Biography
Interests
Tiliksew Liknaw1*, Mulugeta Tesfa2, Mathewos Mekonnen1, Tadele Kinati1 & Atsedemariam Andualem3
1Department of Nursing, Salale University, Ethiopia
2Department of Public Health, DebreMarkos University, Ethiopia
3Department of Nursing, Wollo University, Ethiopia
*Correspondence to: Dr. Tiliksew Liknaw, Department of Nursing, Salale University, Ethiopia.
Copyright © 2019 Dr.Tiliksew Liknaw, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Non-adherence to antiretroviral therapy is a major challenge to HIV/AIDS care. For antiretroviral
therapy to be effective, high level of adherence is required. So far, there is no study on determinant
of non-adherence to antiretroviral therapy in the study area. Therefore, this study was conducted to
identify determinants of non-adherence to antiretroviral therapy among HIV infected children in
Debremarkos and Felegehiwot referral hospital.
Case-control study design was employed on total of 220 samples in Debremarkos and Felegehiwot
referral hospital. Data was collected by using a structured pre-tested questionnaire and by data abstraction format from ART registration chart. Data was entered in to EPI data statistical version
3.1software and then exported to SPSS Windows version 20 for analysis. Binary logistic regression
analysis was conducted to find out association between dependent and independent variables.
Multivariate logistic regression analysis was done to identify independent factors for non-adherence.
Fifty five case and 165 controls were included in the study. The study showed that factors like
duration of HIV diagnosis to ART initiation [AOR=2.379,95% CI(1.150-4.921) ,duration on
ART use [AOR = 3.128; 95% CI (1.036-9.444)] ,types of ART drug [AOR = 4.752, 95% CI
(1.620-13.937)] , educational status of the care giver [AOR = 0.25, 95% CI (0.076-0.831)] ,follow
up schedule [AOR=2.567(1.148-5.740)] and difficulty during taking the drug[([AOR=5.867,95%
CI(2.200-15.645)] were the major identified significant factors for none adherence to ART
treatment in the study area.
The wider the interval of follow-up appointment the higher chance of non-adherence to ART.
Early initiation of ART after diagnosis HIV is protective against non-adherence. Therefore, the
capacity to effectively manage the above critical factor is crucial in the success of antiretroviral
therapy.
Introduction
Globally there were approximately 36.7 million people living with HIV (PLHIV) at the end of 2015 with
2.1 million people becoming newly infected with HIV. Sub-Saharan Africa is the most affected region, with
25.6 million PLHIV and accounts for two-thirds of the global total of new HIV infections. According to
Ethiopian Public Health Institution (EPHI) estimates and projections for Ethiopia for 2017, the national
HIV prevalence is 1.16% [1]. Furthermore, in 2012, 260,000 children less than 15 years were newly infected
and 210,000 died from AIDS-related causes. In the last decade, HIV has emerged as one of the leading
causes of childhood mortality and morbidity in sub-Saharan Africa [2].
WHO recommends antiretroviral therapy (ART) for all people with HIV as soon as possible after diagnosis without any restrictions of CD4 counts and strict adherence towards their medication is mandatory. Adherence is defined as the extent to which a patient takes a medication in the way intended by a health care provider. It is double burden in pediatric patients due to their age standard ART consists of fixed dose combination (FDC) of ART drugs to maximally suppress the HIV virus and stop the progression of HIV disease [3]. With regard to ART drugs, an adherence level of 95% or more is required in order to obtain successful outcome [4].
The ultimate goal of antiretroviral therapy is to achieve maximal and durable suppression of virus replication [5]. However, sub-optimal adherence to ART can lead to incomplete viral suppression, emergence of resistant viral strains and treatment failure. Non-adherence can also result in resistance to first-line ART and in such cases, patients often must switch to significantly more expensive second-line regimens which are more difficult to procure and more difficult for patients to access [6,7]. Switching to second-line therapy for children results in a more costly lifetime ART regimen, and is a major financial concern and human resource burden [8].
Many factors lead children’s to non-adherent to their treatment plan due to frequent dosing and are supplied in formulations that may be difficult for children to tolerate (large pills, bitter-tasting liquids, and gritty powders). Children fail to tolerate adverse effects of ART medications, since it is more frequent and severe. Antiretroviral syrups, which used in young children, require refrigeration. Some households don’t have any sort of refrigeration, and even those that do have, may not have enough space to store large quantities of these formulations [9]. Adherence is also influenced by factors associated with the disease and its treatment, with the relationship between the patient and the healthcare provider and with patients themselves, such as socio-economic status which is often based on employment or occupational status in addition to educational level and income [10].
Children rely on a caregiver, who often is also infected, to administer medication. These challenges may be exacerbated in resource-limited settings (RLS) that are most affected by the HIV epidemic. Often elderly family members have to care for children whose biological parents have passed away, and end up being burdened with multiple dependents while being frail themselves [11]. According to WHO report, the types of factors have been identified as barriers to optimal ART adherence; namely; regimen characteristics, patient characteristics [30]. Drug stock-outs, can hamper adherence with ART [12]. The study conducted in South Africa; transport affects the patient’s access and adherence to ART treatment and economy play an important role in determining the kinds of services that patients receive, the economic strains they experience, and their vulnerability to dropping out of treatment [13].
In Ethiopia in 2016 around 398,277 adults and 21,686 children under the age of 15 are taking ART. Based on the spectrum estimate the 2017 ART need is 665,116 for adults and 57,132 for children under 15 years of age. Recently ART service is being available in more than 1224 Health facilities of which around 909 are Health centers. On the basis of the new spectrum estimate for 2016, ART coverage for adults (age 15+) has reached 61% but the coverage remains low (33%) for children (age <15) living with HIV (1). In addition to low coverage in age group less than 15years in the country factors determining have not been studied in the study area. Therefore, the purpose of this is to identify determinants of non-adherence to ART among HIV infected children aged less than 15 years in Debremarkos and Felegehiwot Referral Hospitals, northwest Ethiopia.
Methods
This study was conducted in Debremarkos and Felegehiwot referral hospitals which are found in Amhara
regional state, Ethiopia. The hospitals have been giving services such as HIV counseling and testing, provision
of ART, treatment of opportunistic infections; prevention of mother to child transmission, TB/HIV co infection treatment, and care for HIV exposed infants. The numbers of children on ART at Debremarkos
and Felegehiwot Referral Hospitals was 323 and 305 respectively.
An institutional based unmatched case-control study was conducted from February to March 2018.
All children under 15 years with their primary care givers who are on ART at Debremarkos and Felegehiwot
Referral Hospital ART clinic during data collection were source population. All HIV positive children
under 15 years who had at least one month start ART before a data collection period was considered as a
study population of this study. All cases who had follow-up during the data collection period were included
in the study whereas controls were included by systematic random sampling techniques in every other Kth
appointees.
The sample size was calculated using STATCALC program of EPI version 7 Software. The minimum number of cases and controls required to achieve a 95% confidence level and power of 80%. Four controls were taken for each case. The minimum require sample size calculated using by inserting the above assumptions was 213, by adding 5% non-response rate the total sample size was 223.
The tool was prepared after reviewing literature. It was prepared in English and then translated to Amharic
and retranslated back to English to ensure its consistency. The questionnaire contains information on socio
demographic related variables, drug regimen related variables, and health care delivery related variables
and reason for non-adherence variables. Medical record was reviewed to identify clinical markers like CD4
count and WHO clinical staging.
The data were collected using clinical record review and interview. Three BSc nurses and three expert case managers working in ART clinics supervised by two BSc nurse experienced professionals. Baseline information was filled out from ART registration and follow-up forms. One day training on the objective of the study, confidentiality of information and interviewing techniques was given.
The outcome variable was non- adherence to ART and explanatory variables were: Patient or family /care giver related factors, medication and clinical related factor, health care delivery system related factor and social or environmental factors.
Data were coded and entered in to EPI data statistical version 3.1software and then exported to SPSS
Windows version 20 for further analysis. Descriptive statistics was computed for each variable. Bivariate
logistic regression was used to check variables associated with the dependent variable. Those variables found to have p-values of ≤0.2 was fitted to multivariable logistic regression to control the effects of confounders.
Odds ratios with 95% CI are computed and variables having p-values less than 0.05 in the multiple logistic
regression models was considered significantly associated with the dependent variable.
Non-Adherence (cases): patients who had a history of they took less than 95% missing the prescribed doses
or fixed hours (missing 1 doses out of 7 doses or 2 doses out of 14 doses) all of scheduled regimens which
supposed to take in a week.
Adherence (controls): were near-perfect (>95%) take to dose of all regimens as prescribed with fixed hours which supposed to take in a week.
Primary Care giver: People who lives with the child and participates in the child’s daily care and take the responsibility in giving the child medication and bring the child to clinic.
Ethical clearance was obtained from the Ethical Review Committee of the Debremarkos University, college
of health science. Permission letter was obtained from Debremarkos and Felegehiwot Referral Hospital.
Each caregiver/subject was adequately informed about the purpose of the study and written informed assent
was obtained from the parents/guardians. Interviews were conducted in private rooms and confidentiality
was kept. They were informed to withdraw from study at any time and/or to refrain from responding to
questions if they were not interest to participate by any reason.
Result
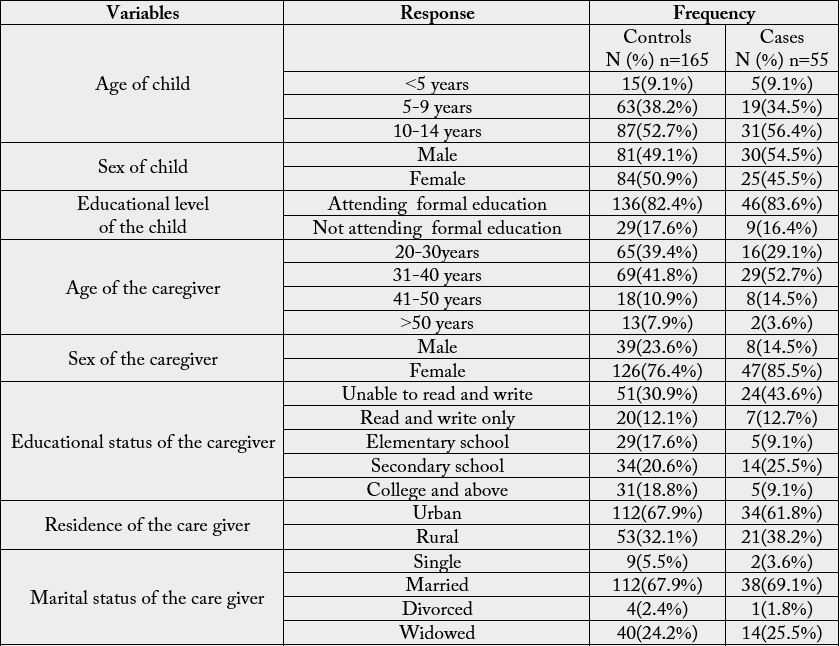
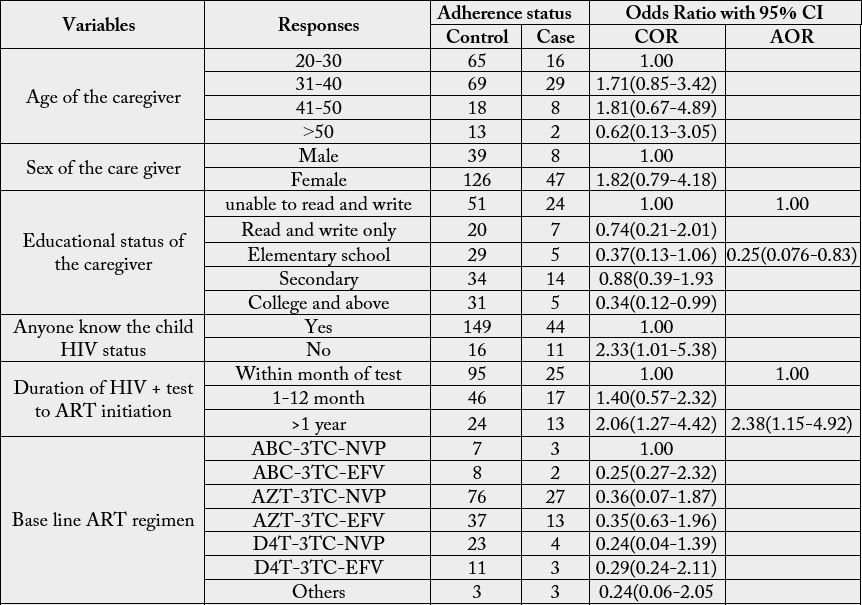
A total of 220 HIV-positive children 55 (25%) cases and 165 (75%) controls) who had at least one month
ART follow up participated in the study with response rate of 99.4%. Among the study participants 50.45%
(30 cases and 81 controls) were male. Majority of 90.9% (50 cases and 150 controls) were above the age
of five years. Furthermore, majority of 78.6% (47 cases and126 controls) of the children’s care takers were
females. The mean age ± (SD) of the children at the time of data collection were 9.3years (±3.25). The mean
age ± (SD) of the caregiver at the time of data collection were 35.5 (±8.39). The reported length of time
the children stayed on ART ranged from 4 month to 149 months and the mean were 70.5 months. Those
who were unable to read and write accounted for 34.0% (24 cases and 51 controls). Regarding occupation,
30.9% (16 case and 52 controls) were merchant and 68.2% (38 cases and 112 controls) of the caregivers were
married. Seventy-nine percent of (44 cases and 130 controls) reported an average monthly family income of
greater than 500ETB (Table 1).
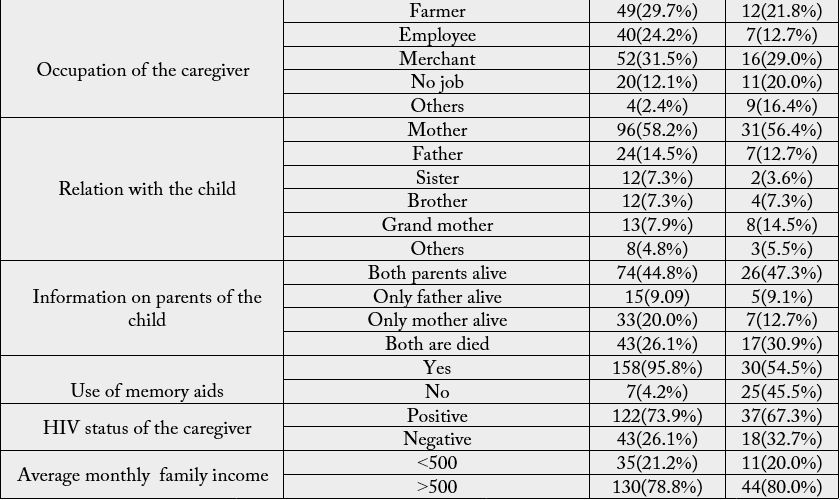
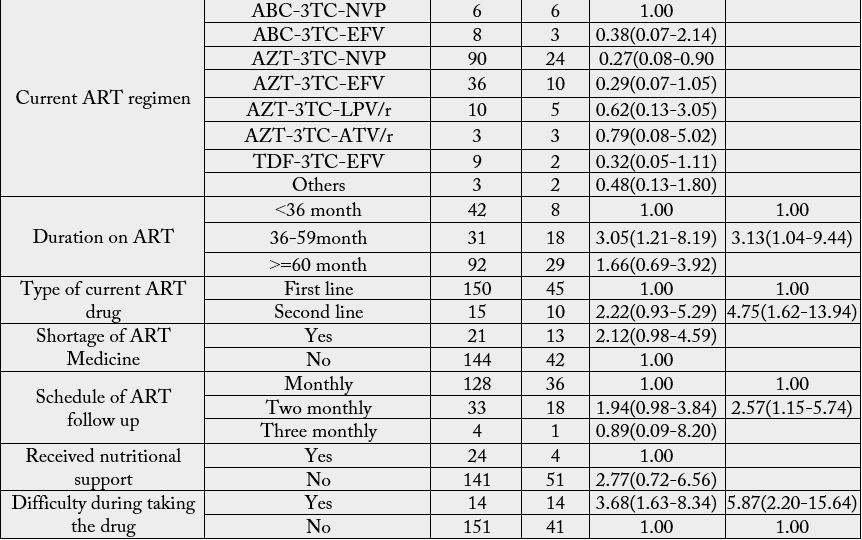
The majority of 46.8% (27 cases and 76 controls) of children in this study were on AZT+3TC+NVP
based Regimen at baseline and similar with the baseline, about 51.8% (24 cases and 90 controls) children
were currently on AZT-3TC-NVP based regimen. About 55% of the children in this study were on ART
for greater than 60 months. Regarding on types of ART drugs 88.2% (45 cases and 150 controls) of the
children was on first line regimen (Table 2).
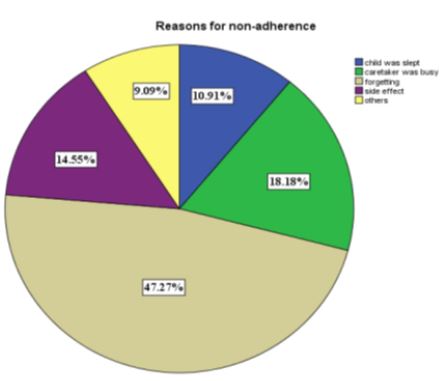
Forgetting, care taker being busy, side effect, the child was slept, and others, were the most common reasons
mentioned by of care givers of the children who were missed their doses respectively.
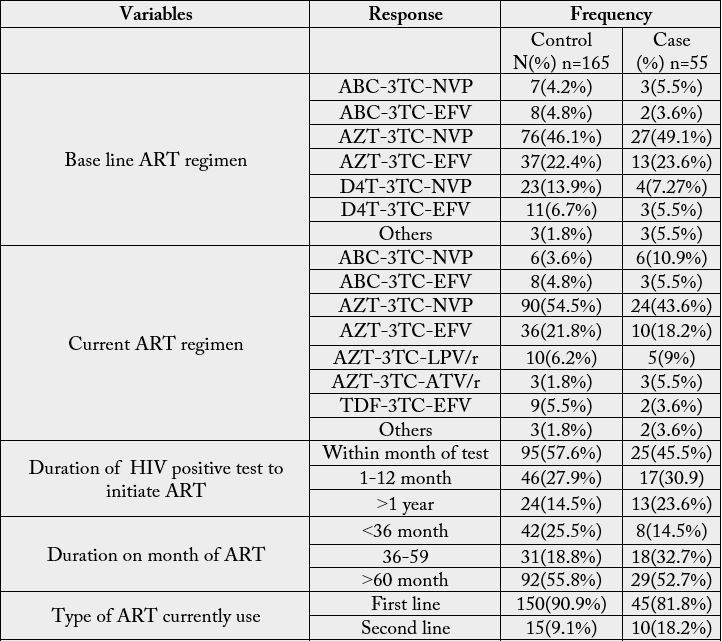
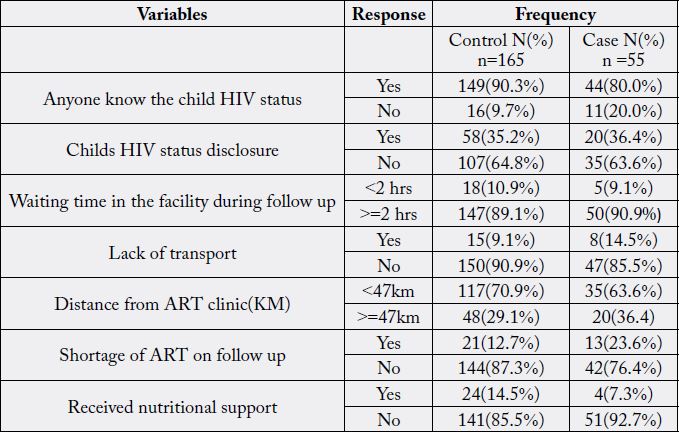
The majority of patients 87.7% (44 cases and 149 controls) disclosed their status to family members and for
other peoples. Sixty nine percent (35 cases and 117 controls) of individuals were more often living less than
47km away from the ART clinic and 89.5% (50 cases and 147 controls) were spending their time more than
2 hours in the health facility (Table 3).
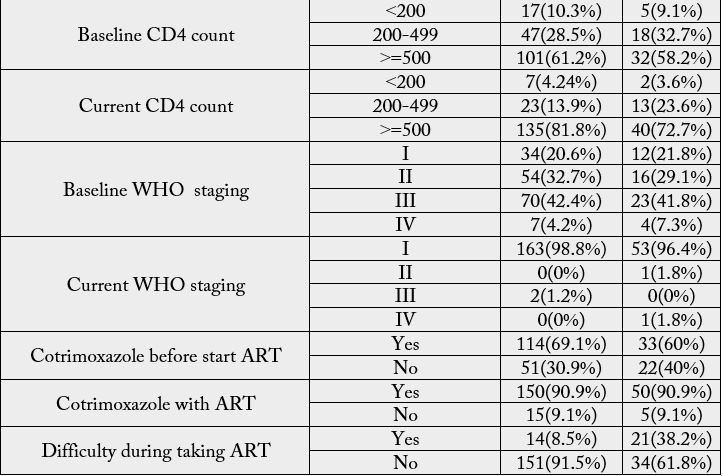
HIV positive children who had received ART medication used after 1 year of diagnosis of HIV were 2.4
times more likely to not adhere as compared to those who had received ART medication within a month
[AOR=2.379, 95% CI (1.150-4.921). Patients who had more than 36 month ART follow-up were 3.1
times more likely to not adhere as compared to those who had <36 months follow-up [AOR = 3.128, 95%
CI (1.036-9.444)]. The odds of non-adherence were 4.8 times more likely occur to those who had on second
line drug as compared to those who had on first line drug [AOR = 4.752, 95% CI (1.620-13.937)]. The odds
of non-adherencewere75% times less likely to occur among the care giver those who had elementary school
as compared to those who had unable to read and write. HIV positive children who had taking medication
for two month were 2.6 times more likely to being non-adherent as compared to those who had taking the
drugs monthly [AOR=2.57(1.15-5.74]. In addition, the odds of non-adherence were 5.9 times more likely
to those who had difficulty during taking the drug as compared to the counterpart [AOR=5.87,95% CI
(2.20-15.64)] (Table 4).
Discussion
This study also tried to examine the different variables associated with child non-adherence to ART Clinical
record review, interview were used to identify Non-adherence factors along with the caregiver characteristics.
In this study, such as, educational status of the care giver, duration on ART, type of ART drug, schedule for
follow up and duration of HIV diagnosis to ART initiation, difficulty during taking the drug; were found to
be independent determinant factors with non-adherence to ART.
Caregivers of non-adherent children reported that missed doses were most often due to forgetfulness; care taker was busy, drug side effects, and others. This finding in the current study is consistent with a study [7,14- 17], which found that missed doses were most commonly due to forgetfulness. The odds of non-adherence was 75% times less likely to occur among those who had elementary schools as compared to those who had unable to read and write, these finding is supported by the study conducted in Fiche hospital [14]. This finding of non-adherence was not being related to the age and sex of the child and it was not in agreement with reports from other studies [7,14-18]. The possible explanations for such differences could be possible progressive improvement of patient care and management systems with time; and difference in study design.
This study showed that patients who had 36-59 month on ART follow-up were 3.1 times more likely to not adhere as compared to those who had less than 36 months follow-up [AOR=3.12,95% CI (1.04-9.44)]. This finding is inconsistent with study conducted in India and Nigeria [6,7]. The possible reason could be these studies were included those patients who had less than 6 months’ duration on ART. On top of the treatment duration of the patients, the accessibility of health facilities, living conditions, socio-demographic characteristics of the population in south India and Nigeria is differ from Ethiopia which might have effect on the adherence status of the patient. And when the duration of ART increases there might be treatment fatigue and side effect can get worse the longer a drug is taken, tend to neglect their ART regimen over a period of time.
The odds non-adherence were 4.8 times more likely occur to those who had on second line drug as compared to those who had on first line drug [AOR = 4.75, 95% CI (1.62-13.94)]. This finding is consistent with done in Mekelle [16]. The possible explanation for this might be children on second line regimen due to formulation of the drug in (size, taste, pill burden) and unavailability of the drug which is too expensive is make it to non-adherent for ART.
HIV positive children who had taking medication every two monthly were 2.6 times more likely to nonadhere as compared to those who had taking the drug monthly [AOR=2.57, 95% CI (1.15-5.74)]. This finding is not significantly associated with adherence in other studies in Fiche Hospital [14]. The possible reason for this could be, in current study patients follow-up appointment were: monthly, every two month and every three month appointment, but in Fiche Hospital appointment was below monthly and monthly.
HIV positive children who had received ART medication used after one year of diagnosis of HIV were 2.4 times more likely to not adhere as compared to those who had received ART medication within one year [AOR=2.38,95% CI (1.15-4.92)]. The possible explanation for this might be the delay of early linkage by health care provider to the chronic follow up, poor counseling of the care giver about importance of early initiation, poor awareness of the caregiver towards the ART drugs and poor care system. The odds of nonadherence were 5.9 times more likely to those who had difficulty during taking the drug as compared to the counterpart [AOR=5.87,95% CI (2.20-15.64)]. The possible explanation for this might be the formulation of drug in (size, taste), treatment fatigue, pill burden of the drug makes it difficult to take the medicine inappropriately.
Limitation of the Study
None inclusion of socio-cultural and behavioral related factors towards non-adherence is one limitation.
Health related effect on non-adherence may be affected to some extent by social desirable; however, it was
minimized by different strategy like interviewing in private rooms. And also adherence assessment was
based on the caregiver self-report through interview which may have social desirability bias and recall bias.
Conclusion
In conclusion, the non-adherence was more likely occur to those who had on second line drug as compared
to those who had on first line drug. HIV positive children who had taking medication every two monthly
were more likely to non-adhere as compared to those who had taking the drug monthly. HIV positive
children who had received ART medication used after one year of diagnosis of HIV were more likely to
not adhere as compared to those who had received ART medication within one year. The non-adherence
were more likely to those who had difficulty during taking the drug as compared to the counterpart. This
study also showed that patients who had 36-59 month on ART follow-up were more likely to not adhere as
compared to those who had less than 36 months follow-up. Therefore, the wider the interval of appointment
the higher chance of non-adherence to ART. Early initiation of ART after diagnosis HIV is protective
against non-adherence.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Data Availability
All the necessary data are available.
Sources of the Fund
The study was conducted by self sponsor.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!