Biography
Interests
Dejene Hailu*, Mathewos Mekonnen & Bikila Tesfa
Nursing Department, College of Health Sciences, Salale University, Fiche, Ethiopia
*Correspondence to: Dr. Dejene Hailu, Nursing Department, College of Health Sciences, Salale University, Fiche, Ethiopia.
Copyright © 2019 Dejene Hailu, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Vaccination is a proven immunization tool in preventing and eradicating communicable diseases. Despite increase in global immunization coverage, many children around the world especially in developing countries still left unvaccinated. To assess expanded program on immunization coverage and reason for drop out among children age 12-23 months in Jigjiga town Fafan zone eastern Ethiopia. Community based cross sectional study was conducted from February to June, 2017. Data was collected by using structured questionnaire through interview and observation of card. Data was analyzed manually using tally sheet and descriptive data was presented using table and diagram The overall dropout rate was 95(24%) and 79(21) were not immunized at all. The coverage for BCG vaccine was 332(87.5%) and for Penta-1 was 318(83.9%) and for Penta-3 was 216(56.9%) and for measles was 185(48.4%) and vitamin A 185(48.4). Concerning immunization status of mothers only 47(12.4%) of them completed up to TT5. Based on the finding, the overall dropout rate from immunization was very high that outbreak can happen possibly by measles with its sever sequel as majority of children defaulted and didn’t immunized for measles. Therefore, concerned is recommended to increase immunization coverage through different strategy.
Introduction
Vaccination has been shown to be one of the most effective public health interventions worldwide, through
which a number of serious childhood diseases have been successfully eradicated. Small pox was eradicated
by the immunization campaign carried out by World Health Organization (WHO) from 1967 to 1977 [1].
The WHO recommends vaccination against a number of serious infectious diseases, including diphtheria, tetanus, Pertussis, HepB, invasive Hib disease, and measles for all children, and against pneumococcal disease, yellow fever, and rotavirus disease for children in some areas as part of their EPI. However, many infants and children still die every year from these diseases. It has been shown that in 2007 approximately 27 million infants are not vaccinated against common childhood diseases, such as measles or tetanus. As a result, 2-3 million children are dying annually from easily preventable diseases, and many more fall ill [1]. But in the same year, 24 million children are not being reached with vaccines and over 10% of children under one year old in developing countries were not receiving even one dose of DTP vaccine, compared with 2% in industrialized countries [2]. An estimated 2.1 million people around the world died in 2002 of diseases which can be prevented by widely used vaccines. This toll included 1.4 million children under the age of five years. Among these childhood deaths, over 500 000 were caused by measles; nearly 400, 000 by Hib; nearly 300,000 by Pertusis; and 180, 000 by neonatal tetanus [1]. It has been also recognized that vaccine preventable diseases are responsible for 16% of under-five mortality in Ethiopia [3].
Although estimated global routine vaccination coverage with the first dose of measles containing vaccine (MCV) reached 82% in 2007, nearly 23.2 million of children missed the vaccine of which 15.3 million (65%) resides in eight countries of Africa and south Asia. From these 1 million of them live in Ethiopia [4]. Despite the increased report immunization coverage of measles in Ethiopia, the disease has continued to be the main childhood health problem in the country. It attributed to 4% of child and infant deaths in 2004 which was highest of the world [5]. But in Ethiopia the incidence of measles has increased from 3.19/100,000 (1964 confirmed cases) in 2009 to 7.35/100,000 (3121 confirmed cases) in 2010 [6]. According to the Ethiopian Demographic and Health Survey (EDHS) 2016, only 30% of children age less than 23 months of age was fully vaccinated and 18% of children did not receive any vaccination. Accordingly, children are more likely to be vaccinated the first doses of vaccination than the third and the fourth doses in which 65% of children received Bacillus Chalmette- Guerin (BCG) and from these only 35% of them receive measles vaccine which is the last vaccine dose in EPI program of Ethiopian. This shows that there is a high rate of drop out from vaccination [7]. The study done in Ethiopia showed that immunization coverage by routine vaccination was less than 20% with card and less than 50% with card and history [8]. In Ethiopia, low access to services, inadequate awareness of caregivers, missed opportunities, and high dropout rate are major factors contributing to low immunization coverage [9]. Therefore, the aim of this study was to assess coverage factors affecting the immunization status among children ager less than 23 months of age in Jigjiga town and to generate data that could be used for better planning and strengthening of immunization services.
Objective
• To assess expanded program on immunization coverage and reasons for non-immunization among
children age 12-23 months in Jigjiga town, Fafan zone, Somali region, and Eastern Ethiopia.
• To assess expanded program on immunization coverage among children age 12- 23 months in Jigjiga
town
• To assess reasons for non-immunization among children age 12- 23 months in Jigjiga town
Method and Materials
A cross sectional study was conducted in Jigjiga town Keble 10 from February to June, 2017. Jigjiga is town
in eastern Ethiopia and the capital of the Somali Region of the country. The dominant ethnic group living in
the town was Somali (99.0%), the next three largest groups were the Amhara (0.25%), the Oromo (0.44%),
and the Gurage (0.30%); all other ethnic groups accounts 0.08% of the population. This city is the capital
city settlement in Jijiga and agro-pastoral in their life style.
All under 12- 23 month children living in Jigjiga town were source population. The study population was
mother with children age 12-23 months living in selected kebeles.
Sample of this study was calculated single population proportion formula based on the following parameters
Where, P=41% [10] and d=5%. Therefore final sample size was 379 children. Three kebeles were selected
purposely and systematic random sampling was employed to select eligible household from the kebeles. Every
mother from each household was selected until the required sample size achieved; the starting household
was selected using a lottery method.
Structured questionnaire was prepared in English and translated into Somali language in order to facilitate
better understanding of respondents. Data was collected by data collectors and supervised by principal
investigators.
Pretest was done one week before the actual survey and it was carried out in Jijiga in other Keble with
similar character of 5% of the study population and necessary modification was made before it is applied
on the study population. The quality of data was maintained by through pretesting of the tool, continuous
supervision by supervisors and the collected data was checked for completeness before analysis is made.
The data was analyzed manually by using scientific calculator and tally sheet. Descriptive statistics was be used to illustrate the socio- economic and demographic characteristics of the study population. The response of respondent for the questions was calculated and presented using tables and diagram.
Prior to data collection letter was written from Jigjiga University college of medicine and health sciences
and communicated to Jigjiga city administration. Data was collected after getting both verbal and written
consent through brief explanation of the objectives of the research. In order to keep the confidentiality of
the data, name of respondents was not included in data collection tool.
Results
This study covered 379 children and their mother/ care takers giving 100% respondent rate of study population.
The majority of children were females 202(53%) and males account 177(46.6%). Among 379 children
208(55%) were fully immunized. The overall dropout rate was 95(24%) and 79(21) were not immunized
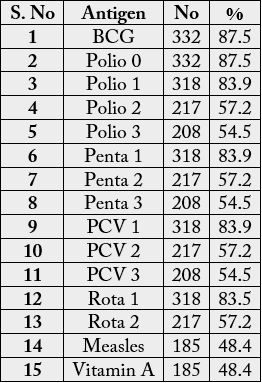
at all. The coverage for BCG vaccine was 332(87.5%) and for penta1, 318(83.9%) and for penta3 was
208(54.5%) and for measles was 185(48.4%) and vitamin A 185(48.4%).
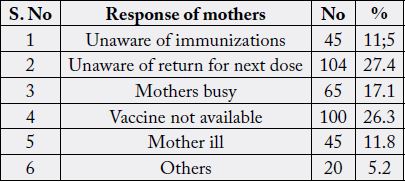
The main reason for not immunizing or defaulting from EPI was mother busy 65(17.1), unaware of return for next dose 104(27.4%), mother ill 45(11.8%), unaware of immunization 45(11.1%), vaccine not available 100(27.4%) and other reasons account 22(5.2%).
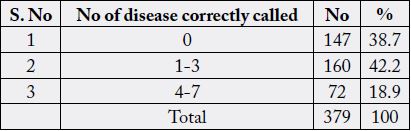
Mothers/care takers were also asked about number of vaccine preventable disease and 147(38.7%) of them failed to respond, 160(42.2%) of them respond 1-3 vaccine preventable disease, 72(18.9%) respond 4-7 vaccine preventable disease (Table 3).
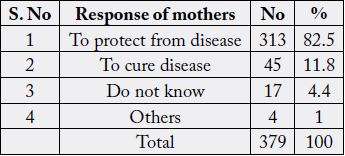
Mothers/care takers were asked about the benefit of immunization and 313(82.5%) of them respond to prevent from disease, 45(11.8%) to cure disease and 17(4.4%) of them do not know the benefit of immunization and 4(1%) were others (Table 4).
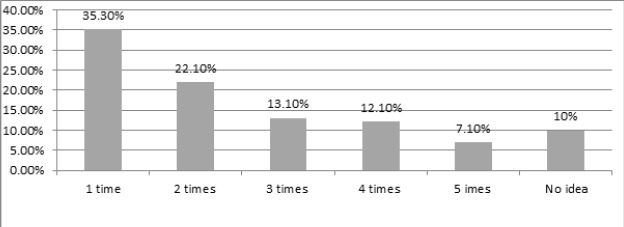
When mothers/ care takers were interviewed about frequency of their own schedule, only 134(35.3%) know that they take one time of TT. Whereas 230(60%) replied 1-4 and 42(11%) had no idea.
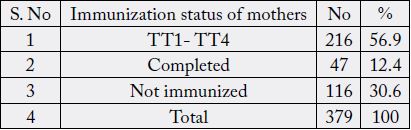
Mothers were also evaluated for their vaccination and accordingly 47(12.4%) of them were completed, 116(30.6%) of them were took TT1-TT4 while 216(56.9%) were not immunized (Table 5).
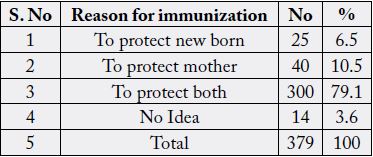
Mothers/ care takers were also asked reason for their own immunization, 300(79.1%) mothers respond to protect both mother and child, 25(6.5%) respond to protect new born, 40(10.5%) respond to protect mother and 14(3.6%) had no idea (Table 6).
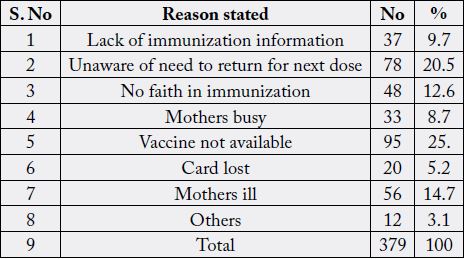
The main reason for not vaccination for TT were lack of immunization information 37(9.7%), unaware of return fir next dose 78(20.5%), no faith in immunization 48(12.6%), mothers busy 33(8.7%), vaccine not available 95(25%), mothers ill 56(14.7%) and others account 12(3.4%) (Table 7).
Discussion
In this study 55% (208) Children were fully vaccinated. When compared to other study carried out in Adami
Tullu woreda in which 37% of the same age group was fully vaccinated and this study shows slight higher
coverage this variation may be due to difference in study area and awareness creation work done overtime.
Moreover, the current study was done in urban where heath service is easily accessible [11]. The coverage
in this study was 54.5% for DPT3 and 48.4% for measles. There was variation in coverage in Tigray region
Tselemti which is 97.2% and 75.5% respectively and the possible reason for such variation may be due to different in level of awareness, educational status and may be due to different in level of knowledge in study
population. It may also be due to different in study area and sample size [12].
More over the result of this study showed that 55 % of children were fully immunized, 24% of them were defaulters and 21% of them were not vaccinated at all. The majority of reasons for not immunizing or defaulting were mothers busy (17.5%), unaware of return to next dose (27.4), mothers sick (11.8) and unaware of immunization (17.1%).
In this particular study TT vaccination coverage accounts 56.4%, but only 29% of them completed five doses. When compared to survey conducted in Gonder town and Adami Tullu woreda it was relatively high because of different in sample size, study area and may be due to different in level of awareness on immunization [11,12].
Conclusion
In this study it was found that overall dropout rate from immunization schedule was high that an epidemic
out break can happen possibly measles with it’s sever sequel as majority of children defaulted and didn’t
immunized for measles. In spite of tetanus also being major problem TT coverage for mothers/care takers
was very small that reflecting neonatal tetanus could put the lives of neonate in danger. Mothers /care takers
were not have enough awareness about immunization and need to repeat dose of immunization for their
children and themselves. Also mothers did not keep the immunization card of their children and themselves
that evaluation of immunization status of study population is very difficult.
Competing Interests
All authors declare there is no conflict of interests.
Author’s Contribution
Students initiated the study, contributed to the study design, coordinated the data collection process and
analyzed the data. Mathewos Mekonnen contributed to the study design, reviewed survey instruments, participated
on data analysis and commented on the manuscript. Dejene Hailu contributed to the study design,
survey instrument development, and data analysis and wrote the manuscript. All authors read and approved
the final manuscript.
Acknowledgments
We would like to thank all study participants and data collectors for their contribution in success of our
work.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!