Biography
Interests
Rakotondrainibe, A.1*, Avotsihoarana, T. H.2, Rahanitriniaina, N. M. P.1, Randriamizao, H. M. R.1, Rajaonera, A. T.1, Ramanampamonjy, R. M.3 & Raveloson, N. E.4
1Surgical Intensive Care Unit - CHU JR Andrianavalona, University of Antananarivo, Madagascar
2Visceral Surgery Unit - CHU JR Andrianavalona, University of Antananarivo, Madagascar
3Gastrology, Enterology and Hepatology Unit - CHU JR Befelatanana, University of Antananarivo, Madagascar
4Medical Intensive Care Unit - CHU JR Befelatanana, University of Antananarivo, Madagascar
*Correspondence to: Dr. Rakotondrainibe, Surgical Intensive Care Unit - CHU JR Andrianavalona, University of Antananarivo, Madagascar.
Copyright © 2019 Dr. Rakotondrainibe, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Admission in intensive care unit is frequent for patient presenting non-variceal upper gastrointestinal
bleeding (NVUGIB). To determine prognosis of those NVUGIB, prognostic scores should be used,
but they are not always available at admission. The shock index (SI) is calculated from systolic blood
pressure (SBP) and heart rate (HR) could more easily assess morbidity and mortality, especially,
when biological and endoscopic data are hardly available like for Malagasy patients. The aim of this
study is to analyze the shock index in non-variceal upper gastrointestinal bleeding in intensive care.
In a six-year retrospective study in surgical intensive care unit of a Malagasy university hospital
(CHUA-JRA), patients admitted for NVUGIB, hemodynamic parameters were studied. The
correlations between the SI and the transfusion, the recurrence and/or the surgery, and the mortality
were evaluated and the receiver operating curves (ROC) curves of the hemodynamic parameters
were analyzed.
During this period, 1424 patients (45.84 ± 16.01 years, predominantly male were selected. The
SBP was 115.79 ± 23.43mmHg, the HR was 91 ± 15bpm, and the SI was 0.82 ± 0.23. The SI was
correlated with mortality, recurrence of bleeding or surgery (2.74% of cases), transfusion (52.11%
of cases). The SI was also more specific than SBP and HR. The mortality percentage was 3.72%.
Hemodynamic parameters should be collected and monitored during NVUGIB. The SI is easy to
calculate, so it would quickly assess the morbidity and mortality of patients presenting NVUGIB in intensive care.
Abbreviations
A: Area (under receiver operating curves)
CHU-JRA: Centre Hospitalier Universitaire Joseph Ravoahangy Andrianavalona
Introduction
Non-variceal upper gastrointestinal bleeding (NVUGIB) is a common cause of hospitalization, resulting in a
mortality of 2 to 14% [1,2]. Immediate management is based on clinical evaluation, paraclinical explorations,
in order to establish prognostic scores [2]. These different prognostic scores allow the initial assessment of
NVUGIB and define the clinical risk and prognosis of this pathology. In front of any admitted patient in a
hospital environment, the clinical examination is always carried out, since the admission of the patient until
its follow-up. In this clinical examination, the hemodynamic parameters can early assess the severity of the
hemorrhage and are undeniably needed in assessing the severity of NVUGIB [1,3-5]. These parameters
include HR and SBP, from which the SI is defined (SI = HR / SBP), determined for the first time by
Allgower and Burri, in 1967 [5]. The SI is studied in several areas, to assess the cardiovascular status of a
patient, to evaluate patients at risk of haemodynamic decompensation, to identify the risks and outcome
of NVUGIB, during the initial assessment or during hospitalization [1,3,4]. The study of this index in
the NVUGIB so, could be interesting. The hypothesis of the study being that the SI could be a factor of
morbidity and mortality in NVUGIB; therefore, the main objective of the study was to analyze the shock
index at admission in non-variceal upper gastrointestinal bleeding in surgical intensive care unit.
Materials and Methods
A retrospective, analytical study was conducted over a period of six years (2011 to 2016), in the surgical
intensive care unit of the J.R. Andrianavalona University Hospital Center (CHU JRA) in Antananarivo,
Madagascar. Patients admitted for non-variceal upper gastrointestinal bleeding were included. The
primary endpoint was blood transfusion and the outcome of these patients (recurrence and / or surgery
and mortality). The variables studied were demographic parameters (age and gender), characteristics of
NVUGIB, hemodynamic parameters (systolic blood pressure (SBP), heart rate (HR), shock index (SI)),
therapeutic management (transfusion, hemostasis surgery), evolution (recurrence and / or surgery and death).
The results are expressed as mean with standard deviation for the quantitative data and frequency for the qualitative data. The software used for statistical analysis is SigmaPlot® 10.0. The Pearson test was conducted to study the correlations between the shock index and the realization of transfusion, the recurrence and / or surgery and mortality; with R defining the correlation coefficient. An analysis of the ROC curves (Receiver Operating Curves) was performed to evaluate the specificity and sensitivity of hemodynamic parameters (SBP, HR and SI) with transfusion, recurrence and / or surgery and mortality. The area under the curve (A) has been studied. A value of p less than 0.05 was considered significant.
Results
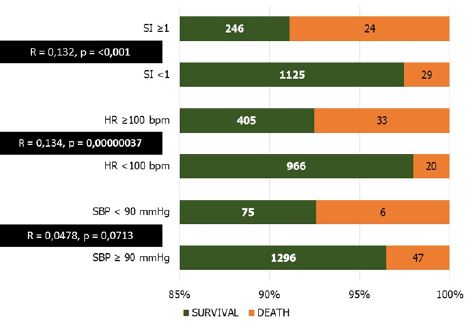
During the study period, 1424 patients with NVUGIB were included. The predominantly male study
population (sex ratio = 3.4) was 45.84 ± 16.01 years old. The hemorrhagic episode was inaugural in 73.52%
of cases. The presentation of NVUGIB was dominated by haematemesis associated with melena (45.71%).
About the hemodynamic parameters at admission, SBP was 116 ± 23mmHg, the HR was 91 ± 15bpm and
the SI was 0.82 ± 0.23. A SI was greater than or equal to 1 was present in 18.96%; a tachycardia of at least
100bpm was observed in 30.76% and a SBP of less than 90mmHg in 5.69%. In the study population, 275
patients (52.11%) were transfused, 39 patients (2.74%) had recurrence and / or hemostasis surgery and 53
patients (3.72%) died. Patients requiring a transfusion had an index of shock greater than or equal to 1
(6.32% of the total population and 50.00% of patients with an SI greater than or equal to 1), a tachycardia
was greater than 100bpm (8.92%) of the total population and 40.84% of patients with an HR greater than
or equal to 100bpm and a SBP was less than 90mmHg (1.83% of the total population and 47.27% patients
with PAS <90mmHg) (Figure 1). The SI was correlated significantly with transfusion and evolution (Figure
1).
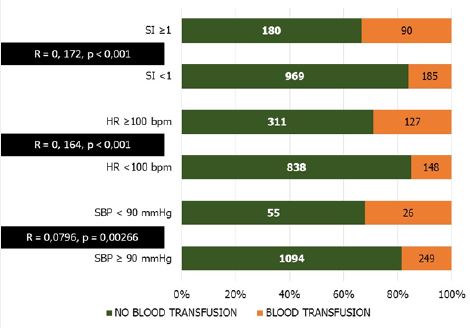
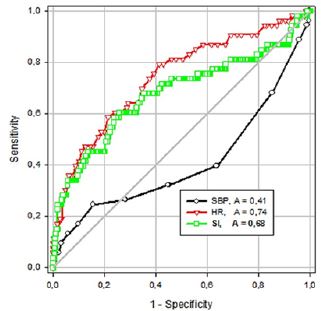
For transfusion, the area under the curve (A) of the shock index was 0.64, with a difference in areas of -0.22 ± 0.03 (between the SBP and the SI, p <0.0001) and -0.02 ± 0.01 (between HR and SI, p = 0.09564) (Figure 2).
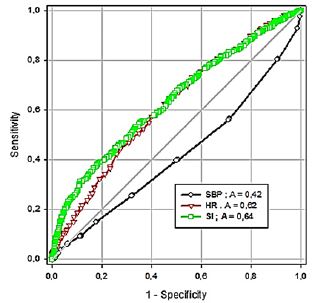
A SI of 0.96 had a specificity for transfusion use of 80% (sensitivity = 37%). Patients with a high shock index had a greater risk of recurrent hemorrhage and / or hemostasis surgery (Figure 3).
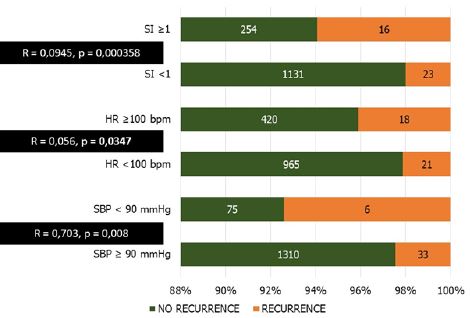
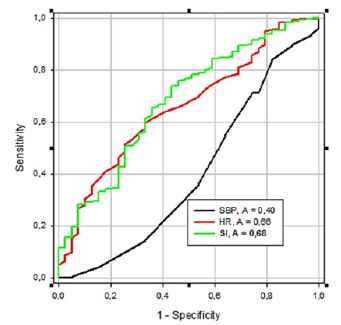
The SI had a better specificity for recurrence and surgery; for a SI at 0.98, the specificity was 80% (sensitivity = 41%, with A = 0.68) with a difference in areas with SBP of -0.27 ± 0.09 (p = 0.00218) and with heart rate of -0.02 ± 0.04 (p = 0.554) (Figure 4).
The SI also had a better specificity for mortality risk (Figure 5).
From a SI at 0.98 the specificity was 80% (sensitivity = 45%, A = 0.68). The difference in area between SI and SBP was -0.27 ± 0.09 (p = 0.0031) and that with HR was 0,061 ± 0.04 (p = 0.1039) (Figure 6).
Discussion
It was found that high values of the SI were more specific than the SBP in transfusion need, the risk of recurrence / hemostasis surgery and the outcome in NVUGIB. Some similarities in ROC curves were found between HR and SI.
In the literature, a renewed interest is observed for the study of the SI. With this index, it is indeed possible to determine four stages of the state of shock: I (SI <0.6 = no shock), II (between 0.6 and 1.0 = mild shock), III (1.0 to 1.4 = moderate shock) and IV (at least 1.4 = severe shock) [6]. Ratra A , [1] even define severe upper gastrointestinal bleeding when the SI is greater than 1.
We found that the SI was correlated with the need for transfusion and was more specific than HR and SBP. The SI is a good predictor of blood loss and hypovolemia [7,8]. This parameter is also a better predictor of blood loss compared to the SBP and the HR even at admission: A = 0.858 vs A = 0.165 (PAS) and A = 0.288 (HR) [6].
Rassameehiran S., et al. [4] find that the increase of the SI increases the need for transfusion. In fact, a SI of at least 1 increases by 52% the need for transfusion and an index of more than 1.4 by 79% [6]. Patients who have a SI > 1 at admission require a transfusion with an average of 4 blood units [9]. Sohn CH., et al. [10] found that a high SI increased the risk of massive blood transfusion by 9.47, whereas the HR multiplied it by only 1.06. The SI is also a good predictor of intra-hospital mortality in upper gastrointestinal bleeding, with a specificity of 80%, from a SI at 0.98.
From 0.7, the SI is predictive of short-term outcome and mortality at 30 days (A = 0.7, 56% / 79%) [3,4]. In addition, a SI of at least 1 resulted in intra-hospital mortality with specificity of 87 to 91% [5,11]. For the other factors, the SI is a determinant of the severity of blood loss in digestive haemorrhages, traumatisms and in the experimental setting. It also permits to assess the need for admission to intensive care units and endoscopic treatment. [3,4,6,12].
Thus, SI is easy to determine, and is available as soon as the patient is admitted. However, the limits of the SI are the possible modifications related to some pathological parameters, other than digestive haemorrhages. The use of the SI is then biased by factors varying SBP or HB [1]. For example, the presence of pain and anxiety can lead to tachycardia which can increase this index [7]. It is necessary also to compare the SI with other parameters or other scores. The strengths of this study are the sample size which is important enough for a Malagasy study. In addition, the study of a purely clinical factor, could be useful for admission or resuscitation to determine the evolution and outcome of NVUGIB, pending the establishment of the classic prognostic scores (Rockall, Glasgow Blatchford, AIMS65); because these scores often use paraclinical examinations whose realization is limited by the pecuniary resources of the patients in the local context. The weak points of this study are the monocentric character that does not reflect all patients with digestive hemorrhage. In addition, this study is limited by the fact that the other parameters that could have determined the need for transfusion, the recurrence of bleeding, the use of surgery and mortality have not been studied and that the comparison with the scores already known was not made.
Conclusion
The admission of patients with digestive hemorrhages in intensive care is necessary when those bleeding
are severe. Non-variceal upper gastrointestinal bleedings require rapid management during which the
hemodynamic parameters are essential and a priority. Among these parameters, the shock index is quick
and easy to determine - pending the establishment of other scores - and it is interesting, especially in the
context of Malagasy where paraclinical exams are not always available, in the evaluation of the evolution and
outcome of NVUGIB.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!