Biography
Interests
Rahanitriniaina, N. M. P.1, Rakotondrainibe, A.1*, Raelison, J. G.2, Rakotondrabe, A.1, Randriamizao, H. M. R.1, Rajaonera, A. T.1 & Rakotoarison, R. C. N.3
1Service de Réanimation Chirurgicale CHU Joseph Ravoahangy Andrianavalona Antananarivo
2Service Accueil Triage Urgence CHU Joseph Raseta Befelatanana Antananarivo
3Service Accueil Triage Urgence CHU Joseph Ravoahangy Andrianavalona Antananarivo, Faculté de Médecine
d’Antananarivo, Université d’Antananarivo - Madagascar
*Correspondence to: Dr. Rakotondrainibe, A., Service de Réanimation Chirurgicale CHU Joseph Ravoahangy Andrianavalona Antananarivo.
Copyright © 2019 Dr. Rahanitriniaina, N.M.P., et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Sepsis in intensive care are burdened with a high morbidity and mortality. The aim of the study
was to determine factors of morbidity and mortality of sepsis at surgical intensive care unit of a
Malagasy university hospital.
A 24-month descriptive and analytical retrospective study (June 2015 - May 2017) was performed
at the surgical intensive care unit of J. R. Andrianavalona University Hospital - Antananarivo.
Patients admitted for any stage of sepsis were included. Demographic, clinical and biological characteristics were studied. The results are expressed in median [Interquartiles 25-75%] and in
frequency. The Spearman correlation test (XLSTAT® 10.0) was used.
458 patients aged 36 [17-50] years, mostly male (sex ratio: 2.06), were included in our study. Sepsis
was present in 73% of patients and septic shock in 37%. The factors correlated with mortality found
were age (p = 0.003), use of vasoactive treatments (p <0.001), high C-reactive-protein (p = 0.02),
elevated serum creatinine (p <0.001) and qSOFA score ≥ 2 (p = 0.01). The qSOFA score had no
correlation with the mortality (42%) but more on the length of stay (4 [2 - 7] days).
The use of the SOFA and qSOFA score is the gold standard in intensive care. In Antananarivo, the
qSOFA score could be integrated into the daily practice especially since it’s related to mortality.
Abbreviations
CHU-JRA : Centre Hospitalier Universitaire Joseph Ravoahangy Andrianavalona
CRP : C-Reactive Protein
GCS : Glasgow Coma Scale
HR : Heart Rate
SpO2 : Oxygen Saturation
q-SOFA : quick Sepsis-related Organ Failure Assessment
RR : Respiratory Rate
SBP : Systolic Blood Pressure
SOFA : Sepsis-related Organ Failure Assessment
Introduction
Sepsis is defined as organ dysfunction due to dysregulation of the systemic inflammatory response of the
host following a bacterial, parasitic or viral suspected or diagnosed infection [1]. It’s a frequent cause of
hospitalization in intensive care unit and is the leading cause of death for patients. Hospital mortality
is higher in Europe (41.1%) than in United States (28.3%) [2]. In Africa, especially in Madagascar, the
correlation between sepsis and hospital mortality is not well defined. The Sepsis-related Organ Failure
Assessment (SOFA) score, which is a predictive score for mortality, cannot be evaluated in current practice
in some hospitals in Antananarivo, especially, because of the unavailability of arterial gasometry. To overcome
this “problem”, the use of q-SOFA (quick SOFA) was proposed [3]. The q-SOFA score is a recent clinical
parameter - less accurate than SOFA, but faster to establish - recommended for assessing patient sepsis [4].
This score includes three parameters: Glasgow coma scale (GCS) less than or equal to 13, systolic blood
pressure (SBP) less than or equal to 100mmHg and respiratory rate (RR) more than or equal to 22cpm (1
point to each item to obtain a q-SOFA score value of 0 to 3). The aim of this work is to assess the factors -
particularly the importance of q-SOFA score - related to the morbidity and mortality of septic patients in
surgical intensive care unit of a Malagasy hospital.
Patients and Methods
A descriptive and analytical retrospective study was conducted over a period of 24 months, from June
2015 to May 2017, in the surgical intensive care unit of the University Hospital of Antananarivo, JR
Andrianavalona (CHU JRA), Madagascar. All patients over 15 y.o. who were diagnosed with a sepsis state,
were included. The exclusion criteria were incomplete data files. Epidemiological, clinical, paraclinical,
therapeutic data and issue of patients were studied. The variables analyzed were demographic parameters
(age, gender), comorbidities, clinical parameters (systolic blood pressure (SBP), heart rate (RR), oxygen
saturation (SpO2), GCS, temperature), biological parameters (leukocyte count, platelet count, prothrombin,
C-Reactive Protein (CRP) and blood creatinine), the origin of the infection, the treatment undertaken and
the outcome of patients. The primary endpoint is patient mortality. The quantitative results are expressed
in median [Interquartile 25% - 75%] and the qualitative results are expressed in frequency. The Spearman
correlation test (with the correlation coefficient defined by R) vas used with a p-value of less than 0.05
considered significant (XLSTAT® 10.0).
Results
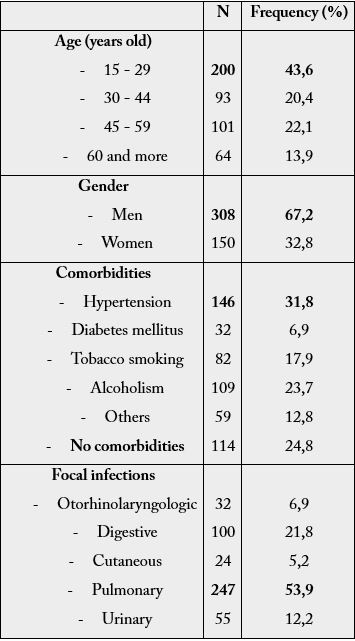
During the study period, 458 files were identified, with an incidence of 10.7% of admissions to the service.
The median age of patients was 36 [21-50] years, with a male predominance (sex ratio = 2.06). Most of
patients (75.2%) had comorbidities dominated by high blood pressure. The origins of the infection were
dominated by the pulmonary (53.9%), gastrointestinal (21.8%) and urinary (12.2%) focus (Table 1). It
was observed that 190 patients (41.5%) had a GCS less than 15. The SBP was 120[100-140]mmHg, the
HR was 109 [92-122]bpm, the RR was 28[23-36]cpm, the temperature was 38.4[38.1-39.0]°C. About the
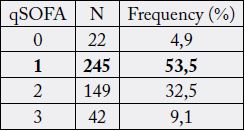
q-SOFA score, 245 patients (53.5%) had a score of 1 and 42 patients (9.1%) a score of 3 (Table 2).
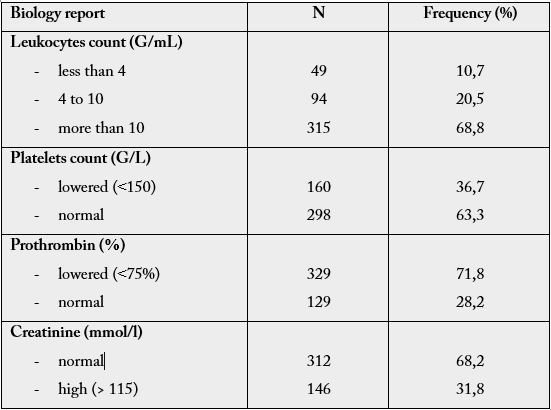
For biological results (Table 3), 315 patients (68.7%) presented leukocytosis, 49 patients (10.7%) leukopenia, 160 patients (34.9%) thrombocytopenia, 329 patients (71.8%) TP lowered (less than 75%). Renal failure (elevated blood creatinine) was found in 146 patients (31.8%). The median CRP was 132.5 [72.5-172] mg/L (Table 3). The treatments used were mainly probabilistic antibiotherapy and 17% of patients received targeted antibiotics after bacteriological results. Vascular filling, use of vasoactive amines (norepinephrine) was realized for 13% and the use of hydrocortisone (in case of refractory septic shock) for 9%.
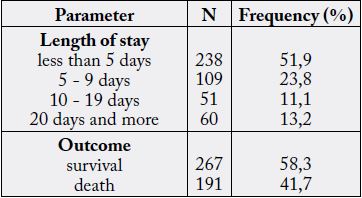
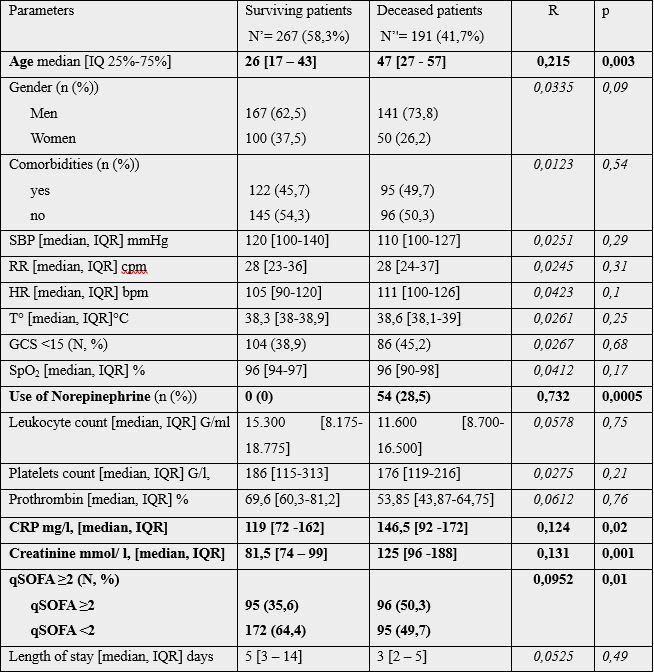
Median length of stay was 4[2-7] days; the mortality rate was 41.7% (Table 4). The correlation between mortality and the studied parameters are shown in table 5. A significant correlation was observed between patient mortality and age (p=0.003), CRP level (p=0.02), blood creatinine (p=0.001), q-SOFA score greater than or equal to 2 (p=0.01), use of norepinephrine (p=0.0005).
Discussion
For 24 months, 10.7% of admissions to CHU JRA surgical intensive care unit presented septic states, which
mortality was related to the use of norepinephrine (R=0.732), the age of the patient (R=0.215), the elevation
of blood creatinine (R=0.131) and the q-SOFA score (R=0.0952).
The age of the patient in our study was young compared to African (Moroccan and Congolese) studies that ranged from 48 to 50.6 years old, and French studies where 61.6% of which were over 60 - 71.2 years old [5-8]. Like in our study, the sources of infection remain mainly, in decreasing order, pulmonary (with an increasing frequency), then digestive and urinary [7,8]. The site of the initial infectious site at the origin of the septic shock can vary, as in a Moroccan study where this site is essentially abdominal (41%), pulmonary (19%) and urinary (11%); the other localizations are much rarer [5].
The length of stay in our study was quite similar with the literature which is 5.25±4.81 days with extremes of 24 hours to 30 days [5,9]. The length of stay in intensive care and resuscitation unit is increasing from 8.5 days to 11 days in the 90s, to 9 days to 22 days in 2011 [8,10-12].
In our study, the mortality rate was 41.7% and we observed five factors related to the mortality of septic states: high age, high CRP, elevated blood creatinine (indicating renal impairment), qSOFA score greater than or equal to 2, the use of vasoactive treatment. According to the literature, mortality in intensive care for patients with septic shock has been decreasing over the last twenty years, from 60.1% in 1993 to 39.5% in 2010 [7,8]. Hospital mortality also decreased from 62% in 1997 to 48.7% in 2011 [13]. The main risk factors for death in septic patients are age and severity scores (IGS II / SOFA), previous health status, presence of at least one comorbidity, and nosocomial infection [14,15]. In Morocco, in 2015, the prognostic factors for mortality were elevated Simplified Acute Physiology Score II (SAPS II), oligoanuria less than 500mL/24h, thrombocytopenia less than 100000/mm³, renal failure, pulmonary failure, hematological failure, neurological failure, and association of defects [5. In our study, the presence of comorbidities was not significantly related to septic-related mortality; despite the fact that 75.2% of the patients had at least one comorbidity.
The qSOFA score was used in our study to assess the severity of sepsis. This score based solely on clinical criteria seems to be more interesting in the local context, because of the non-use of paraclinical parameters. Indeed, the financial resources of the patients who support their medical expenses, often limit the achievement in time of these paraclinical analyses. A study by Wang JY et al [4] in 2016, showed that 28-day mortality was significantly higher in patients with qSOFA score ≥ 2 than in patients with qSOFA score <2 (42.9% vs. 17. 4%; p<0.001), as well as intensive care admission rate (33.3% vs. 16.0%, p<0.001).
The limitation of this study is its monocentric and retrospective characteristic. A multicentric study would be a perspective. However, following this study, the qSOFA score could be proposed to determine the link with the mortality of sepsis in resuscitation / intensive care, or even in other units. This easy-to-establish score could also make it easier to refer patients from other units to intensive care / resuscitation unit.
Conclusion
Septic states are one of the medical priorities of the millennium. It was found that the parameters related
to the mortality of septic states in the surgical intensive care unit of CHU JRA, were a qSOFA score of at
least 2, advanced age, elevated CRP and high creatinine blood levels, use of vasoactive treatment. The SOFA
and qSOFA scores predict mortality and remain a reference. Also, when the biological parameters are not
available, the determination of the qSOFA score could assess mortality of the septic states in resuscitation /
intensive care unit; hence the proposal to introduce it into daily practice.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!