Biography
Interests
Ogbonna Brian, O.1,2*, Nwokoye Fredrick, O.1, Onwuchuluba Ebere3, Eze Uchenna, H. I.4, Osuafor Nkeiruka, G.6, Ohiaeri Ifeyinwa1, Nwafor Maureen, N.1, Okechukwu Raymond, C.1, Oluigbo Kennedy1, Offu Ogochukwu1, Ejieh Loveth, I.1, Okpalanma Nneoma, N.1, Mmaduekwe Hilda, N.1, Umeh Ifeoma, B.1, Ezenekwe Lizzette, N.1, Uzodinma Samuel, U.1, Okeke Anthony1, Anetoh Maureen, U.1, Adenola Ugochi, A.1, Maduabuchi Ihekoronye, R.5, Omuta Michael6, Egere Eustace, C.6, Nnamani Monica6, Onwuma Malachy, U.6
1Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences, Nnamdi
Azikiwe University, Awka, Nigeria
2Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, King David University of
Medical Sciences, Uburu, Nigeria
3Department of Clinical Pharmacy and Bio-Pharmacy, Faculty of Pharmacy, University of Lagos
4Department of Clinical Pharmacy and Biopharmacy, Faculty of Pharmacy, Olabisi Onabanjo University, Sagamu
Campus, Sagamu, Ogun State, Nigeria
5Department of Clinical Pharmacy and Pharmacy Administration, Faculty of Pharmacy, Obafemi Awolowo
University, Ile Ife, Oshun State, Nigeria
6Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, Madonna University, Elele
Nigeria
*Correspondence to: Dr. Ogbonna Brian, O., Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, Awka & Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, King David University of Medical Sciences, Uburu Nigeria.
Copyright © 2023 Dr. Ogbonna Brian, O., et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
The practice of clinical pharmacy and pharmaceutical care has facilitated the improvement of quality
of life via clinical, economic and humanistic outcomes. However, in Nigeria, we have paucity of
evidence-based data. This study evaluated the services, perceptions and barriers to clinical pharmacy
practice in Nigeria from physicians and pharmacists’ perspective.
A cross-sectional survey was conducted among physicians and pharmacists from two hospitals in
south-east Nigeria using questionnaires in the months of June and July, 2019. The questionnaire was
adapted from similar study use to assess the services, perception and barriers of pharmacist about
Clinical Pharmacy practice in Nigeria. This study was done with permission from the institutions
and with approved consents from 400 respondents. The result was summarized with descriptive
statistics and Chi square. A p<0.05 was considered significant.
Among the respondents were, 250 physicians, and 150 pharmacists. Majority of the respondents are
male (68%) within the age of 21-29 (66.3%). Most all the respondents have attained first degree
(84.3%) and within the practice year of 1-10 years (83.8%). Most of the physicians indicated
that recommendations made by pharmacist are sometimes accepted by prescribers (78.9%) and,
that physicians share their therapeutic knowledge with pharmacist (78.4%). The study suggested a
difference (p-0.016) between respondents who indicated that emphasis on drug therapy was placed
to patients in order to improve patients care and quality of life.
The respondents had good perception and attitude towards clinical pharmacy practice. However,
the results suggested that the clinical pharmacy services were poor. The barriers stemmed from
physicians lack of understanding of the expertice and services of a clinical pharmacists which limits
interaction and collaboration with the physicians.
Introduction
Clinical pharmacy practice is relatively a new discipline in pharmacy practice in which the emphasis is
transferred from product oriented to patient-oriented practice [1]. However, the definition of clinical
pharmacy practice or clinical pharmacy has not been universally touched stoned. Clinical pharmacy has
different definition through the world but some recognized definitions are. Clinical pharmacy is a health
science discipline in which pharmacists provide patient care that optimizes medication therapy and promotes
health, wellness and disease [1]. Clinical pharmacy practice is the practice of pharmacy as a multidisciplinary,
healthcare team directed at achieving quality use of medicine [1]. The “Thalidomide tragedy’’ wherein it
was found that consumption of popular sedative thalidomide resulted in birth of babies with sealed limbs,
second in 1968 phenytoin toxicity was reported in Australia which was because of change in formulation
that is switching over from calcium sulfate to lactose as an inert excipient in the tablet [2].
Clinical pharmacy started in the UK in 1960 as result to promote rational use of medication therapy, reduce cost of medications and increase patient quality of life. Some of the barriers to clinical pharmacy practice are; lack of clinical pharmacy training, lack of therapeutic knowledge and policy implementation problem [2]. The Clinical pharmacy has emerged as one of the latest branches of pharmacy in 21st Century. However, this journey was not easy, many barriers, restrictions was overcome with the optimism and persistent efforts of many pioneers who started with nothing. It all began with when pharmacists at the University of Iowa hospital. This helped in defining the Pharmacist’s Intervention in management of pharmacotherapy and made the clinical pharmacist a valuable member of healthcare team. Later on, the many other domains were added in clinical pharmacy from Therapeutic Drug Monitoring (TDM) to Anti-microbial Stewardship (AMS), [3]. Thus, lack of adequate practice of clinical pharmacy is a serious problem to the nation at large. Clinical pharmacy happens to be one of the vital parts in healthcare and it is difficult to determine how far clinical pharmacy has been implemented in Nigeria due to lack of research and proper documentation. This study evaluated the services, perceptions and barriers to clinical pharmacy practice in Nigeria from physicians and pharmacists’ perspective.
Methods
This research was a descriptive cross-sectional study which was questionnaire based.
The study was conducted in two tertiary health care facilities in Anambra State. Having most specialties in
medicine. The facilities were the Nnamdi Azikiwe University Teaching Hospital(NAUTH) and General
Hospital Onitsha. These sites were chosen due to availability of sufficient number of physicians, pharmacists,
and high patients turnout.
All physicians and pharmacists that indicated interest to participate in the study, and gave their informed
consent were recruited for the study. The sample size was calculated as shown below:
Where n= required sample size (unknown)
N=population size
E=maximum acceptable error margin at 5% degree of freedom (95% chances of being right) =0.05
For Physicians
N= estimated population size of Physicians in NAUTH =400
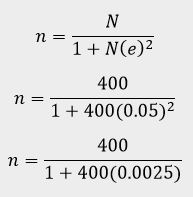
Attrition of 10 Physicians was used
200 + 10 = 210
The study was explained to the respondents and the procedure involved. Data collected was strictly kept
confidential. Those who gave their informed consent participated in the study. The questionnaire was
administered to them, filled and was retrieved.
The questionnaire was self-administered and was collected back after the respondents had finished filling
them same day.
Before the study commenced, ethical approval for the study protocol was obtained from the Research and
ethics. Department of both tertiary healthcare facilities. Informed consent was obtained from the respondents
before commencement of the study.
Data was collected from sample population using questionnaires. The questionnaires were retrieved and data
was analyzed using appropriate statistical method [4]. The questionnaires were pilot tested with 15 health
workers who were not included in the final study.
We summarized the data with descriptive statistics, mean, mode and median. We measured the differences
in frequencies of the outcomes variables with Chi-square test.
Study Criteria
All physicians and pharmacists that were willing to participate who have practiced for morethan 12 months
and were available during the time of the study.
Physicians and pharmacists that were willing to participate but were not available at the time of the study.
Physicians and pharmacists that were not willing to participate in the study at all.
A Pilot study was carried out by distributing 10 questionnaires to 10 physicians and pharmacists each and
the questionnaires were retrieved. Those that were used in the pilot study did not participate in the main
study.
Results
Of the 500-questionnaire instrument distributed, four hundred were returned as validly completed giving a
response rate of 400 (80%).
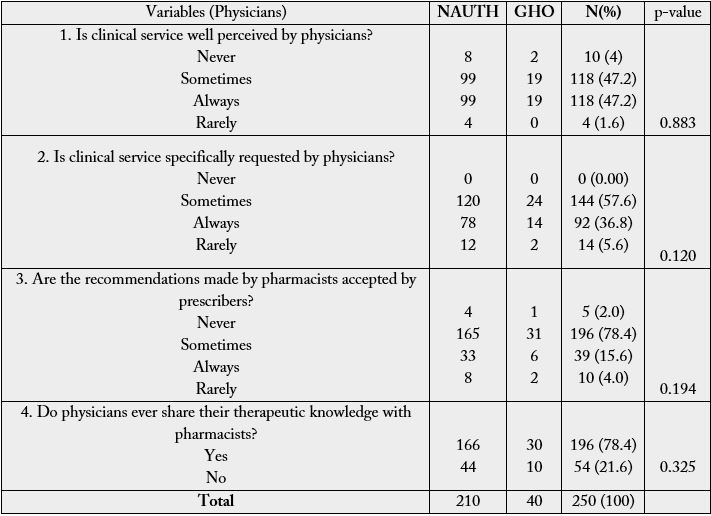
In table 1, among the respondents (Dr), 210 (84%) were from Nnamdi Azikiwe University Teaching Hospital (NAUTH) while 40 (16%) were from General Hospital Onitsha. There were 187 (74.8%) male and 63 (25.2%) females among the respondents with more males in both hospitals; their mean age was 29.9 ± 6.08 years with modal age of 21-29 years. The educational qualification of almost all the respondents 206 (82.4%) were first degree. The year of practice experience of majority of the respondents was 194 (77.6%) were between 1-10 years; their mean duration of practice experience was 7.8 ± 4.29 years with modal practice/experience of 1-10 years.
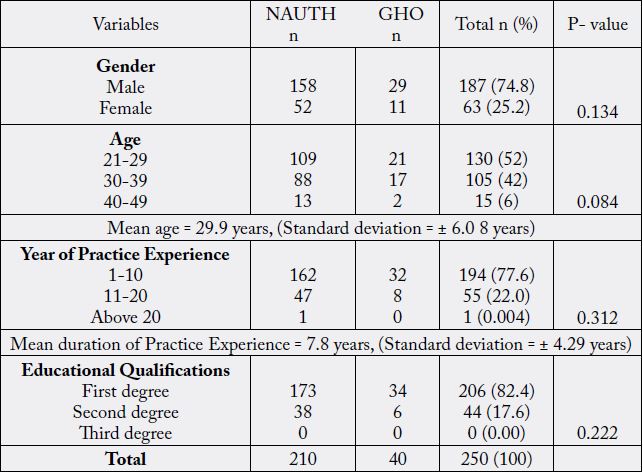
NAUTH - Nnamdi Azikiwe University Teaching Hospital, GHO - General Hospital Onitsha
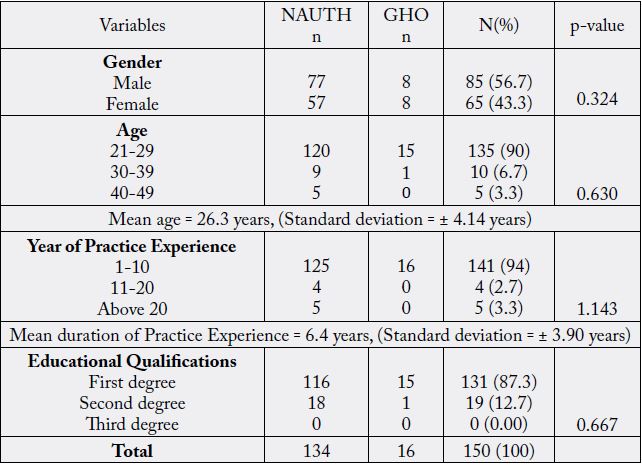
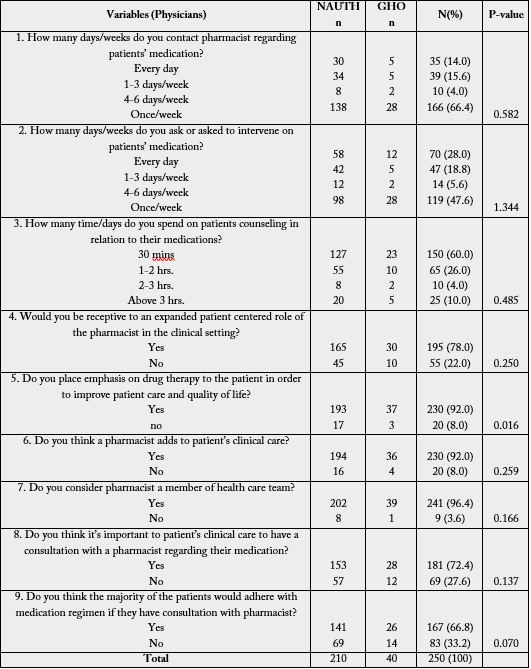
NAUTH – Nnamdi Azikiwe University Teaching Hospital, GHO – General Hospital Onitsha
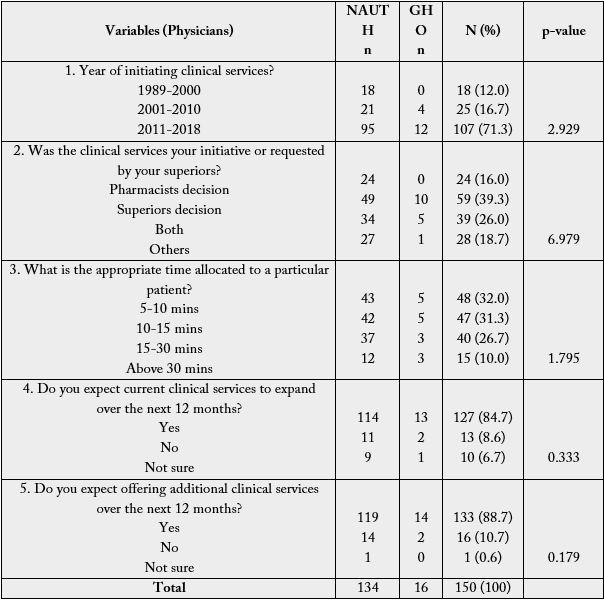
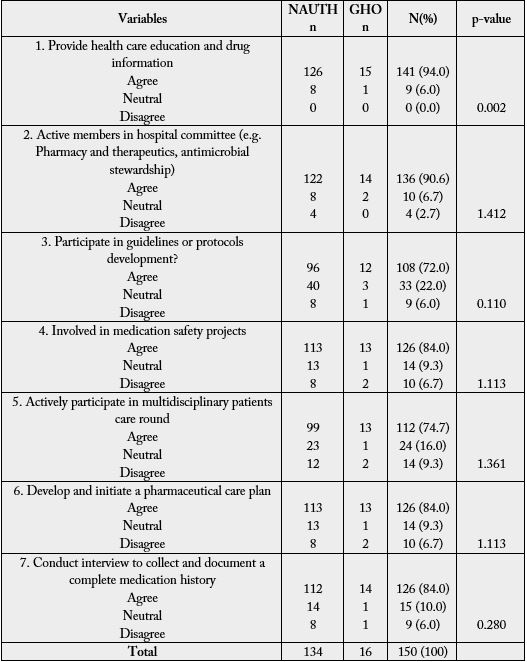
NAUTH – Nnamdi Azikiwe University Teaching Hospital, GHO – General Hospital Onitsha
Discussion
An overall response rate of 80% was recorded. The findings confirmed previous reports of good perspective
and attitude but poor services towards clinical pharmacy practice in both developed and developing countries
[1,2]. This was attributed to lack of formal policy implementation and hence, lack of clinical pharmacist in the
hospitals. According to Lemay, physicians have positive perception of the value and impact of pharmacist to
patient care but poor services to MTM. This was attributed to very little time devoted to MTM by clinical
pharmacist, lack of clinical pharmacy training, lack of therapeutic knowledge and lack of confidence and fear
of new responsibility among some pharmacist which may adversely affect their perception.
That younger physicians and pharmacists showed higher positive attitude towards pharmaceutical care than the older once gives a ray of hope for the future of professional practice in Nigeria. This was reflected in the fact most respondents within the age of 21 - 29 year with 1 - 10 years of experience showed the highest positive attitude towards clinical pharmacy practice in the sub-demographic groups. This is particularly important because they are the determinants of labor force to take charge of pharmaceutical care implementation. The older age groups are usually predominantly for managerial responsibilities. The representation by the both sexes is equally remarkable due to gender implications on policy-related matters [5]. It is indicative that almost all the respondents have good understanding of what clinical pharmacy is with reference to that of Hepler and Strand [2]. This strongly indicates a good knowledge but also needs improved mandatory continuing professional development (MCPD).
A reasonably high number of respondents showed good perspective toward clinical pharmacy practice. This can be seen in table 4 as majority of the physicians indicated that they place emphasis on drug therapy to the patient in order to improve patient care and quality of life (92%); think a pharmacist adds to patients clinical care (92%); consider pharmacist a member of health care team (96.4%); think it’s important to patients clinical care to have a consultation with a pharmacist regarding their medication (72.4%) and they think the majority of the patients would adhere with medication regimen if they have consultation with pharmacist (66.8%). In affirmation to the above, physicians agreed that pharmacists Provide health care education and drug information (94%); are active members in hospital committee (e.g. Pharmacy and therapeutics, antimicrobial stewardship) (90.6%); are involved in medication safety projects (84%); Develop and initiate a pharmaceutical care plan (84%); Conduct interview to collect and document a complete medication history (84%) and actively participate in multidisciplinary patients care round (74.7%). This is in agreement with the roles of pharmacist in pharmaceutical care practice [6].
Clinical pharmacy practice requires a strengthening of the professional relationship between pharmacists and physicians to offer mutual beneficial partnerships in which both share responsibility for patient care. This is indicative in table 4 survey 3 where most physicians (66.4%) indicated that they contact pharmacist regarding patient medication once/week. Therefore, effective pharmacist-physician collaborative working relationship in Nigeria hospitals needs to be improved in order to initiate successful implementation of pharmaceutical care. Counselling is a critical part of pharmaceutical care that cannot be compromised. In table 6 survey 1 and 6, almost all the pharmacist indicated that the provide health care education and drug information (94%); and develop and initiate pharmaceutical care plan (84%). This is in agreement with survey done in Kuwait [7].
The physicians indicated that they allocate 30 minutes to patient counseling while the pharmacist in table 5 surveys 3 allocates just 1-5 minutes to patient care. Lack of time is the most significant obstacle standing against the implementation of clinical pharmacy practice worldwide [8]. Through re-organization of pharmacy staff duties, a certain amount of time could be routinely scheduled for patient care activities. We identified infrequent contact of the respondents with physicians in relation to information about drugs; this may be due to the high competency of the prescribers or their lack of confidence in the pharmacists’ abilities [7].
The non-involvement of majority of respondents, especially the hospital pharmacists, in ward rounds recorded in this study is a major weakness in pharmaceutical services in the study area. Lack of enabling environment, knowledge deficit, inadequate pharmacy personnel, and excess work load among others could be responsible and need to urgently be addressed. Shyness by a number of pharmacists is well known even without much obstacle which calls for improved integration during training at various levels. This study is in agreement with study done in south-west Nigeria [5]. Our respondents’ perspective on ways of improving clinical pharmacy implementation varied and is also an attestation of their readiness to implement it. Topping the list was improved skill acquisition through training. The World Health Organization (WHO) had encouraged special attention to be placed on knowledge, skills, attitudes and behaviours which support pharmaceutical care model right from undergraduate training [9]. Other suggestions were improved relationships with other health care professionals and patients, involvement in ward rounds, political backing, adequate facility provision, better re-numeration and privacy for counseling. Most of these suggestions are commendable and in consonant with WHO and FIP documents on PC related matters [10]. For enhanced relationships with patients, competence, empathy, privacy and good communication skill are paramount.
These are the bedrocks in building enduring therapeutic relationships. For the built relationships to be maintained, regular monitoring and in-process evaluation of the therapy, its production mechanisms and responsible follow-up as well as documentation are mandatory. To achieve and sustain all these meaningfully, continuous quality improvement in capacity building is of absolute necessity. Quality care by nature is collaborative, hence adequate involvement of other health care professionals are paramount particularly the physicians. Practice standards need to be developed [11], and undertake research to assess it in the country, taking each local peculiarity into consideration before satisfactory implementation can be achieved [12,13].
Conclusion
The study revealed that physicians and pharmacist have good perception and attitude towards clinical
pharmacy practice in Nigeria; but have poor services towards clinical pharmacy practice in Nigeria. Improved
partnership with physicians, improved medication therapy management, adequate leadership and resources
and updated legislation from MoH enforcing clinical pharmacists in the circle of care will improve clinical
pharmacy practice in Nigeria. The barriers stemmed from physicians lack of understanding of the expertice
and services of a clinical pharmacists which limits the interaction and collaboration which limits interaction
and collaboration with the physicians. Emphasis should be laid on training and more focus should be paid
to the clinical training and externship programmes because they afford the students and professionals the
opportunity to have real life experiences with patients and improve patient quality of life.
Conflict of Interest: The authors have no conflict to declare
Funding: No fund or grant was received for this study
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!