Biography
Interests
Lu Shoulong1*, Tang Ying2 & Ying Qi1
1Department of Neurosurgery, Shanghai Naval Hospital, China
2Laboratory of Animal Experiment and Medical Information, Shanghai Naval Medical Research Institute, China
*Correspondence to: Dr. Lu Shoulong, Department of Neurosurgery, Shanghai Naval Hospital, China.
Copyright © 2022 Dr. Lu Shoulong, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Semi Cranial Open Decompression (SCOD) technology is a new neurosurgical method, which is mainly suitable for patients with severe or extremely severe stroke. The implementation of this technology can save the lives of some patients and reduce the disability rate.
Nowadays, the incidence rate, disability rate and mortality rate of severe and extremely severe stroke are high. Based on many years of clinical experience and animal experiments, and combined with the initial practice of open decompression for severe traumatic brain injury, the author creatively proposes to SCOD technology, So as to save the lives of some patients and reduce the disability rate.
The main methods are to open the cerebrospinal fluid circulation, relieve the brain hernia, open the decompression wound, etc., so that the patient can successfully overcome the brain edema and brain swelling, which is expected to reduce the mortality and disability rate.
Our study demonstrates the Semi Cranial Open Decompression technology will have a nice application vista.
Introduction
SCOD technology is a new surgical method in Department of neurosurgery. It is another innovation [1]
on the basis of Open Cerebral Decompression (OCD). The incidence rate of death (high mortality rate and
disability rate) in the face of stroke (hypertensive cerebral hemorrhage, large area cerebral infarction) has
remained high for a long time, resulting in serious family and social burden [2]. People are thinking hard,
most mild and moderate patients can be relieved or cured, for severe or extremely severe patients, such as
cerebral hernia, high intracranial pressure and deep coma, the probability of death is very high. To save the
lives of these patients, SCOD technology is an effective option Surgical indications.
Indications
a. Stroke, deep coma, GCS index 3-5 points.
b. The midline structure of the brain moves laterally by more than 5mm or the intracranial pressure is greater
than 30mmHg.
c. Cerebral hernia has occurred
Steps
Routine general anesthesia preparation, endotracheal intubation or tracheotomy, and hyperventilation
can be given if the intracranial pressure is too high. Open two venous channels, including one deep vein.
Preoperative blood pressure should be controlled at systolic blood pressure of 100-130mmHg and diastolic
blood pressure of 60-89mmHg [3].
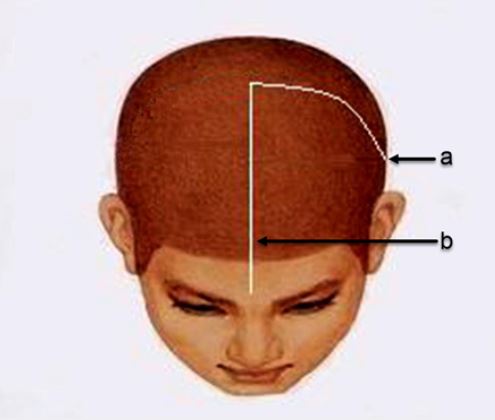
The head incision is shown in (Fig. 1). The skull flap is adapted to the scalp incision and replanted after indwelling.
After dural incision, release the brain hernia as soon as possible, relieve the midbrain compression, open the lumbar cistern drainage tube and connect the closed drainage bag [1]. Patients with cerebral infarction cut the dura mater and covered the exposed brain tissue with meningeal repair material to protect the brain tissue. Patients with intracerebral hemorrhage should try to remove the hematoma, pay attention to protecting the hematoma wall, gently attract the hematoma, electrocoagulate the bleeding point with weak current, and cover the exposed brain tissue with meningeal repair material [4] after proper hemostasis. So far, the wound [5] was covered with brain cotton soaked with antibiotic solution. A porous drainage tube was placed on the brain cotton and connected with a closed drainage bag. Another small plastic tube was placed to drip antibiotic solution, and the scalp flap was without suture. Aseptic dressing Bandage package of operating field.
Key Points of Postoperative Treatment
The head plastic tube and intravenous drip of antibiotic solution to prevent intracranial and other parts of
the body from infection. The brain wound drainage fluid is routinely tested and cultured every day to adjust
the pertinence of antibiotics. Usually, the head drip tube and drainage tube are removed in 5-7 days, and
then enter the operating room to clean the brain wound, suture the dura mater, reset the skull and suture the
scalp. The patient was admitted to a strictly disinfected neurosurgical isolation ward.
Discuss
The main purpose of implementing SCOD is to make the affected side of the brain survive the severe
brain edema and brain swelling caused by hemorrhage or ischemia. The latter two are the most important
causes of early death of patients. Animal experiments demonstrate that open decompression has obvious
advantages over closed decompression in reducing postoperative brain edema and brain swelling [5]. In
addition, combined with lumbar cistern drainage, it is further conducive to the regression of brain edema
and brain swelling.
Open brain decompression will inevitably face the problem of possible intracranial infection. Through the whole process of aseptic operation, covering with sterile cotton pad under the scalp and continuous infusion of antibiotic solution after operation, it will help to avoid intracranial infection [6]. Of course, allowing patients to stay in a strictly disinfected neurosurgical intensive care isolation ward provides another layer of protection against intracranial infection. In this way, the probability of intracranial infection is very low.
Relieving the compression of the midbrain caused by cerebral hernia and opening the cerebrospinal fluid circulation is another key to the success of the operation. Only when the basal cistern is unobstructed, the lumbar cistern drainage tube can be opened for drainage [7], so as to reduce the intracranial pressure. Bloody cerebrospinal fluid can also be drawn out to reduce or avoid extensive arachnoid adhesion and obstructive hydrocephalus [8].
Conclusion
The incidence rate, mortality and disability rate of stroke (hypertensive cerebral hemorrhage, massive cerebral
infarction) are high, which seriously afflicts the family of patients and increases the social burden [9].
SCOD technology is of great value in the treatment of severe and extremely severe stroke. It can significantly reduce the degree of brain edema and brain swelling, shorten the time course of brain edema and brain swelling, and gradually popularize and apply this technology, which can save the lives of some patients and reduce the disability rate.
Bibliography

Hi!
We're here to answer your questions!
Send us a message via Whatsapp, and we'll reply the moment we're available!