Biography
Interests
Ali Alyahawi1* & Ali Alkaf2
1Faculty of Medical Sciences, Saba University, Yemen
2Faculty of Pharmacy, Sana’a University, Yemen
*Correspondence to: Dr. Ali Alyahawi, Faculty of Medical Sciences, Saba University, Yemen.
Copyright © 2022 Dr. Ali Alyahawi & Ali Alkaf. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction
For senior people, who are classified as those 65 years of age and older, potentially inappropriate medications
(PIM) are those that may cause more harm than good [1].
One of the challenges of geriatric medicine is prescribing safe, effective medications with few side effects. Many medications which are safe and effective in younger patients (i.e., < 65 years of age) are not the best option or should be avoided in older adults (i.e., ≥ 65 years of age) because of the change in pharmacokinetics (i.e., absorption, distribution, metabolism, and excretion) and pharmacodynamics (the physiologic effects of the drug) with age [2].
According to United Nations estimates, elderly adults are individuals who are 65 years of age or older. The frequency of chronic co morbid health issues brought on by aging’s inevitability is anticipated to rise as the population of older persons rises. Polypharmacy, often defined as the use of five or more medications, is prevalent in adults ages 65 years and older, with 40% taking 5 to 9 medications and 18% taking 10 or more [3].
Adverse drug events might occur as a result of incorrect pharmaceutical prescriptions due to polypharmacy (ADEs). According to studies, ADEs in senior citizens can result in more hospital admissions and emergency room visits, which raises the need for and cost of healthcare [4].
The usage of PIMs is frequently assessed using a variety of scales and criteria, including the explicit Beers criteria for identifying PIMs. It was initially created in 1991. The American Geriatrics Society (AGS) took control of the changes and updates to the criteria in 2011, following Beer’s passing. Since 2012, AGS has updated the criteria every three years [5].
The most recent revision to the Beers Criteria for Potentially Inappropriate Medication Use in Older Adults was released by AGS in January 2019. It is commonly recognized that older individuals who use PIMs can experience poor health effects and have a lower quality of life [6].
The use of PIMs doubles or triples the risk of hospitalization, drug-related issues, and other negative health effects. There are a variety of factors that might lead to inappropriate medicine use. A significant risk factor that raises the likelihood of PIMs prescription is polypharmacy. One danger of polypharmacy is that medical professionals could mistake bad medication reactions for a brand-new illness and attempt to treat it, which is unacceptable [7].
According to a study conducted in one of the main hospitals in the United Arab Emirates, antipsychotics were the most commonly prescribed drugs incorrectly in 2019 with a prevalence of PIMs according to Beer’s criteria of 34.7% [8].
Another study that done in Amman, Jordan, the most common drugs that should be avoided were the prolonged (more than 8 weeks) use of proton pump inhibitors (lansoprazole, pantoprazole, rabeprazole, omeprazole, and esomeprazole) and long-act¬ing sulfonylureas (glimepiride and glyburide) [9].
Older people frequently receive potentially unsuitable prescriptions for drugs, which could have unintended consequences. The goal of the current study, which was the first one carried out in Yemen, was to ascertain the prevalence of polypharmacy, the prevalence of PIMs in older patients, and the main drug-drug and drug-disease interactions.
Methods
The study was conducted in the internal section of a university of science and technology hospital in Sana’a
Yemen. This study was a retrospective cross-sectional study conducted on the elderly patients from April
2020 to November 2020. The sample size was 100 inpatients medical chart. All patients were ≥ 65 years old
of both sexes.
A retrospective cross-sectional study to discover PIMs across older patients during hospital admission and
discharge. The patient’s medical charts were reviewed to obtain their medication lists. Beer’s criteria 2019
are the criteria used to identify PIMs among the elderly patients. Based on these criteria, PIMs are classified
into:
a. Drugs that generally should be avoided in elderly.
b. Drugs to be avoided in combination with specific comorbidities.
c. Drugs to be used with caution.
d. Drug-drug interactions that should be avoided in elderly.
e. Drugs to be avoided or dosage reduced with varying levels of kidney function.
The study reviewed patients’ medical charts extracted from the electronic health record (EHR) database.
to obtain the required data. Collected demographic data include: (a) Age and gender, (b) the diagnosis (c)
creatinine clearance and (d) the list of admitted and discharged medications.
Statistical analysis was done by SPSS software version 26.0 by using Pearson’s Chi-square test. P-value of less
than 0.05 was considered significant. Categorical variables were presented as frequencies and percentages.
Full ethical clearance was obtained from the qualified authorities who approved the study design. The study
protocol was approved by the Ethics Committee of Saba University and hospital of university sciences and
technology.
Results
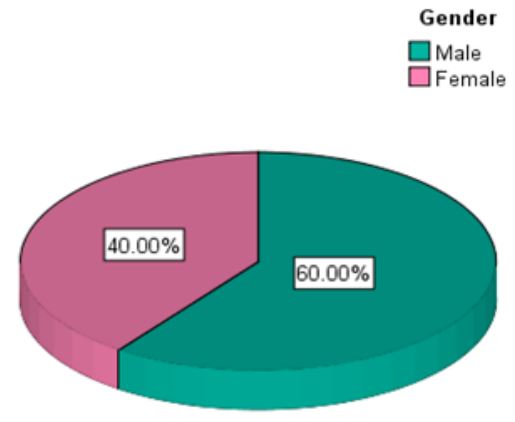
During the period of this study a total of 100 in-patients records were reviewed, among which majority were
males and the remaining were female [Fig. 1].
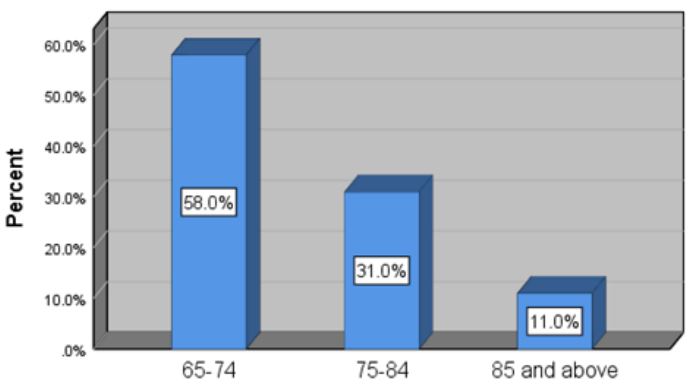
It was found that age of the patients involved varied from 65 to 98 years. The age groups were categorized
into three: 65-74 years, 75-84 years and 85 years and above [Fig. 2].
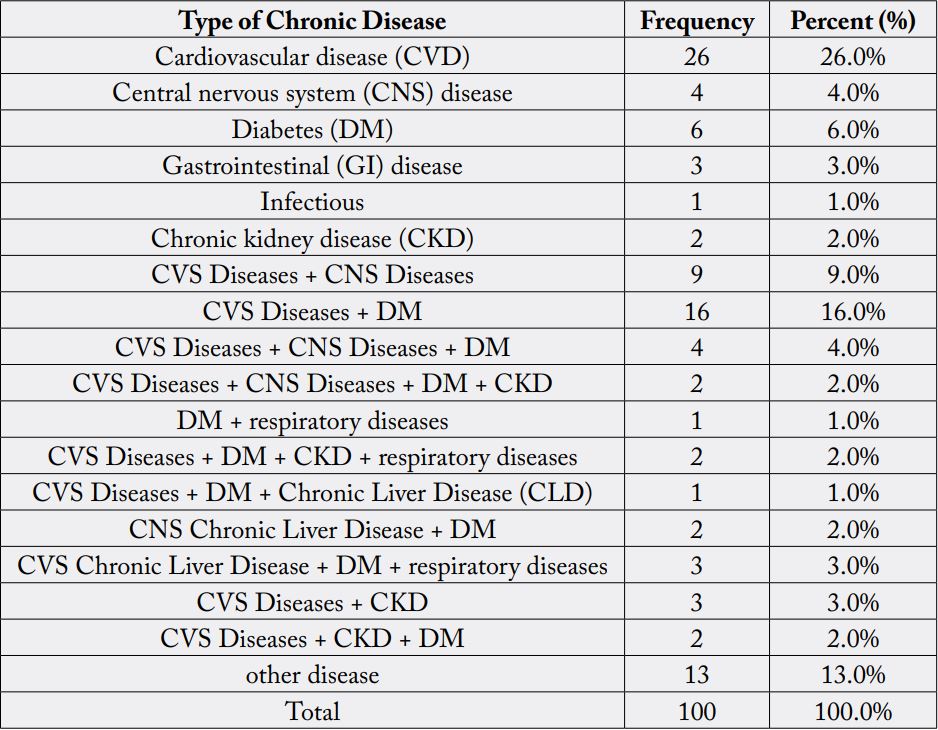
According to the study results, the major morbidity pattern was cardiovascular disease 26%, distributed
between hypertension, ischemic heart disease and heart failure which were the most. Also 16% of the
morbidity was cardiovascular disease with diabetes mellitus together [Table 1].
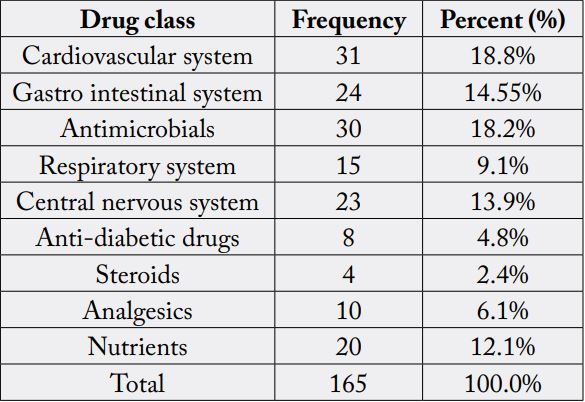
Form 165 drugs were prescribed in the current study, 18.79% were drugs using for cardiovascular system
followed by antimicrobials (18.18%) and (14.55%) used for gastrointestinal system (GI), and the other
drugs distributed between other systems as mentioned in [Table 2].
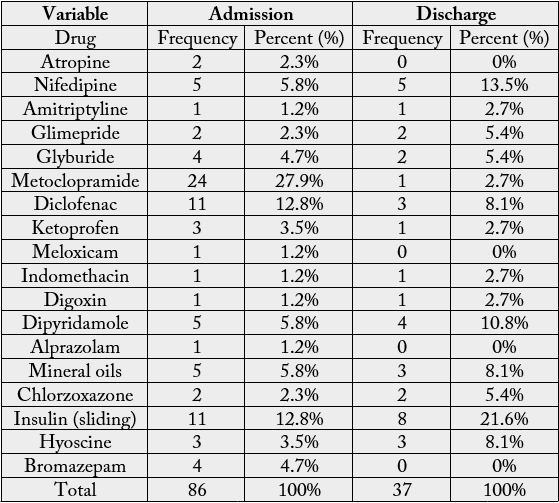
On application of beers criteria 2019 to all study prescriptions, it had been found that 18 drugs out of 165
drugs were drugs that generally should be avoided in older adults [Table 3].
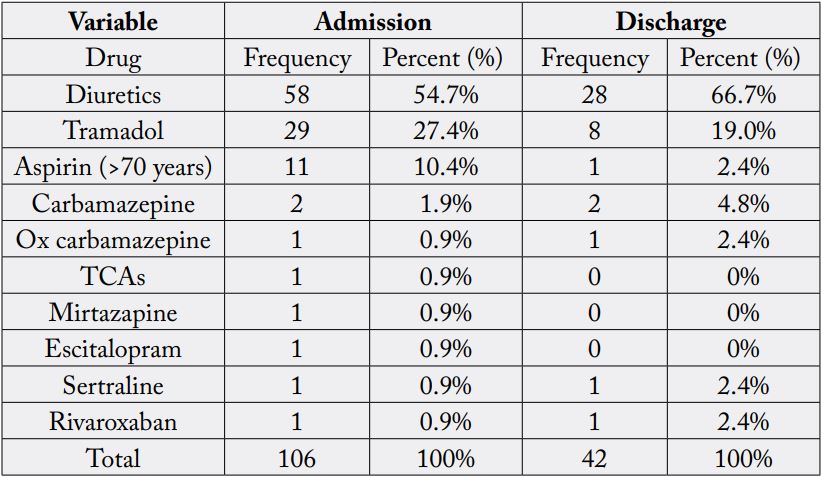
For drugs that should be used with caution the number was 10 (drugs and drug classes) that should be used with caution when prescribe to older adults [Table 4].
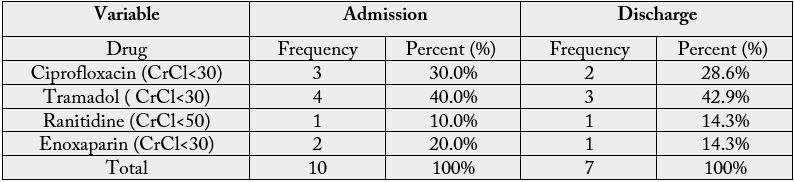
Drugs to be avoided or dosage reduced with varying levels of kidney function out of 165 drugs were (4
drugs) on admission and on discharge [Table 5].
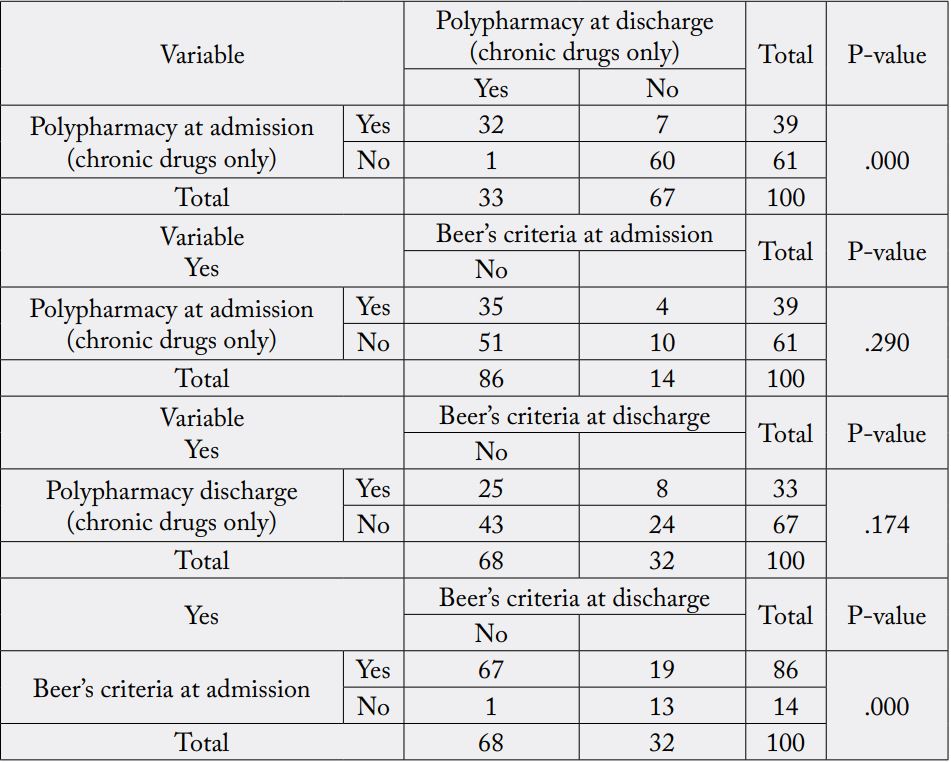
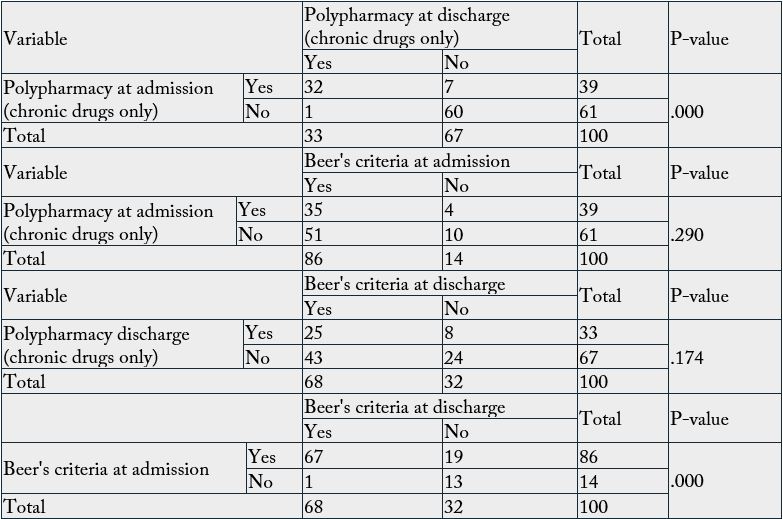
For polypharmacy on admission (39%) of patients had polypharmacy and (61%) with no polypharmacy.
On contrast, the ratio of polypharmacy in discharge were (33%) and (67%) had not polypharmacy and the
relationship between admission and discharge was with statistically significant (P-value < 0.001). There was
no significant statistically relationship between the number of Beers criteria and prevalence of polypharmacy
[Table 6]. The relationship between Beer’s criteria at admission and discharge was with statistically significant
(P-value < 0.001).
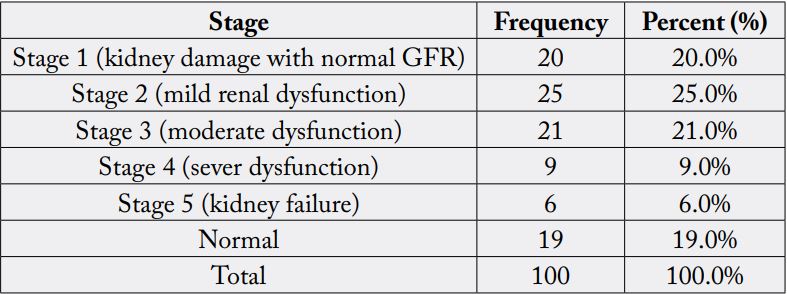
Based on GFR category, 100 inpatients of both sexes were screened for chronic kidney disease stages [Table 7].
The study results also revealed that 54 (54 %) of patients had at least one major drug-drug interactions
on admission and 19 (19 %) on discharge. On other hand, 46 (46%) of patients had no major drug-drug
interactions on admission and 81 (81%) on discharge and the relationship between admission and discharge
was with statistically significant (P-value < 0.001) [Table 8].
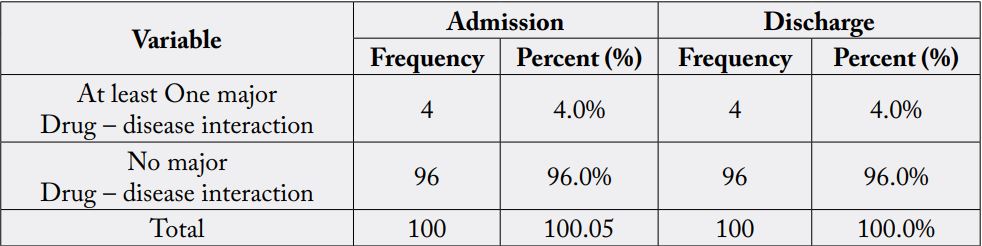
Regarding drug-disease interactions, 4 (4%) of patients had at least one major drug-disease interaction on
admission and discharge [Table 9].
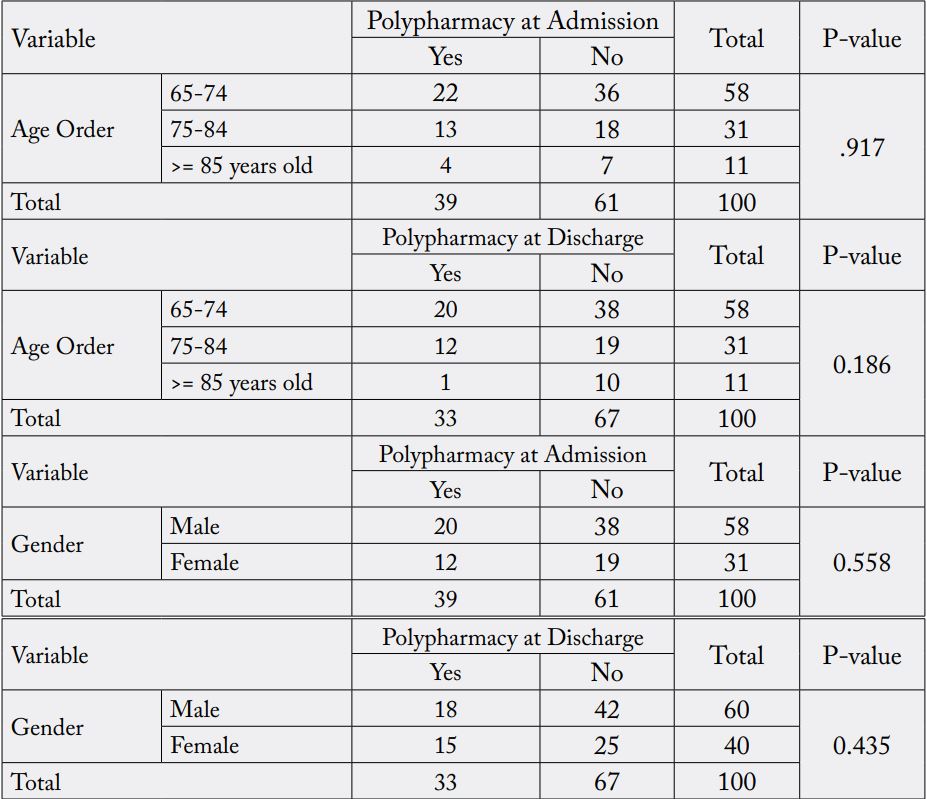
In admission, 22, 13, and 4 of patients had polypharmacy aged 65-74, 75-84, and >= 85 years old respectively and 36, 18, and 7 of patients with no polypharmacy. On contrast, the frequency of polypharmacy in discharge were 20, 12, and 1 aged 65-74, 75-84, and >= 85 years old respectively, while 38, 19, and 10 of patients had not polypharmacy. The relationship between polypharmacy in admission and discharge with age order was statistically non-significant (P-value = 0.917, 0.186). There was no significant statistically relationship between the gender and polypharmacy in admission and discharge (P-value = 0.558, 0.435) [Table 10].
Moreover, the study results showed that the relationship between the age order and Major drug-drug interaction either in admission or in discharge was statistically non-significant (P-value = 0.173, 0.203) [Table 11].

Discussion
This is the first Yemeni study and one of the few international studies that evaluates PIMs use in geriatrics
based on the latest version of AGS Beers Criteria (2019 AGS Beers Criteria). Toxic effects of medications and
drug-related problems can have profound medical and safety consequences for older adults and economically
affect the health-care system. In this study, the presence of certain chronic conditions in older patients
predicted the increased chance of PIMs use. The most common morbidity resulting in hospitalization was
diabetes, HTN, IHD, HF and CKD [Table 5]. Multiple studies have demonstrated a significant association
between PIMs use and CVD, DM, and increase number of chronic diseases [10].
Older age, polypharmacy, having multiple prescribers’ physicians, and having poor health status are more likely to be associated with PIMs use. Moreover, certain chronic conditions have also been associated with a higher risk of PIMs use compared with older adults who don’t have these chronic conditions.
The association between PIMs use and different predictors such as the presence of certain chronic conditions and polypharmacy use could be an indicator of inappropriate medication management for these conditions in such older population [11].
Majority of drugs prescribed to the study population were those acting on cardiovascular system including the (CVS) drugs, ACEIs, ARBs, CCBs, Diuretics and beta blockers were the most frequently prescribed drugs. Antimicrobials as ceftriaxone and cefuroxime were most commonly used. PPIs and antiemetics were the most GIT drugs that were prescribed. A study conducted in Brazil found that also cardiovascular and psychiatric disorders were the factors related to PIMs [12].
Results from this study showed a high prevalence of PIM prescribing among Yemeni elderly patients (86% at admission and 68% at discharge) according to the most updated version of the AGS Beers Criteria (2019). This finding is consistent with pervious published study in Jordan [13].
Another study conducted in Brazil found that 50% of community-dwelling elderly patients were prescribed at least one PIM according to the 2015 update of AGS Beers Criteria [14].
The vast majority of PIMs identified in the present study were drugs to be used with caution (64%). This finding is similar with recent study in Jordan and Qatar where 69% and 65%, respectively, of PIMs were drugs to be used with caution [15].
The prevalence of PIMs to be avoided for older adults which was 18 drugs, metoclopramide was the most prescribed with a frequency of (24 prescriptions) followed by Diclofenac and insulin sliding scale with frequency of 11 prescriptions for each one.
This is inconsistent with other study findings, where central nervous system (CNS) drugs and benzodiazepines have been found to be the most prescribed PIMs (Wang et al., 2019) [16].
Glimepiride, glyburide and insulin (sliding scale) are drugs that have been included in updated Beer’s criteria 2019 as PIMs because they have higher risk of severe prolonged hypoglycemia in older adults. Metoclopramide can cause extrapyramidal effects, including tardive dyskinesia; risk may be greater in frail older adults and with prolonged exposure. The rational of NSAIDS as (Diclofenac, Ketoprofen and meloxicam) to be avoided in older adult is that all increase risk of gastrointestinal bleeding or peptic ulcer disease. For digoxin if used for atrial fibrillation it should not be used for first line because there are safer and more effective alternatives for rate control.
Dipyridamole can cause orthostatic hypotension and mineral oils are potential for aspiration and they should be avoided for those reasons. Chlorzoxazone is muscle relaxant and most muscle relaxant are poorly tolerated by older adults because some have anticholinergic adverse effects, sedation, increased risk of fracture, also Hyoscine cause the same effects. Another drug class that should be avoided in older adults that we found in our study was Benzodiazepine that all of them increase risk of cognitive impairment, delirium, falls and fractures.
For PIMs that’s should be used with caution were (10 drugs and drug classes), which diuretics and tramadol had the majority of prescribed drugs.
Diuretics and Tramadol may exacerbate or cause SIADH or hyponatremia; monitor sodium level closely when starting or changing dosages in older adults. Aspirin (>70 years) has Risk of major bleeding from aspirin increases markedly in older age. Several studies suggest lack of net benefit when used for primary prevention in older adult with cardiovascular risk factors, but evidence is not conclusive. Aspirin is generally indicated for secondary prevention in older adults with established cardiovascular disease. Rivaroxaban increases risk of GI bleeding so it should be used with caution.
Carbamazepine, oxcarbamazepin, TCAs, mirtazapine, Escitalopram and sertraline may exacerbate or cause SIADH or hyponatremia, monitor sodium level closely when starting or changing dosages in older adults is important.
PIMs that’s should be avoided or dosage reduced with varying levels of kidney function according to GFR that was calculated using MDRD equation, ciprofloxacin and tramadol had the majority of prescribed drugs.
According to a retrospective charts review study of older patients ≥65 years in Tawam hospital, the percent of drugs that should be dose adjusted or avoided based on kidney function was 11.4% and the most common drugs inappropriately prescribed in this category were anticoagulants (40%) [17].
In a previous study done in Jordan, prescribing gabapentin when CrCl <60 ml/min was responsible for the majority of PIMs.
Polypharmacy increases the incidence of potentially inappropriate medication (PIM) use as defined by the American Geriatrics Society (AGS). The most likely factor associated with PIMs use in the previous studies was polypharmacy [18].
Surprisingly, we found that polypharmacy was observed only in 39% at discharge and 33% during admission of all study cases. In our study, the frequency of PIM was not associated with polypharmacy.
The polypharmacy use in our study population can be attributed to the higher rate of multiple chronic conditions (i.e., two or more chronic conditions), in which they may need to take many medications to control their chronic conditions or to prevent complications associated with certain chronic conditions [19].
The majority of interactions found between Cephalosporins (ceftriaxone, cefuroxime) with heparin or enoxaparin that Cephalosporins will increase the levels or effect of heparin by anticoagulation so avoid or use alternative drug. Followed by interactions between fluoroquinolones with ondansetron that both increase QTc interval. Another interaction was between NSAIDs and ACEIs that coadministration may result in a significant decrease in renal function. Sodium bicarbonate with moxifloxacin is another interaction that sodium bicarbonate decreases levels of moxifloxacin by inhibiting GI absorption. This interaction applies only to oral form of both agents so avoid or use alternative drug or separate by 2 hours. Omeprazole decreases effects of clopidogrel by affecting hepatic enzyme CYP2C19 metabolism so clopidogrel efficacy may be reduced. More and more drugs interaction had been found in this study and needs more focusing and care when prescribing drugs to patients [20].
In the drug-disease interaction-based Beer Criteria 2019, the heart failure with NSAIDs was reported and the rational of that use is potential to promote fluid retention and/or exacerbate heart failure. Also, the use of opioid in patients with history of falls or fractures may cause ataxia, impaired psychomotor function, syncope and additional falls so avoid opioids except for pain management in the setting of severe acute pain (e.g., recent fractures or joint replacement) [21].
The role of health care providers should expand in order to take the necessary precautions when managing older patient’s conditions to avoid inappropriate medications prescribing, adverse events and other misadventures associated with older patients. Additionally, pharmacists can play a major role in improving the appropriateness of medications use by the recommendation for either medication discontinuation, medication review, the clinical application of tools to assess PIMs such as beers criteria, or other tools to identify older patients at risk of unnecessary use of PIMs [22].
The strength of this study is that it is the first study conducted in Yemen to assess the prevalence of PIMs among older patients during admission and discharge. The study is subjected to some limitations. One of the study limitations is that not all medications of beers criteria are available in the hospital formulary. Also, this study is done over one hospital only, one department and the study duration was short so, the results may be not representative of all geriatrics in Yemen. This study only used Beer’s criteria as the tool for detecting PIMs use. Comparing between Beers criteria and other validated tools such as STOPP/START criteria in detecting PIMs use may be suggested. The reason that STOPP/START criteria was not used in the evaluation is the lack of sufficient information about patient history because of incomplete documentation.
Conclusion & Recommendations
This study showed a high prevalence of PIMs that should be avoided or used with caution among older
patients. Polypharmacy and chronic conditions were predictors for increased use of PIMs among older
patients. Increase the knowledge about PIMs and their potential side effects among patients and healthcare
providers is warranted.
According to the results obtained in this work, the following recommendations are proposed:
o Further studies should be done on all departments of Yemen’s hospitals.
o Physicians should be aware and given more attention during prescribing of drugs.
o Clinical pharmacists should be present in all branches of the hospitals in order to correct such errors.
o All geriatric’s medications should be subjected to Beer’s criteria to avoid inappropriate use of them.
Principle Investigator Statement
I certify that the information provided in this article is accurate. I have ultimate responsibility for the
conduct of the study, the ethical performance, and strict adherence to the study protocol.
Conflict of Interest
The authors have no conflicts of interest to declare.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!