Biography
Interests
Julián Rondón-Carvajal
Assistant Professor, Department of Internal Medicine, Faculty of Medicine, University of Antioquia. Medellín, Colombia
*Correspondence to: Dr. Julián Rondón-Carvajal, Assistant Professor, Department of Internal Medicine, Faculty of Medicine, University of Antioquia. Medellín, Colombia.
Copyright © 2023 Dr. Julián Rondón-Carvajal. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The micronodular lung pattern is defined radiologically as the presence of multiple nodules of less than 3 mm in size distributed diffusely and bilaterally. Three types of distribution patterns are distinguished in relation to the secondary lung lobule: centrolobular, perilymphatic and random [1]. By accompanying these findings with the appropriate clinical context, the differential diagnosis can be narrowed considerably. From a historical perspective, it has been termed a miliary pattern in the context of tuberculosis results from a massive lymphohematogenous dissemination of Mycobacterium tuberculosis bacilli, characterised by tiny tubercles evident on gross pathology resembling millet seeds in size and appearance. The global HIV/AIDS pandemic and widespread use of immunosuppressive drugs and biologicals have altered the epidemiology of miliary TB [2].
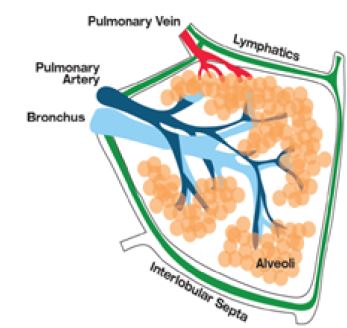
Between 5 and 15 acini, each composed of a terminal bronchiole and airway distal to it represented by alveolar sacs, are enclosed by interlobular septa forming a secondary pulmonary lobule [3]. In these structures, the arteriole and terminal bronchiole are located in the centre, while the veins run along the periphery, i.e. through the interlobular septa. Lymphatics are found mainly in the interlobular septa and visceral pleural surface, as well as in the peribronchovascular interstitium, together with arteries and bronchioles (figure 1). In the absence of involvement of the pleural surfaces by micronodular opacities, it is a centrolobulillar distribution pattern [3,4].
Although classically the randomly distributed miliary pattern on chest X-ray evokes haematogenous dissemination of tuberculosis as primary or post-primary infection (reactivation), it is necessary to rule out concomitant perilymphatic distribution of lesions with septal thickening in addition to mediastinal adenopathies by means of detailed tomographic studies, which allow us to rule out metastasis of solid tumours, cited in order of frequency: breast, thyroid, melanoma and lung cancer [3,5]. (figure 2)

Alende-Castro et al draw attention to the re-emergence of miliary tuberculosis in the setting of increasingly available immunomodulatory therapies. Of a total of 27 patients with this diagnosis, immunosuppression was documented in 51.9% of them, most of whom had pulmonary involvement (65% of cases), with isolation of M. tuberculosis in 88.9% of patients [6].
However, the miliary pulmonary pattern is not synonymous with tuberculosis, as noted. Miliary pattern is an uncommon presentation in lung malignancies and should be considered especially in young females [7]. Miliary nodules can be the manifestation of multiple diseases and the differential diagnosis is broad once encountered in conventional radiographs. Thin-section chest CT is the imaging method of choice for the characterization of pulmonary micronodules and optimizes the diagnostic approach. Interestingly, the development of a miliary pattern of intrapulmonary carcinomatosis has been associated with the presence of EGFR mutations, in particular exon 19 deletions. Patients with lung adenocarcinoma with a miliary pattern and EGFR mutation appear to have a shorter survival time compared with similar patients without miliary pattern, possibly related to the relatively increase tumour burden [8].
Thus, the approach to this radiological finding requires interpretation of each clue, always opting to complement the diagnostic process supported by histopathological and molecular studies. We are in the era of precision medicine, where “pathognomonic” is a paradigm of the past and every challenge is a new opportunity to refine clinical practice.
Acknowledgments
None.
Conflict of Interest
There are no conflicting interests declared by the autor.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!