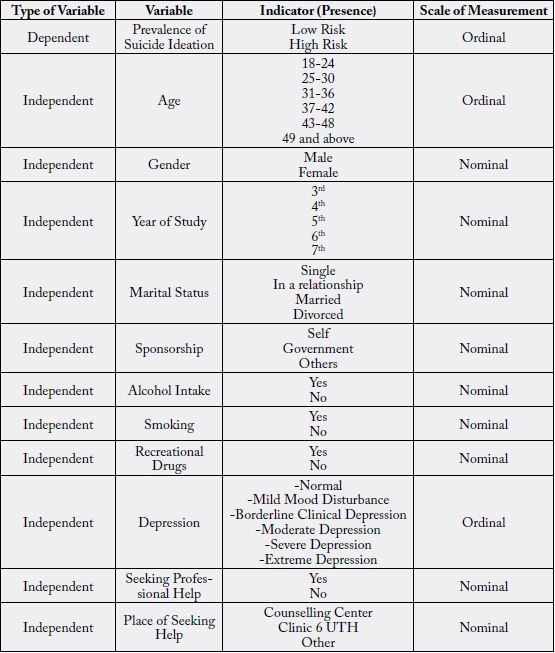
Figure 1 shows results for the prevalence of suicidal ideation. Results show that (n=264, 93.29%) of the respondents fell into the category of lower risk suicidal ideation category while (n=19, 6.71%) fell into the higher risk suicidal ideation category.
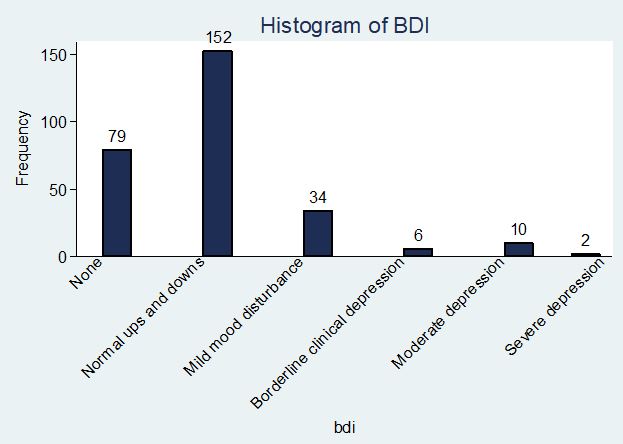
Figure 2 shows that (n=79, 27.92%) of respondents fell into the category of no depression, (n=152, 53.71%) fell in the category of ups and downs that are considered normal, (n=34, 12.01%) fell in the category of mild mood disturbance, (n=6, 2.12%) respondents that fell into the category of borderline clinical depression, (n=10, 3.53%) fell into moderate depression, (n=2, 0.71%) were severely depressed and no one was found to have extreme depression
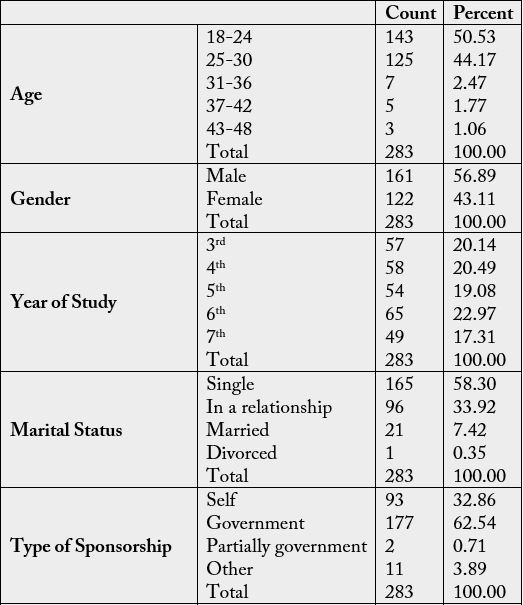
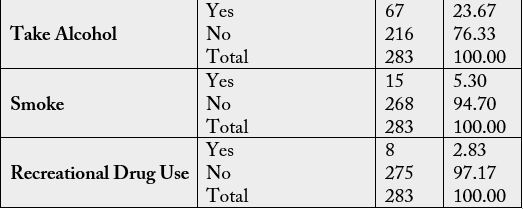
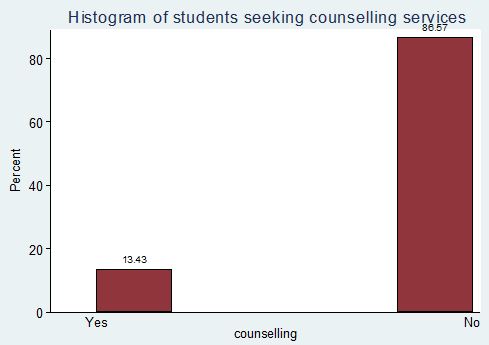
Figure 3 shows results for the percentage of students that seek counselling services. Results show that (n=38, 13.83%) have sought counselling services while (n=245, 86.57%) have never sought counselling services.
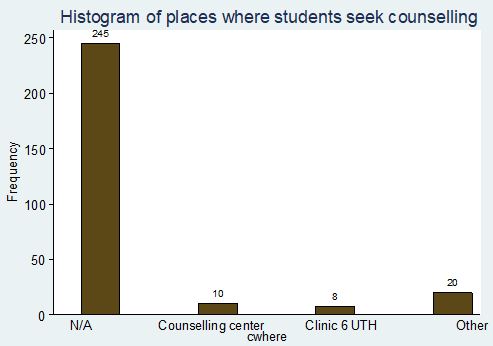
Figure 4 shows results for the places where students sought counselling services from. Results show that (n=10, 3.53%) went to the counselling center, (n=8, 2.83%) went to Clinic 6 at UTH, while, (n=20, 7.07%) went to other places.
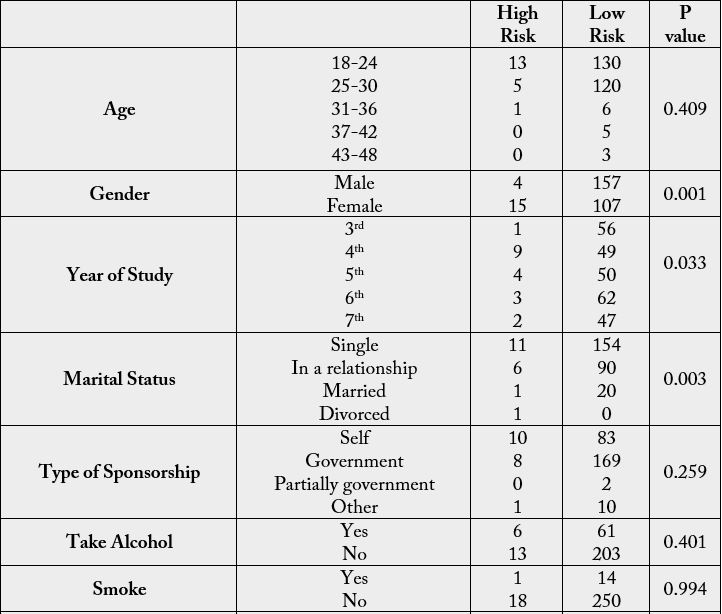
According to the Pearson Chi square test which is calculated under the assumption of no association, a p value < 0.05 means that an association exists between the two variables, where as a p value >0.05 means that no association exists between the two variables.
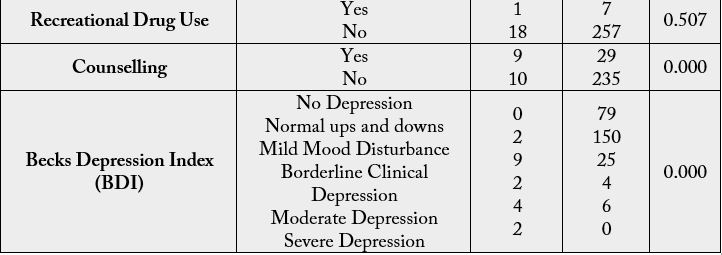
Therefore according to the above table the factors that are associated with suicide ideation include; Gender, Year of study, Marital Status, BDI and whether the student had sought counselling services or not. However, Age, Type of Sponsorship, Alcohol Intake, Smoking and Recreational Drug use do not have an association with Suicide Ideation
Discussion of Findings
The findings from the Suicidal Risk Screening Scale (SRSS) showed that 6.71% were at high risk for suicide
ideation whereas 93.29% were in the lower risk category. This finding was in accordance with previous
studies done which showed a prevalence of suicide ideation in medical students to be between 3% and 15%
[9]. This study was also in line with the systematic review of literature of articles done by Ricardo and Carlos
(2018), on the prevalence of suicidal ideation and associated factors in medical students between July 2011
and May 2018, which found a prevalence of 1.8% to 53.6%. This review included 13 countries (Western and
Non Western) and found no association between suicidal ideation and geographical location. A study done in South Africa also found a higher suicide rate among medical students than in the general age- appropriate
population. They found a prevalence of suicidal ideation (32.3%) and suicidal attempt (6.9%) [17].
The National Comorbidity Survey found that of individuals in the general population that have suicidal ideation, 34% of them develop a suicide plan, and of those who plan, more than 70% will attempt suicide. Of note, 26% of individuals with suicidal ideation progressed directly to an unplanned suicide attempt [9]. Therefore even though 6.71% seems like a small portion of people with suicide ideation, it really is not as it relates to 19 out of 283 people studied. As suicide is a matter of life and death, even 1 person with suicide ideation is considered significant. This is in accordance to the World Health Organizations indication that for each person that commits suicide, there may be more than 20 others who attempted suicide [4].
In the study conducted it was found that out of the 283 students studied, 2 (0.71%) were found to be
severely depressed, 10 (3.53%) were moderately depressed, 6 (2.12%) had borderline clinical depression, 34
(12.01%) had mild mood disturbance, 152 (53.71%) had ups and downs of life which are considered normal
and, 79 (27.92%) were found to have no depression. There was no one found with extreme depression. The
study also showed a strong correlation between suicide ideation and depression with a P value of 0.000. Of
the 19 students that were found to be at high risk of suicide, the majority (9) were found to have mild mood
disturbance, 4 were moderately depressed, 2 were Severely Depressed another 2 had borderline clinical
depression and the last 2 had ups and downs which were considered normal. It is also worthy to note that
those that had no depression were at low risk of suicide ideation and, none that had severe depression were
at low risk of suicide ideation. These results are in accordance with a study done in Portugal which found
that suicidal behavior was 66.7% in those with severe depression, 36.4% in moderate depression, 28.6% in
mild depression and 1.9% in those with no or minimal depression [20]. Researchers in Brazil also found
that moderate to severe depressive symptoms were linked with suicide ideation [22]. Therefore it could be
concluded that the higher the level of depression, the higher the risk for suicide ideation.
56.89% (161) of the students were Male while, 43.11% (122) were Female. The results showed that there is
an association between gender and suicide ideation, based on the Pearson chi square which gave a P value
of 0.001. It was seen that females (15 out of the 19) were at higher risk of suicide ideation than males (4
out of 19). These results were generated despite the Male population being slightly higher than the female
population and therefore it can be said that being female is a risk associated with suicide ideation. This
is in line with research done in India which found that in females, suicide ideation was 62.2% while in
males it was 45.6% [18]. Females could be at higher risk for suicide ideation because of their higher risk of
depression compared to males as found in literature. Other factors that could predispose females to higher
risk of suicide ideation is that females in the African and Asian cultures have more family responsibilities
than Males. This could play a role in affecting their performance at school and hence leading to suicide
ideation. Goyal et al (2012), are of the opinion that females studying in a medical college are subjected to
more stress than males because of issues like security and the societal pressure on them to be at par with their
male counter-parts. Studies in Egypt also found higher rates of suicide ideation in females than males [21]. This study however was not in line with the studies done in Pakistan and Portugal, which showed a higher
prevalence of suicide ideation in Males than in Females [19,20]. It was also not in line with the study done
by Ricardo and Carlos which found no statistically significant difference between genders, while others
found that females are more prone to suicidal ideation [11].
In this study, 57, 58, 54, 65 and 49 students were from the years 3rd, 4th, 5th, 6th and 7th respectively. A P
value of 0.033 was found between suicide ideation and year of study and hence it can be said that the two
variables are associated. Out of the 19 that were at high risk for suicide ideation, 9 were in 4th year, 4 in 5th
year, 3 in 6th year, 2 in 7th year and 1 in 3rd year. With these results no formal conclusion can be drawn as to
whether suicide ideation is higher in the lower years or in the higher years. This could be due to the fact that
not equal number of students were selected from each year. However the researcher is of the opinion that
4th year at Ridgeway Campus is the bulkiest year and this could be a contributing factor to the high suicide
ideation rate in the 4th years. In India, research showed that first year medical students showed the highest
suicide ideation rates (64.4%). The researchers are of the opinion that this could be due to the fact that in
addition to academic pressures, first year medical students face challenges in acclimatizing to the new life
and curriculum of medical school [18]. In Egypt also, the suicide ideation rate was found to be highest in
year 1 students compared to pre-clinical and clinical phase students [21]. On the other hand studies done in
Taiwan, China showed higher suicide ideation rates in second year compared to first year [11].
According to the data gathered there was found to be an association between Marital Status and Suicide
Ideation. Out of the 283 participants, 165 were single, 96 were in a relationship, 21 were married and 1 was
divorced. From the 19 that scored high on the suicide risk scale, it was seen that 11 were single, 6 were in
a relationship, 1 was married and another 1 was divorced. From this it is seen that being single could be a
risk factor for suicide ideation. This is in line with research done by Russell et al which showed that suicidal
ideation has been associated with low social function scores which indicates a decrease in the pursuit of
social activities with family, friends, or colleagues [12]. The researcher is of the opinion that relationship
problems and divorce could also lead to suicide ideation.
The results obtained found that 13.43% sought counselling services while 86.57% did not seek any form
of counselling services. The Pearson chi squared also gave a P value of 0.000 which indicates a strong
correlation between suicide ideation and whether the person sought any counselling services or not. Out
of the 19 at high risk, 10 sought counselling services while 9 did not. According to Ricardo and Carlos,
concerns about time, confidentiality, stigma, and the potential negative effects on their careers make medical
students reluctant to seek psychiatric help [11]. However in this research it was shown that people have
become more aware of the need to seek professional help and could be a stepping stone in battling the
stigma associated with suicide ideation and Mental Health in general.
It is also worthy to note that out of the 38 students that sought counselling services, 8 had been to clinic 6 Psychiatry at UTH.
From the results obtained there was no association found between sponsorship and suicide ideation. However
it is worthy to note that out of the 19 who were at high risk of suicide ideation, 10 were self-sponsored.
Therefore the researcher is of the opinion that financial constraints could be a risk factor for suicide ideation.
This is in agreement of Ricardo and Carlos citation that, information overload, lack of leisure time, financial
debt, being away from home, academic load, and work pressure also make medical students vulnerable to
suicide ideation [11].
Out of the 283 participants, 67 were found to take alcohol, 15 smoked and 8 used recreational drugs.
However there was no association found between suicide ideation and substance abuse. This could be true
in that substances may help individuals cope with stress, and hence reduce the risk for suicide ideation,
however other research has found that substance abuse could actually lead to suicide ideation. Russell et al
cited that substance abuse leads to an increase in suicide ideation [12]. A study done by Breet, Goldstone
and Bantjes, also demonstrated a positive association between substance use and Suicidal Ideation across all
substances (i.e. alcohol, tobacco, cannabis, illicit drugs, non-medical use of prescription drugs) [23]. In this
research however, out of the 19 that were high risk for suicide ideation, 6 took alcohol while 13 did not, 1
smoked while 18 did not and also 1 used recreational drugs while 18 did not.
The main limitations faced by the researcher were lack of adequate time and funding to print enough
questionnaires. Out of the target population of 384, 283 was reached. Other factors that contributed to this
were that some questionnaires were not given back by participants while other did not want to partake in
this survey.
Another limitation was that by the time ethical approval was given some classes like the 5th years and 7th years were on study break and hence was difficult to target them. This could be one of the reasons that no proper conclusion could be made between the association of suicide ideation and year of study.
Conclusion and Recommendations
It can be concluded that there is a significant prevalence of suicide ideation in medical students at Ridgeway
Campus. 6.71% were found to be at high risk of suicide ideation. This opens areas for further research to find
out the prevalence of actual suicide attempts or even deaths by suicide, as according to literature the higher
the rate of suicide ideation, the higher the chances of suicidal attempts. It can also be concluded that some
of the factors that are associated with suicide ideation are depression, gender, year of study, marital status and whether the person had been for any counselling services or not. Age, type of sponsorship and substance
abuse did not show any association with suicide ideation. There is need for early detection of suicide ideation
to prevent deaths by suicide.
• Further research should be conducted and a wider range of population of medical students should be
targeted. For example students from Apex Medical University, Cavendish University among others should
be included to get a better idea of some of the factors associated with suicide ideation.
• More awareness needs to be raised to battle the stigma of suicide as many people are still unwilling to talk
about and hence were not willing to answer the questionnaires.
• Psychiatrists could organize a day to talk to each class and educate them about suicide and shatter the
myths associated with it.
• Regular screening for suicide ideation in medical students should be conducted.
• A counselling center should be made available to the students at Ridgeway Campus.
• Mandatory yearly screening for suicide ideation could be implemented.
• The school could revise its curriculum to reduce some of the burden.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!